Axial non-contrast head CT through the centrum semiovale.
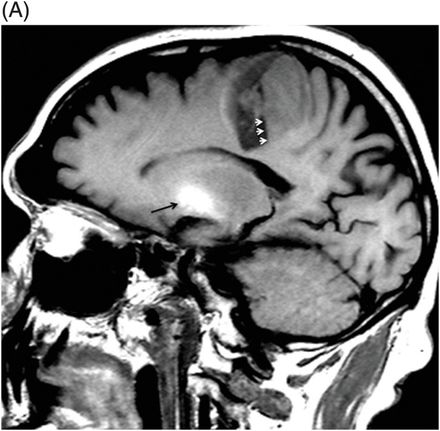
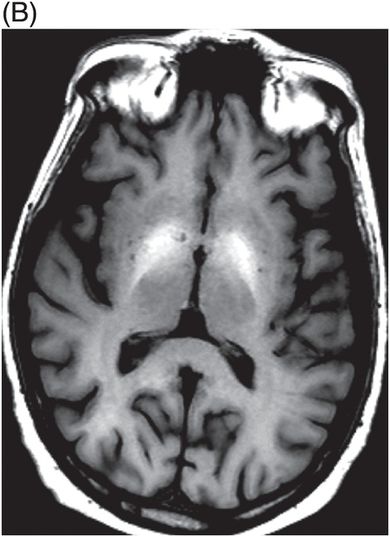
(A) Sagittal T1WI through the left basal ganglia. (B) Axial T1WI through the basal ganglia.
Chronic Hepatic Encephalopathy
Primary Diagnosis
Chronic hepatic encephalopathy
Differential Diagnoses
Trauma with physiologic basal ganglia calcification
Non-cirrhotic portal hypertension
Occupational exposure to manganese
Imaging Findings
Fig. 66.1: Axial non-contrast head CT through the centrum semiovale demonstrated a large intraparenchymal hematoma with minimal perihemorrhagic edema. Fig. 66.2: (A) Sagittal T1WI through the left basal ganglia demonstrated a large hematoma in the posterior aspect of the left frontal lobe, with hematocrit level (small white arrows). There is prominent T1 hyperintensity in the basal ganglia area (black arrow). (B) Axial T1WI through the basal ganglia demonstrated bilateral symmetric basal ganglia T1 hyperintensity.
Discussion
Bilaterally symmetric putaminal T1 hyperintensity is highly suggestive of chronic hepatic encephalopathy. The presence of abnormal liver function tests and ethanol in the urine confirm the diagnosis. Extrahepatic hemorrhage is a known complication of chronic liver disease, secondary to coagulopathy. T1 signal, characteristic of calcified lesions, depends upon the ionic state of the calcium and the presence of other minerals, in addition to the calcium in the calcified lesion. Physiologic basal ganglia calcification can cause T1 hyperintensity; however, the absence of physiologic calcification on CT scan excludes this possibility. Isolated intraparenchymal hematoma in this location is extremely unlikely to be trauma-related. In addition, CT imaging did not reveal any evidence of head injury. Large lobar hematoma can be a complication of amyloid angiopathy; however, amyloid angiopathy is very uncommon in adults less than 65 years of age and MRI did not reveal any characteristic microhemorrhage.
Hepatic encephalopathy (HE) consists of a series of neuropsychiatric, cognitive, and neuromuscular disorders in patients with comorbid liver disease. It is an important cause of mortality and morbidity in these patients. Hepatic encephalopathy can manifest as episodic, chronic HE, and clinical or subclinical HE. Chronic HE can be relapsing or persistent. Relapsing chronic HE consists of frequent episodes of acute HE due to other complications such as gastrointestinal tract bleeding, uremia, discontinuation of medication, or metabolic derangements, etc. In between two episodes, patients are usually cognitive and cooperative. Persistent chronic HE is irreversible and typically includes mental status change with or without abnormal movements.
In the setting of chronic liver disease, several metabolic alterations can cause CNS symptoms. Hepatic dysfunction causes an imbalance in the excitatory and inhibitory CNS neurotransmitters, and toxic buildup of many metabolites normally detoxified and excreted through the liver. For example, manganese (Mn) is one of the metabolites normally excreted through the liver. In hepatic failure, increased plasma Mn levels have a toxic effect on brain tissue, inducing selective neuronal loss and reactive gliosis in the globus pallidus (more prominently the medial segment) and substantia nigra. Patients with chronic HE frequently present with Parkinsonian syndromes secondary to Mn-induced selective basal ganglia injury.
Abnormal CNS Mn deposition can be readily identified on MRI. Bilateral symmetric T1 hyperintensity in the basal ganglia and in the substantia nigra are well-known findings of abnormal CNS Mn deposition in patients with chronic hepatic failure. Signal intensity increases after transjugular intrahepatic portosystemic shunt placement as the toxic metabolites are directly shunted from portal circulation to systemic circulation. Signal intensity may reverse with hepatic transplantation.
There is a disconnect between CNS Mn deposition and HE in patients with chronic liver disease. Almost all of the cirrhotic patients have abnormal pallidal T1 signal but not all chronic liver disease patients with abnormal pallidal T1 signal have chronic HE. Similarly, neuropsychiatric symptoms reverse immediately after liver transplantation; however, it takes up to a year to normalize the abnormal pallidal T1 signal. Although patients with chronic liver disease are coagulopathic, studies found intracerebral hemorrhage is very uncommon in chronic liver disease. The exact etiology of hemorrhage remained unknown in this patient as no obvious cause of hemorrhage could be found.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree