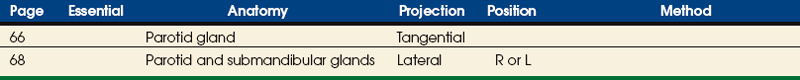
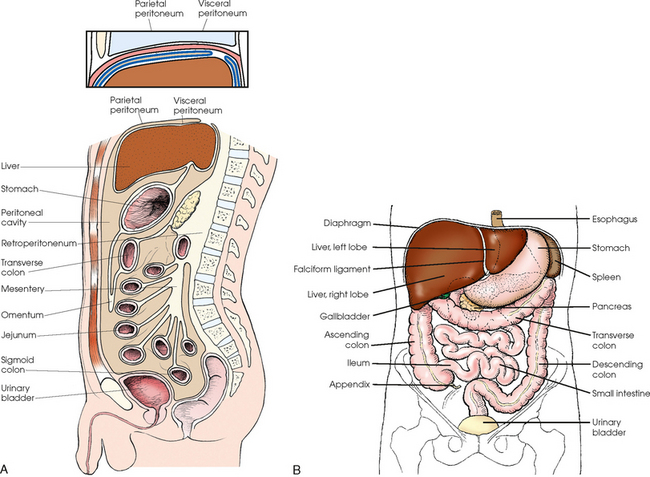
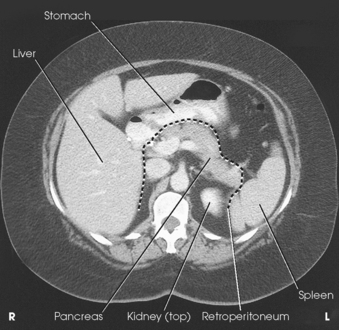
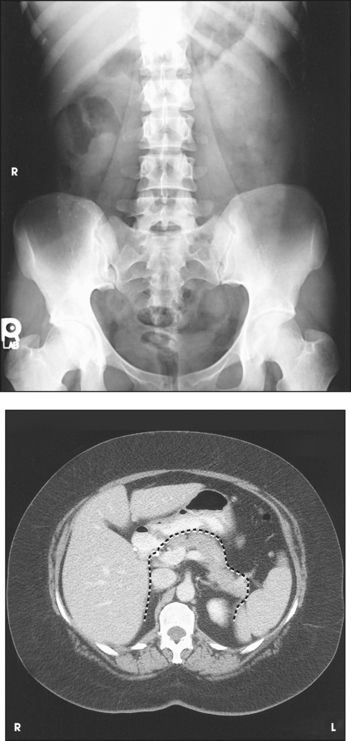
16 The abdominopelvic cavity is enclosed in a double-walled seromembranous sac called the peritoneum. The outer portion of this sac, termed the parietal peritoneum, is in close contact with the abdominal wall, the greater (false) pelvic wall, and most of the undersurface of the diaphragm. The inner portion of the sac, known as the visceral peritoneum, is positioned over or around the contained organs. The peritoneum forms folds called the mesentery and omenta, which serve to support the viscera in position. The space between the two layers of the peritoneum is called the peritoneal cavity and contains serous fluid (Fig. 16-1). Because there are no mesenteric attachments of the intestines in the pelvic cavity, pelvic surgery can be performed without entry into the peritoneal cavity. The retroperitoneum is the cavity behind the peritoneum. Organs such as the kidneys and pancreas lie in the retroperitoneum (Fig. 16-2). In examinations without a contrast medium, it is imperative to obtain maximal soft tissue differentiation throughout the different regions of the abdomen. Because of the wide range in the thickness of the abdomen and the delicate differences in physical density between the contained viscera, it is necessary to use a more critical exposure technique than is required to show the difference in density between an opacified organ and the structures adjacent to it. The exposure factors should be adjusted to produce a radiograph with moderate gray tones and less black-and-white contrast. If the kilovolt peak (kVp) is too high, the possibility of not showing small or semiopaque gallstones increases (Fig. 16-3, A). Sharply defined outlines of the psoas muscles, the lower border of the liver, the kidneys, the ribs, and the transverse processes of the lumbar vertebrae are the best criteria for judging the quality of an abdominal radiograph (Fig. 16-3, B). • To prevent muscle contraction caused by tension, adjust the patient in a comfortable position so that he or she can relax. • Explain the breathing procedure, and ensure the patient understands exactly what is expected. • If necessary, apply a compression band across the abdomen for immobilization but not compression. • Do not start the exposure for 1 to 2 seconds after the suspension of respiration to allow the patient to come to rest and involuntary movement of the viscera to subside. Voluntary motion produces a blurred outline of the structures that do not have involuntary movement, such as the liver, psoas muscles, and spine. Patient breathing during exposure results in blurring of bowel gas outlines in the upper abdomen as the diaphragm moves (Fig. 16-4). Involuntary motion caused by peristalsis may produce either a localized or a generalized haziness of the image. Involuntary contraction of the abdominal wall or the muscles around the spine may cause movement of the entire abdominal area and produce generalized radiographic haziness.
ABDOMEN
Abdominopelvic Cavity
Abdominal Radiographic Procedures
IMMOBILIZATION
ABDOMEN