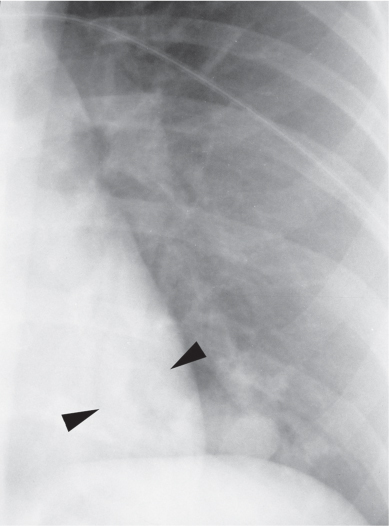
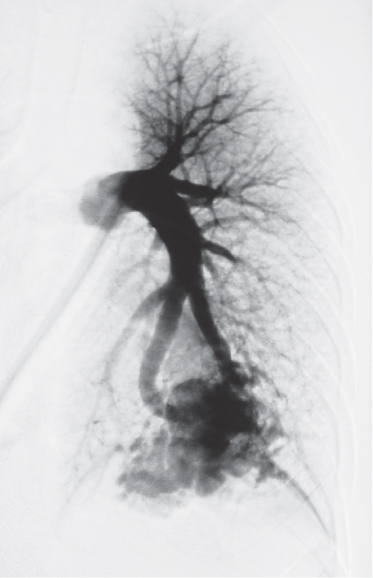
CASE 9 22-year-old woman with postpartum dyspnea and hypoxemia Coned-down PA chest radiograph (Fig. 9.1) demonstrates a left lower lobe mass of lobular contours with tubular opacities (arrowheads) coursing between the mass and the left hilum. Left pulmonary arteriogram (Figs. 9.2, 9.3) demonstrates a pulmonary arteriovenous malformation supplied by two branches of the left interlobar pulmonary artery (Fig. 9.2) that drains into the left atrium (LA) via an enlarged pulmonary vein (Fig. 9.3). Pulmonary Arteriovenous Malformation • Arteriovenous Fistula • Pulmonary Artery Aneurysm Fig. 9.1 Fig. 9.2 Fig. 9.3 (Images 9.1–9.3 are courtesy of Wanda M. Kirejczyk, MD, New Britain General Hospital, New Britain, Connecticut.) A pulmonary arteriovenous malformation (PAVM) is an abnormal communication between a pulmonary artery and a pulmonary vein without an intervening capillary bed, and results in a right-to-left shunt. Simple PAVMs (90%) are defined as single or multiple feeding arteries originating from a single segmental pulmonary artery. Complex PAVMs (10%) are characterized by feeding arteries originating from two or more segmental pulmonary arteries. Approximately 33% are multiple; 20% are bilateral. PAVMs are thought to arise from congenital defects in the capillary bed, which result in a direct communication between the pulmonary arterial and venous circulations. Acquired arteriovenous communications also occur, usually follow trauma (non-iatrogenic or iatrogenic) or inflammation, and are designated arteriovenous fistulae. Rendu-Osler-Weber syndrome or hereditary hemorrhagic telangiectasia (HHT) is an autosomal dominant disorder characterized by recurrent epistaxis, mucocutaneous telangiectasias, and arteriovenous malformations, with an estimated prevalence of one in 5,000 to 10,000 persons. Approximately 60–90% of PAVMs occur in patients with HHT, up to 35% of patients with HHT have one or more PAVMs, and 60% of patients with HTT-related PAVMs have multiple lesions.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis

 Discussion
Discussion
Background
Etiology
Clinical Findings
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine