9 Lymphatics and Nerves of the Thorax
Introduction
The thorax is an irregular cylinder with a narrow superior opening, the superior thoracic aperture, and a relatively large inferior opening, the inferior thoracic aperture. The superior thoracic aperture is open, allowing continuity with the neck, while the inferior thoracic aperture is covered by the diaphragm. The thorax houses and protects the heart, lungs, and great vessels along with their corresponding lymphatics and nerves. The mediastinum acts as a conduit for structures that (a) pass completely through the thorax from one body region to another or (b) connect organs in the thorax to other body regions. 1
Although the nerves of the thorax are rarely identified at cross-sectional imaging, their location can be inferred by localizing easily identified anatomical landmarks. Familiarity with the functional anatomy and clinical significance of the nerves of the thorax is important for interpreting thoracic images correctly. 2 However, various noninvasive diagnostic techniques such as chest radiography, computed tomography (CT), positron emission tomography (PET), and magnetic resonance imaging (MRI) are currently available for assessing the intrathoracic lymphatic system. The lymph nodes distributed through the mediastinum and hila are best understood by correlation with CT and MR cross-sectional images. 3
Nerves
Innervation of Thoracic Wall
Innervation of the thoracic wall is primarily by the intercostal nerves, which are the anterior rami of spinal nerves T1 to T11 and lie in the intercostal spaces between adjacent ribs (Fig. 9‑1). The ventral ramus of spinal nerve T12 (the subcostal) is inferior to the 12th rib.
These nerves innervate the thoracic wall, related parietal pleura, and associated skin. A typical intercostal nerve passes laterally around the thoracic wall in an intercostal space. The largest branch is the lateral cutaneous, which pierces the lateral thoracic wall and divides into anterior and a posterior branch that innervate the overlying skin. 1
In addition to the thoracic wall, the intercostal nerves innervate other regions; for example, the ventral ramus of T1 contributes to the brachial plexus, the lateral cutaneous branch of the second intercostal nerve (the intercostobrachial) contributes to cutaneous innervation of the medial upper arm, and the lower intercostal nerves supply muscles, skin, and peritoneum of the abdominal wall. 1
The intercostal nerves end as anterior cutaneous branches, which emerge either parasternally, between adjacent costal cartilages, or laterally to the midline, on the anterior abdominal wall, to supply the skin. In addition to these major branches, small collateral branches run in the intercostal space along the superior border of the lower rib. 1
The dermatomes of the thorax generally reflect the segmental organization of the thoracic spinal nerves (see Volume II, Chapter 1, Abdominopelvic Wall). The exception, anteriorly and superiorly, is the first thoracic dermatome, which is located mostly in the upper limb, not on the trunk. The anterosuperior region of the trunk receives branches from the ventral ramus of C4 via supraclavicular branches of the cervical plexus. The highest thoracic dermatome on the anterior chest wall is T2, which also extends into the upper limb. At the midline, the skin over the xiphoid process is innervated by branches of the T6 spinal nerve. The dermatomes of T7 to T12 follow the contour of the ribs onto the anterior abdominal wall.
In the thorax, the intercostal nerves carry somatic motor innervation to the muscles of the thoracic wall (intercostal, subcostal, and transversus thoracis), somatic sensory innervation from the skin and parietal pleura, and postganglionic sympathetic fibers to the periphery. 1
Vagus Nerves
The vagus nerves pass through the superior and posterior divisions of the mediastinum on their way to the abdominal cavity. They pass through the diaphragm with the esophagus. En route through the thorax, they provide parasympathetic innervation to the thoracic viscera and carry visceral afferents from them. 1 In brief, the right and left vagus nerves enter the thorax between their respective brachiocephalic veins and the subclavian artery, medial to the mediastinal pleura (Fig. 9‑2 , Fig. 9‑3). In good-quality CT images, the vagus nerve may be seen at the thoracic inlet behind the brachiocephalic veins. They descend posterior to their respective pulmonary hila, ramify to form the esophageal plexus, and then pass through the esophageal hiatus of the diaphragm as the anterior and posterior vagal trunks. 2


Right Vagus Nerve
The right vagus nerve enters the superior mediastinum and lies between the right brachiocephalic vein and the innominate artery. It descends in a posterior direction toward the trachea, crosses the lateral surface of the trachea, and passes posteriorly to the root of the right lung to reach the esophagus. Just before the esophagus, the arch of the azygos vein crosses it. As it passes through the superior mediastinum, it gives branches to the esophagus, cardiac plexus, and pulmonary plexus. 1 , 2
Left Vagus Nerve
The left vagus nerve enters the superior mediastinum posterior to the left brachiocephalic vein and between the left common carotid and left subclavian arteries. As it passes into the superior mediastinum, it lies just deep to the mediastinal part of the parietal pleura and crosses the left side of the arch of aorta. Inferiorly, it runs lateral to the trachea and esophagus. It continues to descend in a posterior direction and passes posterior to the root of the left lung to reach the esophagus in the posterior mediastinum. 1 , 2
As the left vagus nerve passes through the superior mediastinum, it gives branches to the esophagus, the cardiac plexus, and the pulmonary plexus. Also, the left recurrent laryngeal nerve arises from it at the inferior margin of the arch of aorta just lateral to the ligamentum arteriosum (Fig. 9‑4). The left recurrent laryngeal nerve passes inferior to the arch of aorta before ascending on its medial surface. Entering a groove between the trachea and esophagus, it continues superiorly to enter the neck and terminates in the larynx. 1
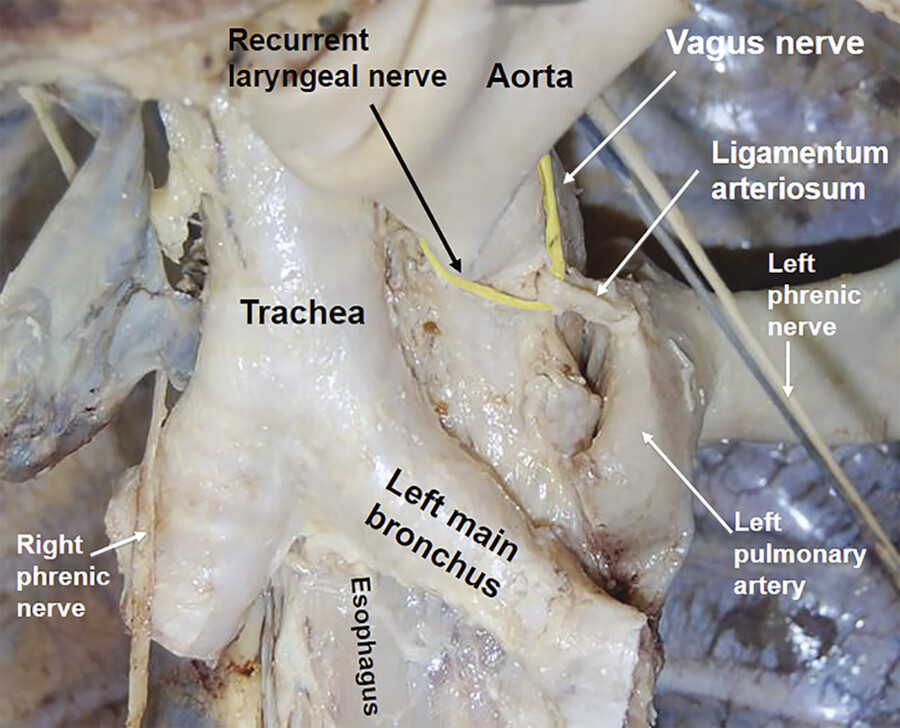
Recurrent Laryngeal Nerves
The recurrent laryngeal nerves follow an asymmetric pathway through the upper chest. The right recurrent laryngeal nerve originates from the right vagus nerve at the level of the right subclavian artery and loops under this artery to ascend out of the thorax. The left recurrent laryngeal nerve originates from the left vagus nerve at the level of the transverse aortic arch and loops under it immediately posterior to the ligamentum arteriosum to ascend along the posterolateral tracheal margin and exit the thorax (Fig. 9‑4). The recurrent laryngeal nerves provide ipsilateral motor innervation to the intrinsic laryngeal muscles for vocalization and sensory innervation to the upper esophagus. They also mediate airway sensation from the level of the true vocal cords to the carina. 2
Phrenic Nerves
The phrenic nerves lie along the lateral mediastinum and run from the thoracic inlet to the diaphragm (Fig. 9‑5, Fig. 9‑6). They course through the upper chest, medial to the mediastinal pleura and the apex of the right or left lung. They provide motor innervation to the diaphragm and sensory innervation to its central intrathoracic and peritoneal surfaces. They also innervate the pericardium and mediastinal pleura and mediate pain from these areas to the neck and shoulder. Manifestations of phrenic nerve disease include diaphragmatic paralysis with elevation or persistent hiccups. The phrenic nerves in their neurovascular bundle can occasionally be visualized on cross-sectional imaging. 2 It is easier to see the left phrenic neurovascular bundle as it passes over the left pericardium.


Right Phrenic Nerve
The right phrenic nerve enters the superior mediastinum lateral to the right vagus nerve and lateral and slightly posterior to the beginning of the right brachiocephalic vein. It continues inferiorly along the right side of this vein and the right side of the superior vena cava (Fig. 9‑6). On entering the middle mediastinum, it descends along the right side of the pericardial sac, within the fibrous pericardium, anterior to the root of the right lung. The pericardiacophrenic vessels accompany it through most of its course in the thorax. It leaves the thorax by passing through the diaphragm with the inferior vena cava. 1
Left Phrenic Nerve
The left phrenic nerve enters the superior mediastinum in a position similar to the path taken by the right phrenic nerve. It lies lateral to the left vagus nerve and lateral and slightly posterior to the beginning of the left brachiocephalic vein and continues to descend across the left lateral surface of the arch of aorta, passing superficially to the left vagus nerve and the left superior intercostal vein. On entering the middle mediastinum, it follows the left side of the pericardial sac, within the fibrous pericardium, anterior to the root of the left lung, and is accompanied by the pericardiacophrenic vessels (Fig. 9‑3, Fig. 9‑5). It leaves the thorax by piercing the diaphragm near the apex of the heart. 1
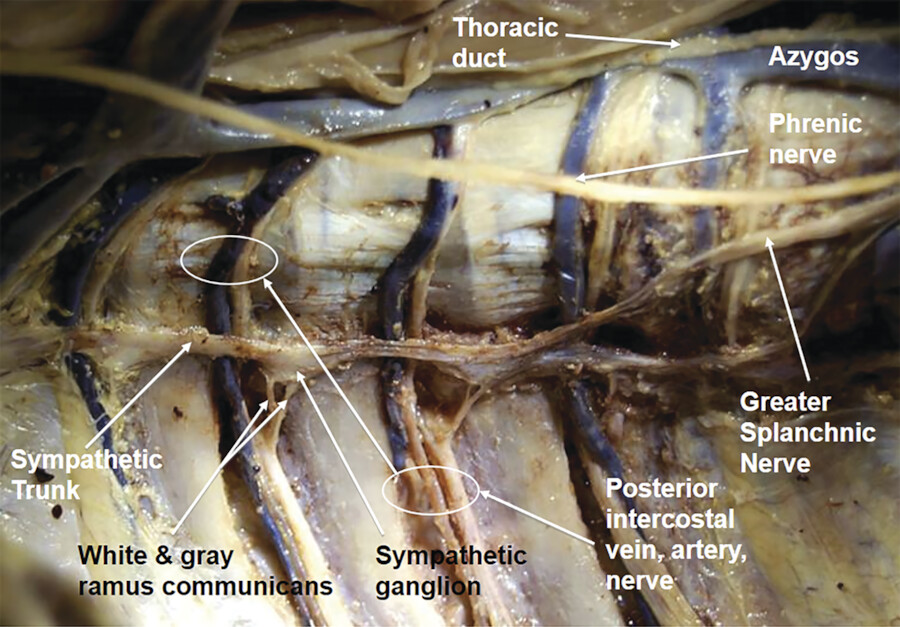
Sympathetic Nerves
The sympathetic trunks (chains) of the thorax are paired, symmetric structures that extend from the thoracic inlet to the diaphragm (Fig. 9‑6 , Fig. 9‑7 , Fig. 9‑8). These fibers and ganglia run in a vertical line that crosses the necks of the ribs. They are covered by the parietal pleura, except for the most inferior segment of the right trunk. Preganglionic nerves from the spinal cord synapse at the sympathetic ganglia, and the postganglionic fibers emerge from the ganglia to a visceral organ.


All preganglionic nerve fibers of the sympathetic system are carried out of the spinal cord in spinal nerves T1 to L2. This means that sympathetic fibers found anywhere in the body ultimately emerge from the spinal cord as components of those spinal nerves. Preganglionic sympathetic fibers destined for the head are carried out in spinal nerve T1. 1 The sympathetic ganglia of the thorax are symmetric bilateral chains of 11 ganglia in the paravertebral soft tissue and in continuity with the neck and abdominal chains. Three splanchnic branches emerge from each trunk and pass medially to the abdominal sympathetic ganglia. 2
Motor Innervation of the Diaphragm
The diaphragm is innervated by the two phrenic nerves that originate, one on each side, as branches of the cervical plexus in the neck. They arise from the anterior rami of cervical nerves C3, C4, and C5, the main contribution coming from C4. They penetrate the diaphragm and innervate it from its abdominal surface (Fig. 9‑8).
The phrenic nerves pass vertically through the neck, the superior thoracic aperture, and the mediastinum to supply motor innervation to the entire diaphragm, including the crura (muscular extensions that attach the diaphragm to the upper lumbar vertebrae). In the mediastinum, they pass anteriorly to the roots of the lungs. Spinal cord injuries below the level of origin of the phrenic nerve do not affect movement of the diaphragm. 1
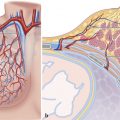
Pulmonary Innervation
Structures of the lung, and the visceral pleura, are supplied by visceral afferents and efferents distributed through the anterior pulmonary plexus and posterior pulmonary plexus. These interconnected plexuses lie anteriorly and posteriorly to the tracheal bifurcation and main bronchi. The anterior plexus is much smaller than the posterior. Branches of these plexuses, which ultimately originate from the sympathetic trunks and vagus nerves, are distributed along branches of the airway and vessels. Visceral efferents from the vagus nerves constrict the bronchioles while the sympathetic system dilates them. 1
Esophageal Innervation
The thoracic part of the esophagus lies between the trachea and the vertebral column in the superior mediastinum. On its way down, the esophagus passes behind the aortic arch, and enters the posterior mediastinum at the level of T4/T5 intervertebral discs. The thoracic duct lies on the left side, and the left recurrent laryngeal nerve lies in the left tracheoesophageal groove. Laterally, on the left side, it is related to the aorta and left subclavian artery; on the right side, it is related to the azygos vein. Anteriorly, the esophagus is related to the trachea, right pulmonary artery, left bronchus, pericardium with left atrium, and diaphragm. Posteriorly, it is related to the vertebral column, right posterior intercostal arteries, thoracic duct, thoracic part of the aorta, and diaphragm. In the posterior mediastinum, the esophagus is related to the descending thoracic aorta, left mediastinal pleura, azygos vein, and cardiac and pulmonary plexus. 4
In general, innervation of the esophagus is complex. Esophageal branches arise from the vagus nerves and sympathetic trunks to form the esophageal plexus (Fig. 9‑6 , Fig. 9‑7). Striated muscle fibers in the superior portion of the esophagus originate from the branchial arches and are innervated by branchial efferents from the vagus nerves. Smooth muscle fibers are innervated by components of the parasympathetic part of the autonomic division of the peripheral nervous system, visceral efferents from the vagus nerves. These are preganglionic fibers that synapse in the myenteric and submucosal plexuses of the enteric nervous system in the esophageal wall. Sensory innervation of the esophagus involves visceral afferent fibers originating in the vagus nerves, sympathetic trunks, and splanchnic nerves. 1
Cardiac Innervation
The fibrous pericardium is a cone-shaped bag with its base on the diaphragm and its apex continuous with the adventitia of the great vessels. Nerves supplying the pericardium arise from the vagus nerve, the sympathetic trunks, and the phrenic nerves. The phrenic nerves, which innervate the diaphragm and originate from spinal cord levels C3 to C5, pass through the fibrous pericardium and innervate it as they travel toward their final destination. The source of somatic sensation (pain) from the parietal pericardium is carried by somatic afferent fibers in the phrenic nerves. Therefore, “pain” related to a pericardial problem can be referred to the supraclavicular region of the shoulder or lateral neck area, the dermatomes for spinal cord segments C3, C4, and C5.
The autonomic division of the peripheral nervous system is directly responsible for regulating heart rate, the force of each contraction and cardiac output. Branches from both the parasympathetic (vagus) and sympathetic systems contribute to forming the cardiac plexus. This plexus consists of a superficial part, inferior to the aortic arch and between it and the pulmonary trunk, and a deep part, between the aortic arch and the tracheal bifurcation.
From the cardiac plexus, small branches that contain both sympathetic and parasympathetic fibers supply the heart. They affect nodal tissue and other components of the conduction system, the coronary blood vessels, and the atrial and ventricular musculature. 1
Parasympathetic Innervation
Stimulation of the parasympathetic system decreases the heart rate, reduces the force of contraction, and constricts the coronary arteries. The preganglionic parasympathetic fibers reach the heart as cardiac branches from the right and left vagus nerves. 1 They enter the cardiac plexus and synapse in ganglia located either within the plexus or in the walls of the atria primarily over the superior aspect and posterior surfaces of the atria near the posterior atrioventricular groove.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree