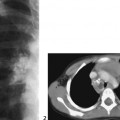
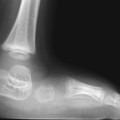
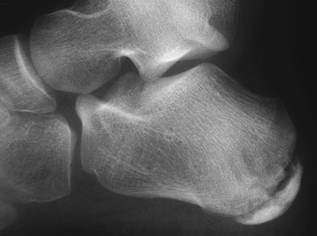
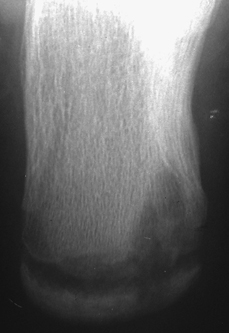
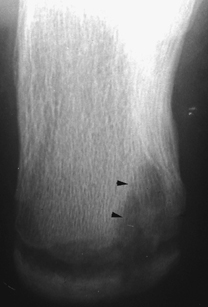
CASE 99 An 11-year-old boy presents with chronic heel pain and mild fever. Figure 99A Figure 99B Lateral radiograph of calcaneus demonstrates inhomogeneous bone density with areas of both patchy sclerosis and increased lucency posteriorly (Fig. 99A). The calcaneal view better defines the lytic component extending into adjacent apophyseal center (Fig. 99B). Chronic osteomyelitis (OM) Langerhans’ cell histiocytosis OM is an infection of bone and bone marrow clinically divided into acute, subacute, and chronic entities. Host resistance, virulence of the organism, and the response to treatment with antimicrobials are the major factors contributing to the development of one entity over another. OM is polyostotic in ~6% of cases and has a predilection for rapidly growing sites in the immature skeleton such as the metaphyses (or metaphyseal equivalent) of the distal femur and radius as well as proximal tibia and humerus. Neonatal OM has an incidence of 1 to 3 per 1000 hospital admissions, often involving the hips, and is multifocal in 23 to 47% of cases. Routes for infection include hematogenous seeding infection (most common form in children), contiguous spread from adjacent soft tissue or joint, and direct inoculation due to trauma. Approximately 2% of all orthopedic procedures are complicated by infection. Infection in the neonate and young infant is often clinically silent. Toddlers and children present with pain in limb with passive motion, pseudoparalysis, or a limp. The area may be red, swollen, and warm on examination. Acute infection via hematogenous seeding results in marrow edema and cellular infiltration usually in the metaphysis of a long bone. The physeal plate in infants and children between ~8 and 18 months of age acts as a relative barrier, localizing the disease process, whereas in both younger infants and older children the infection is more likely to spread to the epiphysis via transphyseal vascular pathways and may extend into the joint space. Progression of infiltrate within the marrow cavity results in an increase in intraosseous pressure leading to extension of the inflammatory process through the cortex and into subperiosteal space via haversian and Volkmann’s canals. Figure 99C Calcaneal view depicts area of ill-marginated lucency (arrowheads). Figure 99D Frontal radiograph of ankle depicts a lytic lesion within distal tibial metaphysis crossing the physis and extending into epiphysis. Margins are ill defined in some segments and well demarcated in others. There is a faint central area of increased bone density. The process may then continue to spread into periosteum and overlying soft tissues. The increased intraosseous pressure can impair blood flow leading to ischemic necrosis of bone resulting in devas-cularized fragments called sequestra. A subacute OM is a more localized pyogenic process in which the term Brodie’s abscess is used when complicated by surrounding granulation tissue and sclerotic bone. Chronic OM is a low-grade continuing infection classified as active or inactive. The process may be indolent for long periods before re-activation. The clinical diagnosis of chronic osteomyelitis can be made if symptoms have been present for >1 month, if there has been inadequate treatment, or if the infection arose >1 month after surgery for trauma.
Clinical Presentation
Radiographic Findings
Diagnosis
Differential Diagnosis
Discussion
Background
Etiology
Clinical Findings
Complications
Pathophysiology

Laboratory
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree