Sagittal T1WI through the midline.
Multiple System Atrophy-Cerebellar Type
Primary Diagnosis
Multiple system atrophy-cerebellar type
Differential Diagnoses
Idiopathic late-onset cerebellar ataxia
Toxin-mediated cerebellar ataxias
Paraneoplastic cerebellar ataxias
Hereditary cerebellar ataxias
Imaging Findings
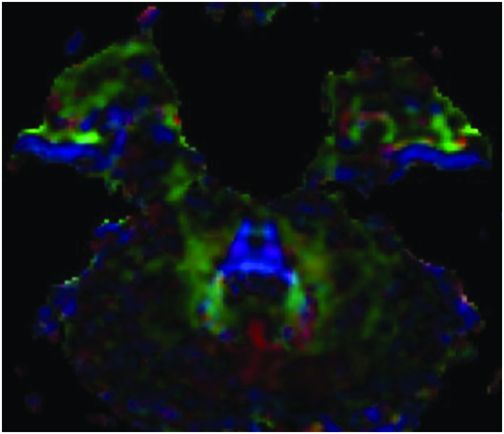
Fig. 8.1: Axial T2WI through the level of the pons demonstrated a cruciform-shaped, T2 hyperintensity through the middle of the pons (hot-cross-bun sign) due to atrophy of the cerebellopontine and transverse pontine fibers. Atrophy of the vermis is demonstrated by the enlargement of the sulci. Fig. 8.2: Sagittal T1WI through the midline demonstrated atrophy of the pons. Fig. 8.3: Colored FA map demonstrated absence of red transverse pontine fibers.
Discussion
Gradually progressing Parkinsonian syndromes (tremor, rigidity) in association with autonomic dysfunction and cerebellar signs are suggestive of possible multiple system atrophy (MSA), according to the second consensus statement on diagnosis of multiple system atrophy. Presence of cerebellar atrophy, hot-cross-bun sign, and pontine atrophy is suggestive of multiple system atrophy: cerebellar type, MSA-C, by the same definition.
Patients with MSA-P have similar clinical presentation, excluding the cerebellar symptoms, cerebellar and pontine atrophy. Idiopathic, late-onset cerebellar ataxia is a descriptive term defined by the presence of a primary progressive form of ataxia in the absence of any known exposure to common cerebellar toxins such as alcohol and antiseizure medications, and the absence of any known primary malignancies or hypothyroidism, with careful exclusion of MSA. The gradual unfolding of underlying genetic causes has led to the identification of many specific entities under the umbrella of idiopathic late-onset cerebellar ataxia (ILOCA), such as Friedreich ataxia, ataxia-telangiectasia, and fragile X-associated tremor. Although ILOCA and MSA-C share many clinical features, MSA-C is more commonly associated with Parkinsonian and premotor symptoms, such as urinary dysfunction, stridor, constipation, dysphagia, and sleep disturbances. Cerebellar atrophy can be seen in either of these syndromes, but pontine atrophy, middle cerebellar peduncle atrophy, and hot-cross-bun signs are not seen in any other ILOCA variety. Other causes of acquired cerebellar ataxias can easily be excluded by the patient’s history.
Multiple system atrophy is a descriptive term for a group of neurodegenerative disorders that were previously known as olivopontocerebellar degeneration, Shy Dragger syndrome, and striatonigral degeneration. It is one of the known three Parkinson-plus syndromes, namely progressive supranuclear palsy, corticobasal degeneration, and MSA. An adult-onset, sporadic neurodegenerative disease, MSA is characterized by autonomic failure in addition to Parkinsonian or cerebellar symptoms. In MSA-C, the cerebellar symptoms dominate the clinical findings. Histopathologically, MSA-C is characterized by alpha-synuclein-positive glial cytoplasmic inclusions and olivopontocerebellar degeneration.
Diagnosis of MSA subtypes is difficult, particularly during early stages. Like many other neurodegenerative diseases, diagnosis of MSA and its subtypes can be described as 1) definite (confirmed at autopsy); 2) probable or possible; or 3) with differing degrees of diagnostic certainty based on clinical and imaging findings. Indicative findings include the presence of autonomic failure (urinary incontinence, erectile dysfunction, or orthostatic hypotension), Parkinsonian symptoms that are refractory to treatment with levodopa, or cerebellar symptoms that consist of gait ataxia with cerebellar dysarthria, limb ataxia, or cerebellar oculomotor dysfunction.
Common abnormalities associated with MSA-C include atrophy of the pons, middle cerebellar peduncle, and cerebellum. Hot-cross-bun sign is characteristic of MSA-C; however, it is not pathognomonic, and is secondary to degeneration and gliosis of pontocerebellar fibers – irrespective of underlying pathologic processes – and usually develops late in the disease process. All of these imaging findings are usually late in the disease process, limiting their role in early diagnosis of MSA-C. On 18F-fluorodeoxyglucose positron emission tomography CT images, there is decreased glucose uptake in the brainstem and cerebellum in patients with MSA-C, as compared to control patients. There is also evidence of denervation of presynaptic nigrostriatal dopaminergic innervation on dopamine transporter scan images (DaT scan).
Treatment for MSA-C mainly targets Parkinsonism and dysautonomia symptoms; however, currently there is no treatment for the cerebellar symptoms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree