CASE 84 A 75-year-old man presents with severe, poorly localized abdominal pain and diarrhea. Fig. 84.1 (A,B) Axial and (C) coronal CT images show diffuse bowel wall thickening of the descending colon extending from the splenic flexure with pericolonic fat stranding and loss of the normal haustral pattern. The affected segment of colon has a typical targeted appearance with mild enhancement of the mucosal layer. Axial and coronal computed tomography (CT) images (Fig. 84.1) show diffuse bowel wall thickening of the descending colon extending from the splenic flexure with pericolonic fat stranding and loss of the normal haustral pattern. The affected segment of colon has a typical targeted appearance with mild enhancement of the mucosal layer. Acute mesenteric ischemia Mesenteric ischemia is a rare pathologic disorder (0.1% of emergency room admissions) predominantly affecting the older population of both genders (> 60 years), although it may occur in younger patients with predisposing risk factors. The prevalence of this condition is growing with the increase in average life expectancy. Three arteries provide the blood supply to the bowel: the celiac trunk, the superior mesenteric artery (SMA), and the inferior mesenteric artery (IMA). A decrease in blood flow can cause ischemia and subsequent reperfusion cell damage, leading to intestinal necrosis. Mesenteric ischemia may be acute or chronic, arterial or venous, diffuse or focal (watershed areas in the transverse colon near the splenic flexure or in the sigmoid colon are extremely vulnerable in cases of hypovolemia). Different etiologies, clinical presentations, and imaging findings have been identified for each of these pathologic entities. Patients with acute mesenteric ischemia usually present severe abdominal pain, diarrhea, nausea, and vomiting. Patients affected by chronic ischemia commonly experience postprandial abdominal pain (intestinal angina), weight loss, and food avoidance. Laboratory tests may reveal leukocytosis and an elevated serum lactate level (usually a late finding). Ischemia causes tissue necrosis, which in turn may lead to bowel perforation and subsequent peritonitis. Major causes of acute mesenteric ischemia include
Clinical Presentation
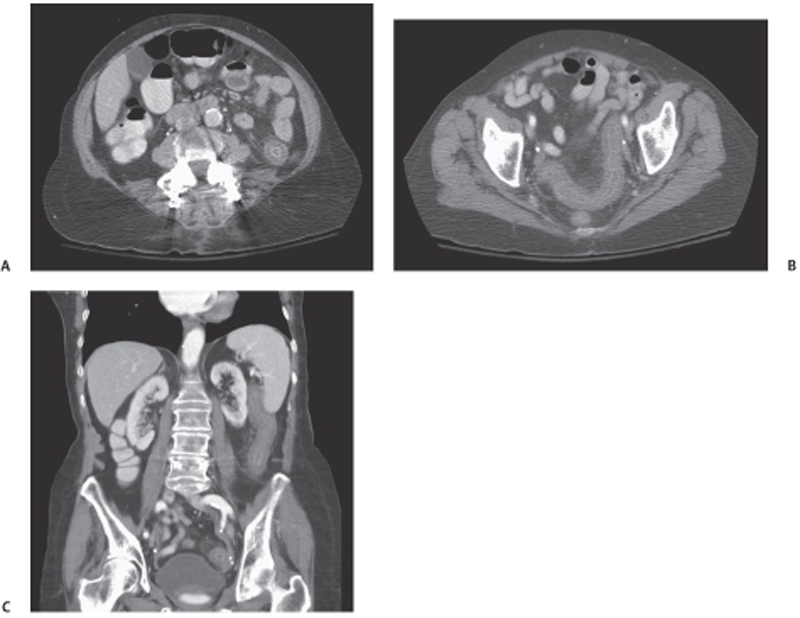
Radiologic Findings
Diagnosis
Differential Diagnosis
Discussion
Background
Clinical Findings
Complications
Etiology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree