CASE 51
A 32-year-old female on hemodialysis for the previous 2 years presented with a polytetrafluoroethylene (PTFE) graft without a pulse or thrill. We discuss the therapeutic options and how a percutaneous graft declotting procedure is performed.
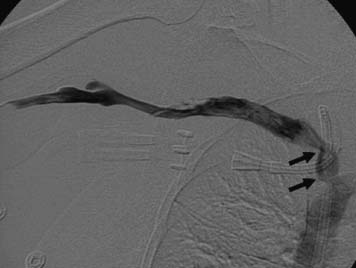
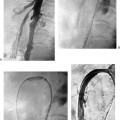
Figure 51-1 A 32-year-old female with renal failure and clotted arteriovenous graft. A central venogram performed after crossing the venous anastomosis shows mild stenoses (arrows) without significant collateral flow. A right internal jugular central venous catheter was placed for emergent dialysis prior to elective declotting.
None.
Thrombosed dialysis graft.
The procedure is divided into access, thrombolytic infusion and anticoagulant administration with heparin, mechanical adjunct to chemical thrombolysis, and treatment of underlying lesions. A stepby-step description of the procedure is detailed below. Note that a wide variety of techniques are used to treat thrombosed grafts. The same outline can be used for declotting of arteriovenous fistulae and femoral synthetic grafts.
- Venopuncture of graft with needle directed toward venous anastomosis and cross venous anastomosis. Inability to cross the anastomosis is the most common cause of declotting failure. If the anastomosis cannot be crossed, the procedure is terminated.
- Perform central venogram (Fig. 51-1). If central vein occlusion is present, treat this lesion prior to declotting. For central vein stenosis or occlusion that cannot be crossed and/or treated, consider aborting the procedure at this point, unless there are adequate collaterals.
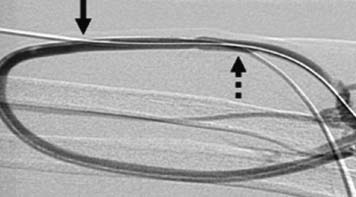
Figure 51-2 Shuntogram of the arteriovenous graft after thrombolysis shows restored flow in the graft with reflux into the native artery and forward flow in the outflow veins. The graft was accessed in a cross-configuration fashion. Arrows point to the sites of puncture (solid arrow to venous limb access; dashed arrow to arterial limb access).
- Administer 3000 to 5000 IU heparin intravenously.
- Administer lytic agent (2–4 mg recombinant tissue plasminogen activator [alteplase] or 1 unit recombinant plasminogen activator [reteplase] into graft.
- Access graft in venous limb about 5 cm central to the first puncture with needle directed toward arterial anastomosis. This will result in a cross-catheter configuration (Fig. 51-2).
- Cross arterial anastomosis.
- Perform inflow arteriogram. Note patency of distal arteries and size and position of inflow feeding artery. If there is inflow stenosis, this should be treated with angioplasty.
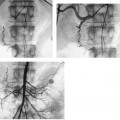
- Perform outflow venography and dilate all venous lesions. Macerate any clot still present on the venous side of the graft (Fig. 51-3).
- Pull arterial plug.
- Macerate intragraft clots if present.
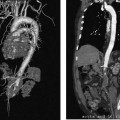
- Treat stenoses with angioplasty and when necessary with stenting. Equivocal lesions after angioplasty should be further evaluated with pull-back pressure measurement (a gradient of > 10 mm Hg is considered significant) and further treatment such as a larger balloon or cutting balloon should be considered (Fig. 51-4).
Micropuncture set
0.035” conventional and hydrophilic guidewires
High-pressure angioplasty balloons (5 to 12 mm in diameter)