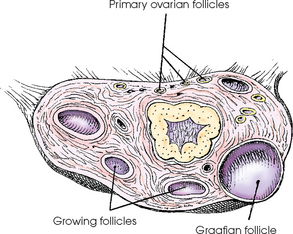
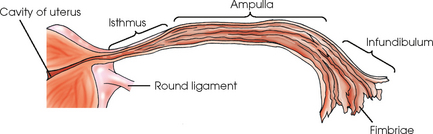
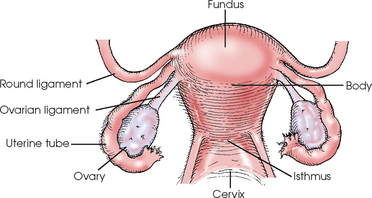
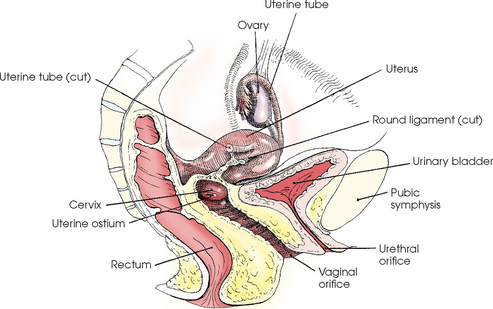
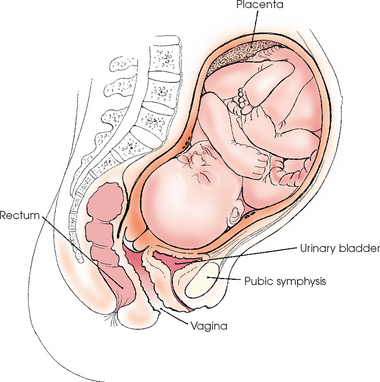
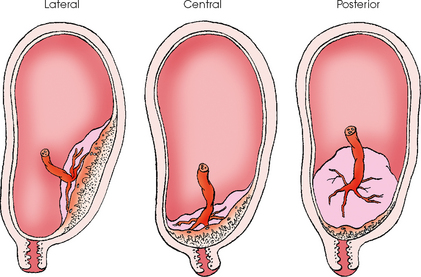
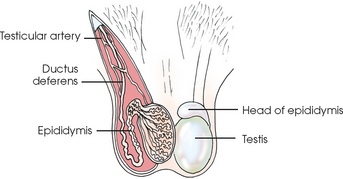
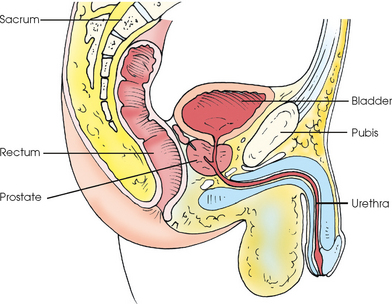
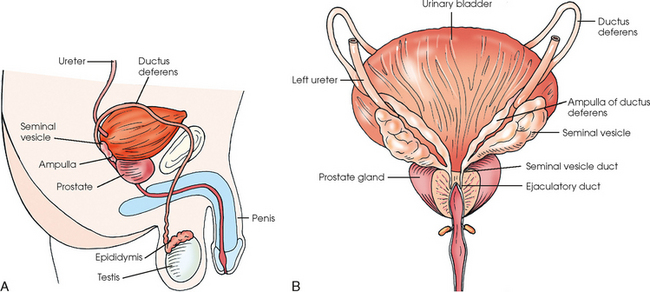
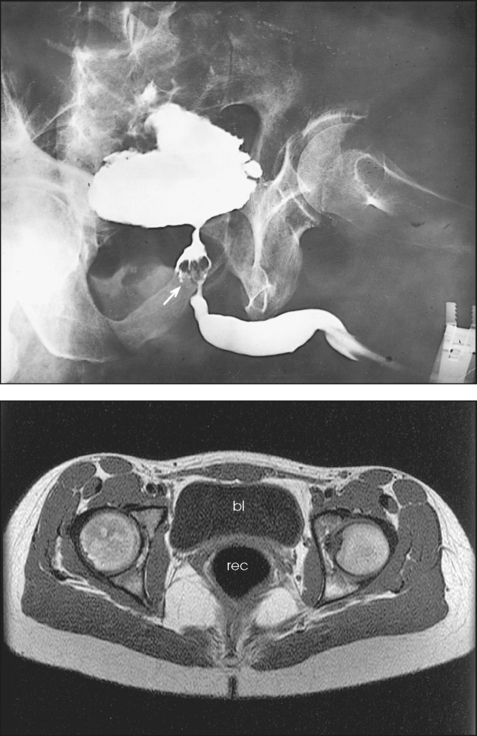
19 The two ovaries are small, glandular organs with an internal secretion that controls the menstrual cycle and an external secretion containing the ova, or female reproductive cells (Fig. 19-1). Each ovary is shaped approximately like an almond. The ovaries lie one on each side, inferior and posterior to the uterine tube and near the lateral wall of the pelvis. They are attached to the posterior surface of the broad ligament of the uterus by the mesovarium. The two uterine tubes, or fallopian tubes, arise from the lateral angle of the uterus, pass laterally above the ovaries, and open into the peritoneal cavity. These tubes collect ova released by the ovaries and convey the cells to the uterine cavity. Each tube is 3 to 5 inches (7.6 to 13 cm) long (Fig. 19-2) and has a small diameter at its uterine end, which opens into the cavity of the uterus by a minute orifice. The tube itself is divided into three parts: the isthmus, the ampulla, and the infundibulum. The isthmus is a short segment near the uterus. The ampulla comprises most of the tube and is wider than the isthmus. The terminal and lateral portion of the tube is the infundibulum and is flared in appearance. The infundibulum ends in a series of irregular prolonged processes called fimbriae. One of the fimbriae is attached either to or near the ovary. The uterus is a pear-shaped, muscular organ (Figs. 19-3 and 19-4). Its primary functions are to receive and retain the fertilized ovum until development of the fetus is complete and, when the fetus is mature, to expel it during birth. During the implantation process, the fertilized ovum, called a zygote, is passed from the uterine tube into the uterine cavity, where it adheres to and becomes embedded in the uterine lining. About 2 weeks after fertilization of the ovum, the embryo begins to appear. The embryo becomes a fetus 9 weeks after fertilization and assumes a human appearance (Fig. 19-5). The fertilized ovum usually becomes embedded near the fundus of the uterine cavity, most frequently on the anterior or posterior wall. Implantation occasionally occurs so low, however, that the fully developed placenta encroaches on or obstructs the cervical canal. This condition results in premature separation of the placenta, termed placenta previa (Fig. 19-6). The testes are ovoid bodies averaging 1½ inches (3.8 cm) in length and about 1 inch (2.5 cm) in width and depth (Fig. 19-7). Each testis is divided into 200 to 300 partial compartments that constitute the glandular substance of the testis. Each compartment houses one or more convoluted, germ cell–producing tubules. These tubules converge and unite to form 15 to 20 ductules that emerge from the testis to enter the head of the epididymis. The ductus deferens is 16 to 18 inches (40 to 45 cm) long and extends from the tail of the epididymis to the posteroinferior surface of the urinary bladder. Only its first part is convoluted. From its beginning, the ductus deferens ascends along the medial side of the epididymis on the posterior surface of the testis to join the other constituents of the spermatic cord, with which it emerges from the scrotal sac and passes into the pelvic cavity through the inguinal canal (Fig. 19-8). Near its termination, the duct expands into an ampulla for the storage of seminal fluid and then ends by uniting with the duct of the seminal vesicle. The two seminal vesicles are sacculated structures about 2 inches (5 cm) long (Fig. 19-9). They are situated obliquely on the lateroposterior surface of the bladder, where, from the level of the ureterocystic junction, each slants inferiorly and medially to the base of the prostate. Each ampulla of the ductus deferens lies along the medial border of the seminal vesicle to form the ejaculatory duct. The prostate, an accessory genital organ, is a cone-shaped organ and averages 1¼ inches (3.2 cm) in length. The prostate encircles the proximal portion of the male urethra and, extending from the bladder neck to the pelvic floor, lies in front of the rectal ampulla approximately 1 inch (2.5 cm) posterior to the lower two thirds of the pubic symphysis (see Fig. 19-9). The prostate comprises muscular and glandular tissue. The ducts of the prostate open into the prostatic portion of the urethra.
REPRODUCTIVE SYSTEM
Female Reproductive System
OVARIES
UTERINE TUBES
UTERUS
FETAL DEVELOPMENT
Male Reproductive System
TESTES
DUCTUS DEFERENS
SEMINAL VESICLES
PROSTATE
Radiology Key
Fastest Radiology Insight Engine