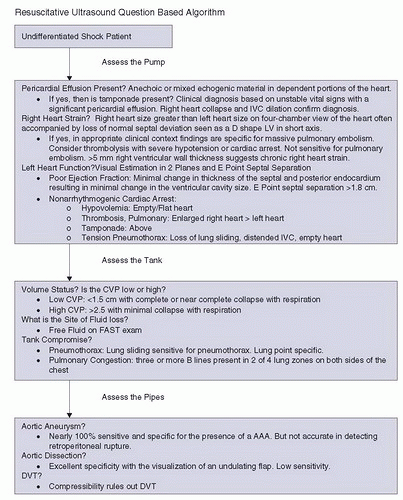
THE BASIC EXAM
The purpose of an algorithmic approach to resuscitative ultrasound is to provide a basic exam that is comprehensive yet still practical and covers most of the relevant questions in a timely, efficient manner. However, no single approach fits
every clinical scenario, and the exam is not intended to be rigid. In fact, depending upon one’s skill level and the clinical setting, certain portions of the exam may not be integrated at all. There is value in learning and using portions of the exam and gradually adding others as one’s proficiency improves.
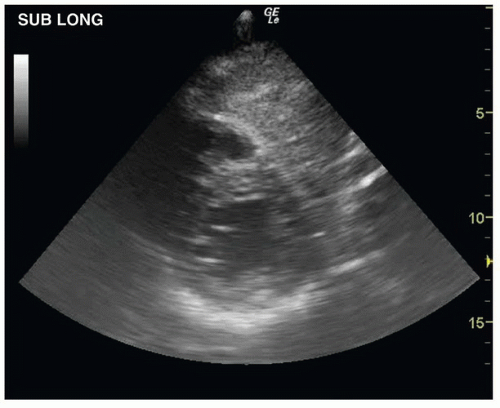
A designated ultrasound machine should be immediately available in the resuscitation suite at all times, at the bedside, ready for use. The exam begins with an examination of the heart. Many prefer a small footprint phased array probe to begin with, although a curvilinear probe allows one to transition from the cardiac exam to other applications without delay. Begin with a subxyphoid approach. If a good window is obtained, assess for myocardial contractility, determine if a pericardial effusion is present, and note the relative sizes of the left and right ventricles. The probe can then be turned into a longitudinal orientation and the scan oriented more to the left to obtain a short view of the right and left ventricle similar in appearance to the parasternal short view (
Fig. 7.2;

VIDEO 7.1) (
11). If the subxyphoid view is inadequate, other cardiac views can be used based on the individual patient and the sonographer’s experience. If the examiner is comfortable with other views, a more thorough kinesis assessment may be completed from the parasternal views. From the parasternal long view, assess for vigorous and synchronous motion of the anterior leaflet of the mitral valve, left ventricle septal and posterior wall, and aortic valve. Qualitative visual estimates of left ventricular function have been demonstrated across multiple
specialties to be a reliable indicator of overall contractility (
4,
12,
13). Rotate the probe to the short axis view to confirm the overall contractility and identify regional wall motion abnormalities.
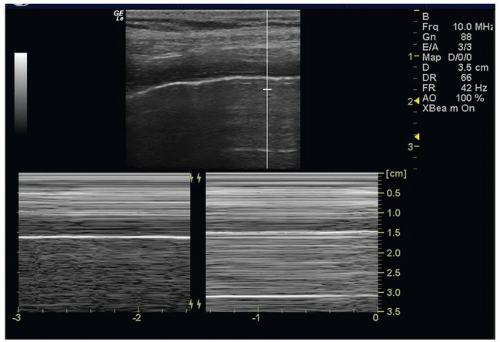
Should time allow, measuring the
E-point septal separation (
EPSS) provides a rapid and simple quantitative confirmation of the initial subjective impression of systolic function. From the parasternal long view, measure the distance between the anterior leaflet of the mitral valve and the septum utilizing M-mode (
Fig. 7.3) (
13).
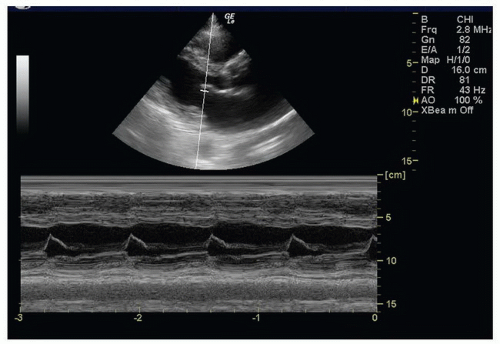
Once the cardiac views have been obtained, next focus on assessment of the IVC (and volume status of the patient). From the subxyphoid position, the probe can be moved inferiorly toward the abdomen to visualize the junction of the right atrium and IVC, then the hepatic veins draining into the IVC. The IVC will be in transverse orientation using this technique. Clear consensus on the optimal patient position, scanning plane, and point at which to measure the IVC has yet to be established. The transverse view prevents imaging errors such as the
cylinder tangential effect; it also prevents a common problem with mistaking the aorta for the IVC in the difficult to visualize patient (
14). Other investigators have also described the long axis approach to IVC visualization; this can be obtained simply by turning the probe from the subxyphoid position into a longitudinal scanning plane (
15,
16). In this view the scanner can avoid less accurate measurements near the diaphragm where the IVC may be narrowed. In either plane, visualize and measure the IVC 1 to 2 cm below the diaphragm. Record a cine loop, then scroll through still images to identify the smallest and largest diameters. When the borders of the IVC are clearly visualized, both visual estimation and M-mode measurements provide reliable measurements (
Fig. 7.4;
 VIDEO 7.2
VIDEO 7.2) (
17).
On occasion, visualization of the IVC may be difficult. The internal jugular (IJ) vein provides an alternative site to estimate central venous pressure. However, it requires the sonographer to move to an alternate site, and may require use of a different probe. These disadvantages add time and complexity to the basic exam; the information gained may be worth it in patients in whom the IVC simply cannot be visualized. Clinicians are likely to be familiar with this anatomy since an assessment is always completed as part of ultrasound-guided IJ line placement. A linear probe provides the best view, but in obese patients, a curvilinear or phased array probe may be better. To avoid inadvertent compression by the probe, in the transverse plane begin by purposely compressing the IJ. Then release pressure until visualizing the vein’s greatest diameter. In a normal upright patient, the IJ is collapsed during respiration. Progressively reclining the normal patient to a more recumbent position causes the IJ to become increasingly visible throughout respiration. Most basic scans will not require visualization of the IJ. It is included to provide an option for the occasional patient.
After completing the IVC scan, it is easy to move to an extended FAST scan. After viewing the IVC, a minor change in probe position will easily obtain a view of Morison’s pouch; a slight move cephalad is all that is necessary to view the right costophrenic angle to look for a right pleural effusion. At this point the sonographer can choose which scan is most important to prioritize. If the patient has a flat or highly compressible IVC and hypovolemia or hemorrhage is suspected, the priority may be to complete the FAST scan. If the patient has evidence of a full, distended IVC and poor cardiac function, or the patient is dyspneic, there may be a higher priority to scan the chest. The sonographer can obtain views of the splenorenal space and pelvis next, or move to the thoracic scan.
The scan of the thorax can be completed with the curvilinear transducer, although some will prefer a linear higher frequency transducer for improved resolution, particularly if there is significant concern for pneumothorax. If scanning to assess for interstitial fluid, the curvilinear transducer offers deeper penetration and a better view of
B-lines. Begin the scan by placing the probe of choice in a longitudinal scanning plane on the anterior superior surface of the chest, and adjust the depth of view to visualize the pleural line between two ribs. Normal
lung sliding excludes the presence of a pneumothorax (
Fig. 7.5;
 VIDEOS 7.3 and 7.4
VIDEOS 7.3 and 7.4). Color flow and power Doppler make this movement readily visible. Likewise, M-mode may be helpful to confirm the normal
seashore sign, or detect the
barcode sign suggestive of pneumothorax. The focal depth should be increased to inspect the lung for
B-lines. Looking deep from the pleural, determine if there is a predominance of
A-lines (horizontal lines deep to the pleura, reverberation artifact seen in normal lung) or
B-lines (echogenic vertical ray-like projections that extend from the pleural surface to deep in the chest). B-lines erase A-lines; scans typically have predominance of A-lines or B-lines. B-line predominance suggests interstitial fluid or abnormal lung. Increasing number of B-lines corresponds to severity of interstitial fluid. Different protocols have been proposed for a complete evaluation of the chest (
5,
18,
19). For the emergency department (ED) scan, the chest may be divided into eight zones: superior and inferior, anterior and lateral, to give four zones each in the right and left chest. During the general inspection of the chest, the scan may also detect large pleural effusions or consolidated lung segments.
Once the cardiac, IVC, and thoracic scans are done, the clinician has a fairly complete assessment of the physiologic status of the patient to guide the initial resuscitation and help classify the type of shock. Depending upon the results, the sonographer can take a directed approach to further imaging based on their differential diagnosis.
The sonographer may return to the abdomen to complete the FAST exam to look for intra-abdominal fluid, or consider surveying the abdomen for a potential source of sepsis. By adding the views of the splenorenal space and the pelvis, the FAST is easily completed. The scan may also be used to check other intra-abdominal conditions such as acute cholecystitis, hydronephrosis with urosepsis, or an intra-abdominal or pelvic abscess. If concern exists for an abdominal aortic aneurysm (AAA), the aorta can be included in the abdominal survey. Obviously, in cases of sudden back pain and hypotension, hypotension in face of an abdominal mass, or a known AAA, the clinician will likely have prioritized this application early in the assessment of the patient. To examine the abdominal aorta, place the curvilinear or phased array probe in the midline epigastrium in the transverse scanning plane to quickly visualize the hyperechoic vertebral body in the far field, with the pulsating aorta just anterior and to the right of the prevertebral stripe, and the teardrop-shaped compressible IVC to the left. Lift and press in 1-cm caudad “jumps” to displace bowel gas in between the probe and the aorta, bringing the proximal
branch vessels into view. The aorta should be visualized from the xyphoid process to below the bifurcation to avoid missing a small saccular aneurysm behind transverse colon or other bowel gas. Continue distally until both iliac arteries have been clearly visualized. Always measure the outermost wall to outermost wall of the aorta, not just the lumen, which may be partially blocked by acute or chronic thrombus.
Scan the aorta in the longitudinal scanning plane to quickly confirm findings or, better, detect the presence of a dissection flap. If an aortic dissection is suspected, return to the chest to visualize the aortic root on the parasternal long view. When dilated more than 4 cm, inspect carefully for the presence of a secondary hemopericardium or a dissection flap. The descending aorta is seen in short axis in the far field of this same parasternal long view. Move to the parasternal short axis view to obtain a limited long axis view of the descending aorta. When possible, extend the patient’s neck and place the probe in the sternal notch in the transverse scanning plane aiming anterior and caudad into the superior mediastinum to visualize the aortic arch.
Finally, if a pulmonary embolism (PE) is suspected, the sonographers can wrap up their assessment with evaluation for deep venous thrombosis (DVT). Place the linear probe just below the inguinal ligament in the transverse scanning plane. In obese patients, the curvilinear probe may allow adequate depth. Visualize the common femoral artery and vein. If no echogenic thrombus is noted, lift and compress the vein to exclude thrombus. Next, in 1-cm jumps, move down the proximal anterior medial thigh, visualizing the compressible common femoral vein moving beneath the superficial femoral artery, then bifurcating into the superficial and deep femoral veins. Time permitting, continue to compress the superficial femoral vein down to the distal two-thirds of the thigh. However, since the 99% of DVT’s are located proximally in the common femoral vein or distally in the popliteal fossa, this area may be skipped when time is limited (
20). Abduct the thigh and flex the knee slightly to facilitate placement of the probe in the popliteal fossae. Note that the popliteal vein now sits above the popliteal artery, opposite of the femoral artery and vein, remembered easily as the “pop on top.” Compress in 1-cm jumps again until the trifurcation of the popliteal vein is clearly visualized.
The resuscitative ultrasound algorithm for the patient in undifferentiated shock is intended to be quick, and in experienced hands can be accomplished in just a few minutes (
8,
9). For many, however, acquiring expertise will require time and experience, and the applications should be focused on the most essential questions. In some instances, abnormal findings will dictate action that should interrupt the scan. If a febrile patient appears septic and has a vigorous ejection fraction (EF) and collapsible IVC consistent with sepsis, the exam may be interrupted to obtain central venous access, administer fluids, and antibiotics. The scan may be resumed to look for a focal source of infection, or reassess response to fluids. The real value of the resuscitative ultrasound is its ability to be adaptable to the situation, answer questions, assist interventions, and help with reassessments.
 VIDEO 7.1) (11). If the subxyphoid view is inadequate, other cardiac views can be used based on the individual patient and the sonographer’s experience. If the examiner is comfortable with other views, a more thorough kinesis assessment may be completed from the parasternal views. From the parasternal long view, assess for vigorous and synchronous motion of the anterior leaflet of the mitral valve, left ventricle septal and posterior wall, and aortic valve. Qualitative visual estimates of left ventricular function have been demonstrated across multiple
VIDEO 7.1) (11). If the subxyphoid view is inadequate, other cardiac views can be used based on the individual patient and the sonographer’s experience. If the examiner is comfortable with other views, a more thorough kinesis assessment may be completed from the parasternal views. From the parasternal long view, assess for vigorous and synchronous motion of the anterior leaflet of the mitral valve, left ventricle septal and posterior wall, and aortic valve. Qualitative visual estimates of left ventricular function have been demonstrated across multiple  VIDEO 7.2) (17).
VIDEO 7.2) (17).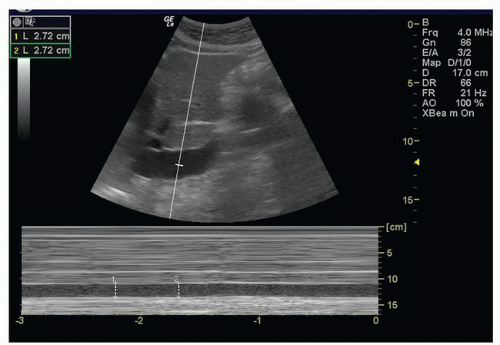
 VIDEOS 7.3 and 7.4). Color flow and power Doppler make this movement readily visible. Likewise, M-mode may be helpful to confirm the normal seashore sign, or detect the barcode sign suggestive of pneumothorax. The focal depth should be increased to inspect the lung for B-lines. Looking deep from the pleural, determine if there is a predominance of A-lines (horizontal lines deep to the pleura, reverberation artifact seen in normal lung) or B-lines (echogenic vertical ray-like projections that extend from the pleural surface to deep in the chest). B-lines erase A-lines; scans typically have predominance of A-lines or B-lines. B-line predominance suggests interstitial fluid or abnormal lung. Increasing number of B-lines corresponds to severity of interstitial fluid. Different protocols have been proposed for a complete evaluation of the chest (5,18,19). For the emergency department (ED) scan, the chest may be divided into eight zones: superior and inferior, anterior and lateral, to give four zones each in the right and left chest. During the general inspection of the chest, the scan may also detect large pleural effusions or consolidated lung segments.
VIDEOS 7.3 and 7.4). Color flow and power Doppler make this movement readily visible. Likewise, M-mode may be helpful to confirm the normal seashore sign, or detect the barcode sign suggestive of pneumothorax. The focal depth should be increased to inspect the lung for B-lines. Looking deep from the pleural, determine if there is a predominance of A-lines (horizontal lines deep to the pleura, reverberation artifact seen in normal lung) or B-lines (echogenic vertical ray-like projections that extend from the pleural surface to deep in the chest). B-lines erase A-lines; scans typically have predominance of A-lines or B-lines. B-line predominance suggests interstitial fluid or abnormal lung. Increasing number of B-lines corresponds to severity of interstitial fluid. Different protocols have been proposed for a complete evaluation of the chest (5,18,19). For the emergency department (ED) scan, the chest may be divided into eight zones: superior and inferior, anterior and lateral, to give four zones each in the right and left chest. During the general inspection of the chest, the scan may also detect large pleural effusions or consolidated lung segments.