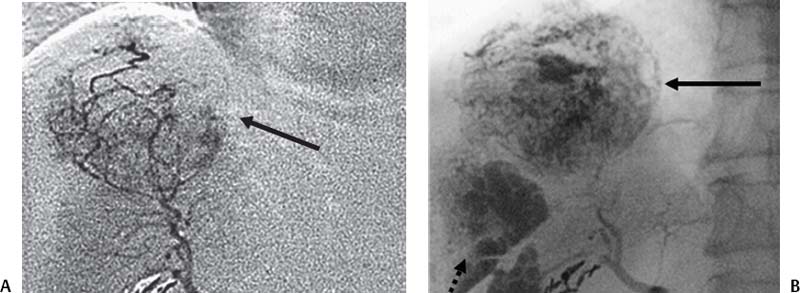
CASE 60 A 62-year-old female with hepatitis C cirrhosis had an elevated α fetoprotein level discovered on a screening blood test. A CT scan was then obtained. Figure 60-1 A 62-year-old female with cirrhosis. (A) Axial image from contrast-enhanced CT shows a shrunken, cirrhotic liver with a large mass (arrow) at the dome. There is also ascites. (B) Coronal reconstruction shows the mass (arrow) pushing on the diaphragm. CT scans showed a 6.5-cm enhancing mass in the dome of the liver (Fig. 60-1). Ultrasound (not shown) showed no definite mass lesion in the background of heterogenous echogenic liver parenchyma. Hepatocellular carcinoma. 5F vascular sheath 5F Cobra, RC-1, RIM, VS-1 catheters Standard 0.035” guidewire 3F microcatheter 0.014” microwire 500- to 700-micron polyvinyl alcohol particles Contrast material Chemotherapeutic agents with syringes and stopcocks compatible with agents The right common femoral artery was catheterized, and a pigtail catheter was advanced into the abdominal aorta. Angiography of the abdominal aorta was performed. The pigtail catheter was exchanged for a 5-French (F) Cobra glide catheter (Boston Scientific, Natick, Massachusetts). The superior mesenteric artery was selected. Selective superior mesenteric arteriogram was performed to evaluate for variant hepatic anatomy (such as a replaced right hepatic artery). Portal vein patency was assessed by carrying the angiogram to the portal venous phase. Celiac trunk arteriogram was performed to delineate hepatic arterial anatomy. The proper hepatic artery was selected, and hepatic arteriogram was performed to identify the arterial supply to the tumor. The arteries supplying the tumor were selected with a microcatheter (Renegade; Boston Scientific, Natick, Massachusetts), using the coaxial technique (Fig. 60-2). Chemoembolization was then performed. A mixture of chemotherapeutic agents (doxorubicin, mitomycin-C, cisplatin) emulsified with Ethiodol (Savage Laboratories, Melville, New York) was infused, followed by embolization with polyvinyl alcohol particles and Gelfoam (Pharmacia and Upjohn, Kalamazoo, Michigan). See Table 60-1. Primary and metastatic malignancies of the liver remain a challenging problem for clinical oncology. Most hepatic malignancies are not resectable. When untreated, patient prognosis is dismal and the response rate to conventional, mostly intravenous chemotherapy, is disappointing. Chemoembolization is performed by delivering a concentrated dose of chemotherapeutic agents directly into the arteries supplying the tumor via an intra-arterial catheter. This is followed by embolization. Ethiodol (Savage Laboratories, Melville, New York) is used in the emulsion with other chemotherapeutic agents as it is selectively taken up and retained by solid tumors, allowing slow targeted release of agents. The basis of chemoembolization is that tumors derive blood supply primarily from the hepatic artery, whereas the normal liver blood supply is mostly from the portal vein. Thus, occlusion of the segmental hepatic arteries does not lead to liver infarction.
Clinical Presentation
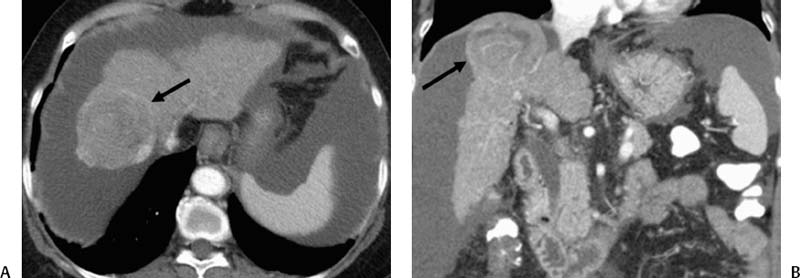
Radiologic Studies
Diagnosis
Treatment
Equipment
Transarterial Chemoembolization
Discussion
Background
| 50 mg of doxorubicin 50 mg of cisplatin powder (made for chemoembolization) 10 mg of mitomycin The agents are mixed in 10 cc sterile iodinated contrast 10 mL of Ethiodol* These agents can be emulsified and infused until near-stagnation of flow, followed by further embolization until stasis with Gelfoam† or polyvinyl alcohol particles, if selection of tumor vessels can be achieved. |
†Gelfoam, Pharmacia and Upjohn, Kalamazoo, Michigan.
Noninvasive Imaging Work-up
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree