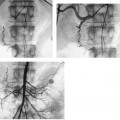
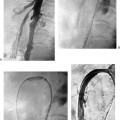
CASE 48 A 55-year-old male with a history of end-stage renal disease requiring multiple hemodialysis catheters and arteriovenous shunts presented with marked right upper extremity swelling. He had a current right upper arm arteriovenous fistula. Figure 48-1 Selected subclavian venography performed by catheterization of a right arm arteriovenous hemodialysis fistula shows a stenosis of the right brachiocephalic vein. Pressure gradient measured 8 mm Hg across this stenosis. Conventional subclavian venography performed by catheterization of the right arm fistula showed a stenosis of the right brachiocephalic vein (Fig. 48-1). Pressure gradient measured 8 mm Hg across this stenosis. Central venous obstruction caused by long-term hemodialysis venous access. The fistula was initially accessed for venography using a Micropuncture system (Cook, Bloomington, Indiana), and a 5-French (F) multipurpose catheter and standard guidewire were advanced across the stenosis of the right brachiocephalic vein. A 9F vascular sheath was placed in the fistula. A 12-mm diameter, 2-cm long Wallstent (Boston Scientific, Natick, Massachusetts) was deployed and angioplastied using a BlueMax balloon catheter (Boston Scientific, Natick, Massachusetts) with a diameter of 12 mm. Follow-up venography through the sidearm of the vascular sheath showed wide patency (Fig. 48-2) across the thoracic inlet. Figure 48-2 Venography following placement of a Wallstent (12 mm diameter, 2 cm long; Boston Scientific, Natick, Massachusetts) across the brachiocephalic vein and angioplasty using a balloon catheter with a diameter of 12 mm. Superior vena cava (SVC) syndrome refers to central venous obstruction with inadequate formation of venous collateral pathways resulting in clinical symptoms of swelling of the upper extremities, face, neck and chest, as well as unsightly dilatation of subcutaneous chest veins. In severe cases, swelling may result in airway compromise. SVC syndrome may result from obstruction of the brachiocephalic veins or SVC, and may result from benign or malignant causes.
Clinical Presentation

Radiologic Studies
Diagnosis
Treatment
Equipment
Discussion
Background
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree