
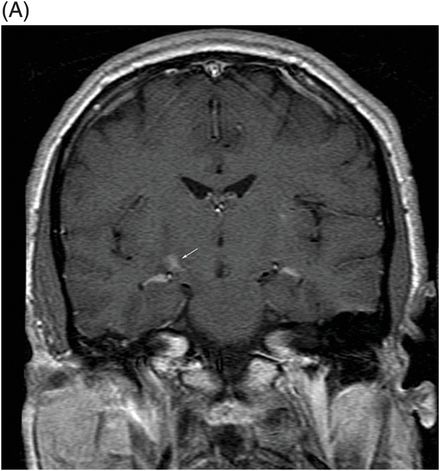
(A) Postcontrast coronal T1WI through the cerebral peduncles and (B) Postcontrast axial T1WI through the cerebral peduncles.

Neuro-Behçet Disease
Primary Diagnosis
Neuro-Behçet disease
Differential Diagnoses
Central nervous system vasculitis
Multiple sclerosis
Acute disseminated encephalomyelitis (ADEM)
Infiltrating primary CNS neoplasm
Imaging Findings
Fig. 53.1: (A) Axial FLAIR image through the level of the optic tract and (B) cerebral peduncle demonstrates patchy areas of FLAIR abnormality in the right mesodiencephalic junction (involving the posterolateral aspect of the right cerebral peduncle and adjoining brain tissue extending superiorly to the thalami regions). It was noted that the left side was normal. There was no abnormal FLAIR signal in the visualized area of the periventricular white matter. Fig. 53.2: (A) Postcontrast coronal T1WI and (B) axial sequences demonstrate subtle enhancement (arrow) within the area of FLAIR abnormality.
Discussion
Multi-joint arthritis and recurrent oral and genital ulcers is suggestive of a rheumatologic condition. Predominant motor involvement with typical mesodiencephalic junction abnormality on MRI is consistent with neuro-Behçet disease (NBD).
Primary CNS vasculitis is exclusively a disease of the CNS. The presence of extra-neurologic manifestations rules out the possibility of primary CNS angiitis. The presenting clinical features including oro-genital ulcers are suggestive of Behçet disease (BD) rather than other causes of systemic vasculitis. The presence of extra-CNS manifestations rules out multiple sclerosis, ADEM, and CNS neoplasm.
Behçet disease is an idiopathic, relapsing, multisystem inflammatory disease of the vascular system that typically presents in the third or fourth decade of life. The disease is prevalent in Asia and Mediterranean countries. The highest prevalence of BD, 80–370 cases per 100,000 persons, is in Turkey. The disease is rare in North America, as compared to the more prevalent areas. In areas with high prevalence of the disease, there is no gender predilection. The common clinical manifestations include recurrent painful mucocutaneous ulcerations that predominantly involve the oral cavity and genital areas. Other common manifestations of BD include episodic bilateral uveitis, venous occlusive diseases such as obstruction of superior and inferior vena cava or deep vein thrombosis, vasculitis involving medium- to large-sized arteries, including the pulmonary artery, and asymmetric arthritis. The kidneys, heart, and gastrointestinal system can also invariably be involved in patients with BD. The international BD study group criteria for diagnosing BD include recurrent oral ulceration and two of the following four symptoms: recurrent genital ulcers, eye lesions (anterior or posterior uveitis or retinal vasculitis), skin lesions (erythema nodosum, pseudofolliculitis, papulopustular lesions, or acneiform nodules), and a positive pathergy test.
The literature variably documents the frequency of neurologic involvement in patients with BD, i.e., NBD, reporting incidence as low as 1.35% to as high as 59%. Generally, NBD is more common in men than women. The average age of onset of NBD is between 20 and 40 years. Diagnosis of NBD should be made carefully, as similar pathologic imaging features are more prevalent in elderly patients. Neurologic manifestations commonly develop several years after the onset of other systemic features; however, NBD may be the presenting symptom in up to 6% of patients, similar to this patient. Central nervous system involvement can be either parenchymal or non-parenchymal. Parenchymal NBD is usually a result of intense meningoencephalitis with penetrating inflammatory infiltration within the brainstem, thalamus, basal ganglia, and subcortical white matter. Although inflammatory infiltrates can occur in small-sized brain blood vessels, fibrinoid necrosis is not seen, differentiating BD from other cerebral vasculitis conditions. Non-parenchymal involvement, sometimes referred to as vasculo-NBD, presents with CNS vascular involvement, and may include dural venous thrombosis, intracranial hypertension, or intracranial aneurysms.
Magnetic resonance is the imaging study of choice to evaluate NBD. Unilateral T2 hyperintensity in the mesodiencephalic junction with variable degree of swelling with or without enhancement is the characteristic imaging finding in parenchymal NBD. If enhancement is present, it is usually patchy. Bilateral involvement is less common than unilateral involvement. Diffusion restriction is not a feature; however, in acute lesions, diffusion restriction may be present. In patients with severe CNS involvement, T2 hyperintense lesions can also be seen in the subcortical white matter of the frontal and temporal lobes, as well as in the hypothalamus. In the chronic phase, there may be lesions present in the supratentorial brain that are difficult to differentiate from multiple sclerosis lesions, based on imaging alone. As BD predominantly targets the vascular structures, intracranial vascular complications are also common, such as dural venous thrombosis, large arterial distribution infarction, and aneurysm involving the larger-sized intracranial arteries. Although rare, intracranial arterial dissection has also been described as a manifestation of NBD.
Cerebrospinal fluid studies typically demonstrate pleocytosis and elevated protein. Opening pressure is elevated in patients with intracranial hypertension. Cerebrospinal fluid is negative for elevated IgG index and oligoclonal bands. Neuro-Behçet disease is typically treated with immune suppressive agents with or without tumor necrosis factor (TNF) antagonists depending upon the nature of the disease, and severity of involvement response to steroids.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








