Abdominal Aorta and Branches
The abdominal aorta begins at the aortic hiatus of the diaphragm, anterior to and at the level of the lower portion of the 12th thoracic vertebra, descending slightly lateral to the midline and in close relation to the vertebral bodies, ending at the 4th lumbar vertebra. At that point, it bifurcates into two common iliac arteries forming an angle of 37°. The abdominal aorta reduces the diameter rapidly because the branches are large and numerous (Figs. 18.1, 18.2).
The aorta is in contact, anteriorly with the celiac plexus and the lesser sac or omental bursa, and the pancreatic body with the splenic vein attached posteriorly. Behind the pancreas, between the superior mesenteric artery and the aorta, is the left renal vein in close association with the anterior wall of the aorta. Below the pancreas is the horizontal part of the duodenum; farther distally, it is covered by the posterior parietal peritoneum and crossed by the oblique parietal attachment of the mesentery. Laterally on the right, the aorta is in contact with the cisterna chyli, and thoracic duct, azygos vein, and right crus of the diaphragm, which separates it from the inferior vena cava. Below the 2nd lumbar vertebra the aorta is in contact with the inferior vena cava, all the way down. Laterally on the left, the aorta is in contact with the crus of the diaphragm and celiac ganglion. At the level of the 2nd lumbar vertebra, there is contact with the duodenojejunal flexure and sympathetic trunk, ascending duodenum, and inferior mesenteric vessels. The bifurcation of the abdominal aorta is projected on the abdominal wall surface at the level of the umbilicus (Figs. 18.3, 18.4, 18.5, 18.6, 18.7, 18.8).
Abdominal Aorta
Branches of the Abdominal Aorta
Ventral
Celiac trunk
Superior mesenteric artery
Inferior mesenteric artery
Lateral
Inferior phrenic artery
Middle suprarenal artery
Renal artery
Testicular or ovarian artery (gonadal)
Dorsal
Lumbar
Median sacral
Terminal
Common iliac
Ventral Branches
Celiac Trunk
It is the first wide ventral branch of the aorta, 1.5 cm long, arising just below the aortic diaphragmatic hiatus (Figs. 18.9, 18.10). It is generally horizontal and oriented forward, but may be caudally or cranially oriented (Figs. 18.11, 18.12, 18.13, 18.14, 18.15). It may give off the inferior phrenic arteries before the origin of the left gastric artery. In approximately 50% of the population, the celiac trunk follows the standard pattern. A celiac trunk may be absent in 0.4% to 2.5% of the population.
Branches
Left gastric artery
Hepatic artery
Common hepatic artery
Gastroduodenal artery
Pancreaticoduodenal arcades
Right gastroepiploic artery
Hepatic artery proper
Right gastric artery
Cystic artery
Arteries of the liver
Segmental branches
Microscopic hepatic structure
Terminal hepatic artery
Hepatic arterial collaterals
Variations of the hepatic artery
Splenic Artery
Arteries of the pancreas
Pancreaticoduodenal arcades
Dorsal pancreatic artery
Arteria pancreatica magna
Arteria caudae pancreatis
Short gastric arteries
Posterior gastric artery
Left gastroepiploic artery
Terminal splenic branches
Segmental splenic branches
Variations of the celiac trunk
Left Gastric Artery
This is the smallest celiac branch. The origin of the left gastric artery (LGA) may be in the aorta, close to the celiac trunk, or at the cranial aspect of the celiac trunk, all the way, from the ostium to the bifurcation creating a real trifurcation. It ascends cranially to the left, behind the oriental bursa, to the upper end of the stomach. After giving off distal esophageal branches and branches to the gastric fundus, the artery turns anteroinferiorly into the left gastropancreatic fold, running along the gastric lesser curvature, reaching the pylorus, supplying both gastric walls (anterior and posterior), and ends with an anastomoses with the right gastric artery (Figs. 18.16, 18.17). The left gastric artery may give origin to the left hepatic artery, or an accessory left gastric artery may arise from the left hepatic artery (Figs. 18.18, 18.19. 18.20, 18.21, 18.22). At the gastric fundus, there are anastomoses with the splenic artery through the short gastric arteries (Fig. 18.23).
Hepatic Artery
In the adult, the hepatic artery is smaller than the splenic artery, but larger than the left gastric artery. It originates from the bifurcation of the celiac trunk, directed forward and to the right, toward the porta hepatis, where it divides in the right and left branches to the hepatic lobes (Fig. 18.10). The artery is subdivided in common hepatic artery from the celiac trunk to the origin of the gastroduodenal artery and hepatic artery proper. It is called the hepatic artery proper, from the gastroduodenal artery to the bifurcation into right and left hepatic branches (Fig. 18.12). The common hepatic artery may be extremely short or may not exist at all (Fig. 18.15). The proper hepatic artery may not exist at all (Fig. 18.11) and may be part of a trifurcation of the common hepatic artery. The hepatic artery may arise from the superior mesenteric artery (replaced hepatic artery). The right hepatic branch may arise from the superior mesenteric artery, whereas the left hepatic branch may originate from the left gastric artery. See Variations of the Hepatic Artery at the end of this section.
Common Hepatic Artery
Gastroduodenal Artery
The gastroduodenal artery arises from the hepatic artery, characterizing the beginning of the hepatic artery proper (Figs. 18.24, 18.25). It is short and large, descending between the duodenum and neck of the pancreas. It may be located at the left aspect or anteriorly to the bile duct. The gastroduodenal artery has three constant branches: the posterior and anterior pancreaticoduodenal arcades, the terminal branch, and the right gastroepiploic artery (Figs. 18.26, 18.27). The gastroduodenal artery may be duplicated, or the pancreaticoduodenal arcades may arise from the common hepatic artery (Fig. 18.28).
Posterior Pancreaticoduodenal Arcade (PPDA)
This artery is part of a rich vascular network to the head of the pancreas, uncinate process, and duodenal bulb, together with the anterior pancreaticoduodenal arcade. The PPDA arises 1 to 2 cm from the origin of the gastroduodenal artery in 78% of the cases, but the superior origin may also arise from various branches from the hepatic artery in 15% of the cases, or the superior mesenteric artery in 5% of the cases. It is also called the retroduodenal artery or posterior superior pancreaticoduodenal artery. The retroduodenal artery may become very prominent, tracking along the common hepatic duct (Fig. 18.29). The PPDA gives branches to the duodenum (to the right) and the head of the pancreas (to the left). The pancreatic branches anastomose freely with arteries in the head of the pancreas, anterior pancreaticoduodenal arcade, supraduodenal artery, and dorsal pancreatic artery (Figs. 18.26, 18.27). The arcades are frequently multiple with two, three, and four branches. The lower part of the bile duct has the main blood supply from the posterior pancreaticoduodenal arcade.
Anterior Pancreaticoduodenal Arcade
Along with the right gastroepiploic artery, the anterior pancreaticoduodenal arcade is a terminal branch of the gastroduodenal artery. It is also called the superior pancreaticoduodenal or anterior superior pancreaticoduodenal artery and may give a pyloric branch and have distal anastomoses with the superior mesenteric artery or the inferior pancreaticoduodenal artery. The anterior arcade has free communications with the posterior arcade and dorsal pancreatic and transverse pancreatic arteries (Figs. 18.26, 18.27, 18.30). The middle colic artery may also have anastomoses with the anterior pancreaticoduodenal arcade.
Right Gastroepiploic Artery
This artery is the terminal branch of the gastroduodenal artery, and is the main artery of the stomach (Figs. 18.31, 18.32). It follows a winding course along the greater curvature of the stomach and gives off an ascending pyloric branch and several ascending gastric branches, which anastomose with descending branches of the right and left gastric arteries. Several omental branches are also originated from the right gastroepiploic artery. The right and left omental branches form an anastomotic arcade at the greater omentum and have anastomoses with the posterior omental branches from the transverse mesocolon. The gastroepiploic artery reaches and anastomoses with the left gastroepiploic artery, where it ends (Figs. 18.33, 18.34, 18.35, 18.36, 18.37).
Other Branches
Less constant branches are occasionally seen, including the right gastric artery, the transverse pancreatic artery, accessory cystic artery, and supraduodenal artery.
Right Gastric Artery
This artery arises from any site at the hepatic artery, before or after the gastroduodenal artery. It anastomoses with the left gastric artery (Fig. 18.38, Fig. 18.19).
Cystic Artery
This artery usually arises from the right branch of the hepatic artery. It divides into superficial and deep branches. It may originate from the hepatic artery itself at many levels or other arteries such as the gastroduodenal artery. It crosses over (anteriorly) the common bile duct reaching the gallbladder. An accessory cystic artery may be
present and arise from the common hepatic artery or one of its branches. Small branches of the cystic artery may enter the liver parenchyma in the gallbladder bed. The cystic artery arises from the right hepatic artery in 63.9% of the cases, from the hepatic trunk in 26.9% of the cases, from left hepatic artery in 5.5% of the cases, from the gastroduodenal in 2.6% of the cases, from the superior pancreaticoduodenal arcade in 0.3% of the cases, and directly from the superior mesenteric artery in 0.8% of the cases. (Figs. 18.39).
present and arise from the common hepatic artery or one of its branches. Small branches of the cystic artery may enter the liver parenchyma in the gallbladder bed. The cystic artery arises from the right hepatic artery in 63.9% of the cases, from the hepatic trunk in 26.9% of the cases, from left hepatic artery in 5.5% of the cases, from the gastroduodenal in 2.6% of the cases, from the superior pancreaticoduodenal arcade in 0.3% of the cases, and directly from the superior mesenteric artery in 0.8% of the cases. (Figs. 18.39).
Supraduodenal Artery
The supraduodenal artery has been described as a distinctive artery that allows for the surgical mobilization of the horizontal segment of the duodenum. The supraduodenal artery is probably present in more than 90% of the population, but with a high degree of variation in its origin. It provides blood supply to the distal upper two thirds of the duodenum, with connections to the proximal small bowel (Fig. 18.40). When this artery is absent, it may arise as multiple vessels from the right gastric artery. The supraduodenal artery has been reported to originate from the gastroduodenal artery in 27% of the cases, from the common hepatic artery in 20% of the cases, from the left hepatic artery in 20% of the cases, the right hepatic artery in 13%, and from the cystic artery in 10% of the cases. It may also participate in the blood supply of the extrahepatic bile ducts.
Arteries of the Liver
Hepatic Artery
In the adult individual, the hepatic artery is intermediate in size between the left gastric and splenic arteries. However, in fetal life and early postnatal life it is the largest celiac branch. It has a forward direction and curves to the right, below the epiploic foramen to the upper aspect of the superior part of the duodenum. Crossing anteriorly the portal vein, and roughly parallel, but to the left of the common bile duct, it ascends between layers of the lesser omentum, anterior to the epiploic foramen, to the porta hepatis, where it divides into the right and left branches to the hepatic lobes, accompanying the ramifications of the portal vein and hepatic ducts, within the portal space. The segments of the hepatic artery have been described in the preceding text (Fig. 18.41). Several intra- and extrahepatic branches of the hepatic arteries are identified, including the right gastric artery, the cystic artery, rami to the bile ducts and connections with the supraduodenal artery, and retroduodenal artery.
Interlobar Communicating Arcades
Redman and Reuter, first demonstrated the existence of interlobar collateral vessels angiographically and described them as preexisting small arterial communications present in the hilum of most cases. Despite the description of interlobar communications by other authors only recently, Tohma et al. described systematically the presence of communicating arcades (CAs) between the right and left hepatic arteries in more than 85% of the cases and proposed a classification (Figs. 18.42, 18.43, 18.44). On the left side, the CAs originated from the segment IV artery (type 1) in 62% of the cases. The CAs originated from the left hepatic artery (type 2) in 38% of the cases (Fig. 18.44). On the right side, the CAs originated from the right anterior hepatic artery (type 1) in 46% of the cases and from the right hepatic artery (type 2) in 15% of the cases (Fig. 18.45). In 38% of the cases, the CAs originated from both the right hepatic artery and the right anterior hepatic artery (type 3). The CAs bifurcated off two branches to the caudate lobe in 18% of the cases and one branch in 45% of the cases. No caudate branches were observed in the remaining 36% of the cases. The CAs are located extrahepatically cranial to the portal vein bifurcation, close to the hilar bile duct (Fig. 18.46).
Embryologic Aspects
The biliary and hepatic systems have a complex embryologic origin, which causes a significant number of variations and adaptations to the flow patterns. As the embryologic duodenal diverticulum migrates toward the liver hilum carrying the extrahepatic bile ducts, it is supplied by multiple arteries to maintain adequate perfusion for the developing system. These vessels originate from the aorta, celiac trunk, and superior mesenteric artery. The formation of the intrahepatic bile ducts has been suggested, to be dependent upon contact between the developing embryonic liver mass and the preformed extrahepatic duct system, which carries the arteries with it. As the biliary system matures, many of the vessels are resorbed or incorporated into the main arterial bed. However, the resorption and incorporation is variable and multiple arterial patterns develop. Therefore, only 57% to 61% of the population has what is considered the “standard” hepatic arterial perfusion pattern. The presence of significant variations in the hepatic artery anatomic arterial perfusion creates in later life the so-called replaced arteries, which do not correspond to the classical anatomy and perfuse a complete vascular bed. An accessory artery is a secondary artery that contributes to the perfusion of the vascular arterial bed in addition to the conventional anatomic arteries (see “Variations of the Hepatic Artery” in subsequent text).
Other Branches and Connections of the Hepatic Artery
Falciform Artery
Falciform Artery
The falciform ligament divides the medial and lateral segments of the left lobe of the liver and connects the liver to the diaphragm and the supra-umbilical part of the anterior abdominal wall. Its free edge contains the ligamentum teres and the small para-umbilical veins, and the falciform artery. The falciform artery originates from the middle hepatic artery (when present) and the left hepatic artery. The angiographic incidence of the falciform artery varies from 2% to 25%, but in postmortem dissections, it is identified in as many as 67% of the cases (Fig. 18.47). The terminal branches of the falciform artery are connected to the network of the
phrenic arteries, internal mammary artery, and superior epigastric artery (Fig. 18.48).
phrenic arteries, internal mammary artery, and superior epigastric artery (Fig. 18.48).
Middle Hepatic Artery
The middle hepatic artery or segment IV artery is not considered an anatomic variation, although it may serve as an exclusive supplier for the segment IV of the liver. It may also be the origin of the falciform artery, the right gastric artery, and the accessory left gastric artery. It may arise from the proximal right hepatic artery or from the proper hepatic as an independent artery forming a trifurcation.
Hepatic–Phrenic Artery Connections
The hepatic arteries, particularly the left hepatic artery may develop free communications with the phrenic arterial system. Peripheral hepatic tumors, inflammatory processes of the subphrenic space and base of the lungs, may develop multiple connections, particularly from the bare area of the liver surface. Occasionally a phrenic artery arises directly from the left hepatic artery (Fig. 18.49).
Segmental Anatomy of the Liver
The intrahepatic arteries follow a segmental distribution (Figs. 18.50, 18.51). The division of the liver into segments is delineated by fissures and the distribution of the vascular and ductal structures. The three main hepatic veins divide the liver into four sectors, each of which receives a portal pedicle, with an alternation between hepatic veins and portal pedicles. Of the four fissures, only one is represented superficially—the portoumbilical fissure. The other three fissures are related to the three large hepatic veins, but not apparent in the liver surface.
Right Fissure
This fissure commences at the right margin of the inferior vena cava and follows the attachment of the right superior coronary ligament to about 3 to 4 cm from the junction of the latter with the right inferior layer. The fissure then curves anteriorly to a point on the inferior margin about midway between the gallbladder fossa and the right margin of the liver. Passing posteriorly, the fissure follows a line that runs parallel to the gallbladder fossa and crosses the caudate process to reach the right side of the inferior vena cava. Lying almost in the coronal plane, the fissure contains the right hepatic vein, with branches passing anteriorly to segments V and VIII and posteriorly to segments VI and VII (Figs. 18.50, 18.51).
Median Fissure (Main Portal Fissure, also called Cantlie’s Line)
This fissure passes from the gallbladder fossa to the left margin of the inferior vena cava. Posteroinferiorly, this fissure is represented by a line from the gallbladder fossa to the main bifurcation of the hepatic pedicle (portal triad) and, then, to the retrohepatic inferior vena cava (Figs. 18.50, 18.51).
Left Fissure (Left Portal Fissure)
This fissure runs from the left side of the inferior vena cava to a point between the dorsal one third and ventral two thirds of the left margin of the liver; it divides the left liver into two sectors: anterior and posterior, separating the segments III and II. It is not the umbilical fissure. Inferiorly, the fissure passes to the commencement of the ligamentum venosum (Figs. 18.50, 18.51).
Portoumbilical Fissure (or Umbilical Fissure)
This fissure is marked superficially by the attachment of the falciform ligament, which contains the ligamentum teres hepatis in its inferior border. Angled less generously than the right fissure, it meets the inferior margin of the liver at an angle of about 50°.
The liver is divided into right and left lobes, separated by the main portal fissure or median fissure (projection of the path of the middle hepatic vein upon the liver surface). The portal fissure runs from the medial side of the inferior vena cava to the middle of the gallbladder bed. The right lobe is vascularized by the right hepatic artery and the left lobe is fed by the left hepatic artery. The hepatic lobes are divided in sectors. The right lobe has an anterior and a posterior sector (also called anteromedial and posterolateral), separated by the right portal fissure (projection of the path of the right hepatic vein upon the liver surface). The left lobe has a lateral (left) and a medial sector (right), separated by the falciform ligament and portoumbilical fissure (partial projection of the path of the involuted umbilical vein, called round ligament) (Figs 18.50, 18.51, 18.52).
Hepatic Segments
The caudate lobe is an independent segment, supplied by the right and left hepatic artery and portal vein. It is called segment I and has venous drainage directly into the inferior vena cava. It is also called lobule of Spiegel. It is considered to be part of the left hepatic lobe (segment I of the left lobe) for surgical purposes. The caudate lobe is connected to the right lobe by a narrow bridge called the caudate process, behind the porta hepatis. Below and to the left, there is a small round appendage called the papillary process, which sometimes covers completely the inferior vena cava bridging the caudate lobe to the right liver lobe (Fig. 18.53A-D).
The left hepatic lobe is further subdivided into three segments. The lateral sector is divided into segment II and segment III by the left portal fissure (projection of the path of the left hepatic vein upon the surface of the left lobe of the liver). Segment II is posterior and superior, and segment III is inferior and anterior (Figs. 18.54, 18.55). The medial sector of the left lobe is segment IV. It has a cuneiform format, with the base turned anteriorly. It may be subdivided into a cranial and a caudal part, also called segments IVa and IVb. Segment IVa is also called the quadrate lobe of the liver (Fig. 18.56).
The right hepatic lobe is subdivided into four segments. The anterior sector is divided in segment VIII and segment V. Segment VIII is superior and segment V is inferior (Figs. 18.57, 18.58). The posterior sector is divided in segment VI and segment VII. Segment VI is inferior and segment VII is superior. The posterior sector is posterior and more lateral than the anterior sector (Figs. 18.59, 18.60).
The segments of the liver, either at the left or the right hepatic lobes, follow a clockwise distribution. The hepatic artery, the bile ducts, and the portal vein branches run in the center of the hepatic segments, whereas the hepatic veins run within the fissures between the segments. The fissures of the liver cannot be seen at the liver surface, except at the umbilical fissure, due to the presence of the falciform ligament and round ligament (ligamentum teres) (Figs. 18.50, 18.51, 18.52).
Microscopic Hepatic Structure
The classic hepatic lobules are polyhedral structures (hexagonal in histologic sections), about 1 mm in diameter, with a small central vein as a central axis, surrounded by portal triads (Fig. 18.61). Each triad contains a branch of the portal vein, a hepatic artery, a lymphatic vessel, and an interlobular biliary ductule. The portal triad is sheathed by connective tissue, called the portal canal or perivascular fibrous capsule, surrounded by the limiting plate, having in between the space of Mall. In humans, the idea of a functional unit has been proposed instead because the hepatic lobules are not readily perceptible. The functional unit is the portal lobule, consisting of parts of at least three neighboring classic lobules, bile from which drains into a biliary ductule in the portal canal between three such hepatic lobules. Again, the section shows a portal lobule as a polygonal area, centered on a portal triad, with boundaries passing through adjacent central veins. The concept of a portal acinus is more useful considering metabolic organization. The portal acinus is centered on a preterminal branch of a hepatic arteriole and includes the hepatic tissue served by this, and its boundaries are limited by the territory of other acini and by two adjacent central veins (Fig. 18.62). The acinus has been divided into three zones: zone 1 (periportal), zone 2, and zone 3 (close to the central venous drainage). Zone 3 (in the circulatory periphery and close to the central vein) suffers most from injury, developing bridging necrosis. Zone 1, close to the afferent vessels, survives longer and may trigger the regeneration of the liver (Figs. 18.61, 18.62, 18.63).
Portal Space
Portal areas, also called portal triads or portal canals, are located at the corners of the liver lobules. Portal spaces are surrounded by much larger areas with hepatic cords and sinusoids. Each portal space contains three (hence the term portal triad) more-or-less conspicuous tubular structures wrapped together in connective tissue. The tubular structures are branches of the bile duct, the portal vein, and the hepatic artery (Fig. 18.64). There are two less conspicuous structures within the portal space, a nerve and a lymphatic channel, but usually these are not apparent in routine specimens. The portal vein brings much more blood to the liver than does the hepatic artery; each branch of the portal vein is typically much larger than the associated branch of the hepatic artery. The relative sizes of the paired vessels in a portal area thus differ from those of a typical vein–artery pair in other parts of the body, where the artery delivers the same volume of blood that the vein subsequently returns. The portal vein branches, within the portal space arise at right angles to the main axis of the portal vein in a radial fashion. Direct connections with the sinusoids are provided by the inlet venules (Fig. 18.65). The artery and bile ducts occupy the periphery of the portal space, but the artery and the bile duct may be multiple. Between stroma and hepatocytes, there is a small space, called space of Mall—one of sites where lymph originates.
Terminal Hepatic Artery
The hepatic artery ramifies parallel with the portal vein branches and bile ducts. Arterioles are released into the lobular parenchyma and terminate at different levels of the lobule, providing arterial blood flow to zone 1 of the acinus through anastomoses with the portal venule inlet (Fig. 18.66). Much like the bronchial arteries that provide bronchial circulation and pulmonary arterial anastomosis in the lungs, in the liver, the main circulatory arterial flow is provided to the periportal area by arterial branches directly to the peribiliary plexus and to the bile duct. Subsequently and to a much lesser extent, the artery provides nutrition to the acinus and to the liver parenchyma itself through the anastomosis of the arterioles with the portal inlet venule. In fact, due to importance of the hepatic artery to the bile ducts, the hepatic artery should be called biliary artery (Fig. 18.67).
According to Lunderquist, there are four types or levels of arterioportal communications: (1) the peribiliary plexus; (2) the terminal arterioloportal anastomosis connecting to the sinusoids; (3) the vasa vasorum on the wall of the portal vein; and (4) the direct arterioportal communications. The vasa vasorum of the wall of the portal vein is provided by direct small branches from the hepatic artery (Fig. 18.68). There are two concentric vascular layers within the wall of the larger bile duct, constituting the peribiliary plexus. The inner layer is a capillary plexus present in the submucosa, which drains into the outer adventitial venous plexus. The latter opens directly into the hepatic sinusoids via the lobular vein or into the portal vein via the interlobular vein (Figs. 18.69, 18.70). The intrahepatic bile duct is supplied by the hepatic arterial branches, which form the peribiliary plexus, whereas the extrahepatic bile duct receives its arterial nutrition from various sources, but most commonly from branches of the gastroduodenal artery.
According to Ekataksin, unlike the portal vein which exclusively supplies sinusoids, the hepatic artery supplies five compartments: (1) peribiliary plexus, (2) portal tract interstitium, (3) portal venous vasa vasorum, (4) fibrous capsule of Glisson, and (5) central sublobular-hepatic venous vasa vasorum, which subsequently either secondarily flows through the lobules or directly drains into the hepatic vein.
Within the portal tract, the arterial bed forms distinct collecting vessels, forming a portal system, the so-called hepatic artery-derived portal system, which anastomoses
with and/or follows or joins the vein–venule to open at the lobular periphery.
with and/or follows or joins the vein–venule to open at the lobular periphery.
Outside the portal tract, the hepatic artery departs from the tract as an “isolated artery” directed toward the two compartments: the Glisson capsule and the central sublobular-hepatic venous vasa vasorum. The capsular arteriole that eventually drains into the local subcapsular lobules is likely to be misinterpreted as evidence of the hepatic artery being a primary feeder of sinusoids. The hepatic venous vasa vasorum that immediately drains into the respective hepatic vein without passing through lobular sinusoids is a hitherto unrecognized, but occasionally suspected, unusual pathway, a “bypass artery.” There are multiple peripheral communications between the hepatic artery and the portal vein radicles, especially in pathologic contexts, such as in liver cirrhosis, when the arterioportal shunts are widely open, contributing therefore to the increase in the portal vein pressure levels and promoting hepatofugal flow in the intrahepatic portal branches (Fig. 18.71). The cirrhotic nodules reduce significantly the number of sinusoids and perinodular shunts develop. The cirrhotic nodule develops a central feeding artery or group of feeding arteries, visible in a central bundle (Fig. 18.72).
To facilitate description, the biliary duct has been divided into three segments, namely hilar (right and left ducts), supraduodenal (common hepatic duct and upper common bile duct), and retropancreatic (lower common bile duct).
The arterial supply of the hilar bile duct (right and left) is provided by direct numerous small branches from the right and left hepatic arteries that form a rich network on the surface of the ducts in continuity with the plexus around the supraduodenal duct (Fig. 18.73).
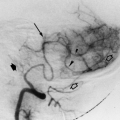
The arterial supply of the supraduodenal bile duct is essentially axial, and most arteries arise from named arteries related to its upper and lower ends. The main vessels rim along the lateral aspects of the duct. According to Terblanche, these vessels are named 3 o’clock and 9 o’clock arteries and most commonly originate from the posterior pancreaticoduodenal arcade and gastroduodenal artery. Approximately 60% of the vessels supplying the supraduodenal duct run upward from vessels below, whereas 38% run downward from the right hepatic and other arteries. Only 2% of the supply is nonaxial, arising from the common or proper hepatic artery. The 3 o’clock and 9 o’clock arteries give branches to the duct forming the pericholedocal plexus (Figs. 18.35, 18.73, 18.74, 18.75, 18.76, 18.77).
An additional supply to the supraduodenal bile duct may be the retroportal artery, arising from the celiac trunk or superior mesenteric artery close to the origin of these vessels from the aorta. This artery courses to the right, behind the portal vein and to the back of the head of the pancreas, reaching the lower end of the supraduodenal duct. This artery may end, joining the posterior pancreaticoduodenal arcade, close to the distal supraduodenal duct, giving off small branches to the posterior surface of the duct (type I pattern). In one third of cases, the retroportal artery passes upward on the back of the supraduodenal duct, reaching the right hepatic artery (type II pattern). The retroportal artery along its route gives branches to join the pericholedocal plexus (Fig. 18.74).
The retropancreatic bile duct is supplied by direct small branches from the posterior pancreaticoduodenal artery or gastroduodenal artery, forming a mural plexus (Fig. 18.73). More recently (1999), Vellar described the presence of a 12 o’clock marginal artery in a smaller number of individuals, joining the plexus on the posterior surface of the common hepatic duct, in addition to the previously described 3 o’clock and 9 o’clock arteries.
The hilar plexus: The hilar plate is a condensation of connective tissue, which lines the hilum of the liver and forms a roof over the contents of the hilum, separating these structures from the hepatic substance. The right and left hepatic ducts have an intimate relation to the hilar plate. Bridging between the branches of the left hepatic artery and the right hepatic artery are a number of collateral vessels, which are found on the inferior surface of the hilar plate and which form the hilar plexus. The hilar arterial plexus is not only involved in the blood supply of the confluence of the bile ducts and the right and left hepatic ducts and, therefore, in communication with the arterial plexus over the biliary system, but it is the most important collateral between the right hepatic artery and its branches and the left hepatic artery and its branches, and the same communicating arcade described by Tohma et al. in 2005. Branches from the hilar plexus supply the caudate lobe and process. The caudate lobe is an important bridge for collateral blood flow between the right and left sides of the liver. It is suggested in the literature that the caudate lobe takes its blood supply not only from the segment I artery, but also from the communicating arcade. This may be the reason that transcatheter arterial chemoembolization is often not an especially effective treatment for hepatocellular carcinomas in the caudate lobe. According to that description the arterial branches from the hilar plate ascend posterior to the right and left hepatic ducts (Fig. 18.77). It is supposed that the communicating artery may exist as a marginal artery for the hilar bile duct and connect the parabiliary arteries to form the parabiliary arterial network that supplies the biliary tract, as well as the 3 o’clock and 9 o’clock arteries (from the porterior-superior pancreaticoduodenal arcade), which exist as marginal arteries for the common bile duct.
Hepatic Arterial Collaterals
There are 26 known potential collateral pathways for the arterial supply of the liver. They may be classified as intrahepatic collaterals (Fig. 18.78) and extrahepatic collaterals (Fig. 18.79).
Intrahepatic Collaterals (Fig. 18.78)
Perivascular
Interlobar or intersegmental
Intralobar or intrasegmental
Vasa vasorum of the portal veins and hepatic veins
Peribiliary plexus
Extrahepatic Collaterals (Fig. 18.79)
Pancreaticoduodenal arcades
Inferior pancreaticoduodenal artery
Dorsal pancreatic artery
Arc of Bühler (Fig. 18.80)
Periportal route
Common bile duct collaterals
Retroduodenal or supraduodenal artery
Cystic artery
Right branches of dorsal pancreatic artery
Multiple unnamed branches in the porta hepatis
Left gastric route
Left gastric to right gastric anastomosis
Left gastric to left hepatic via lesser omentum
Inferior phrenic route
Right inferior phrenic artery
Left inferior phrenic artery
Right paracolic gutter route
Branches from middle or right colic artery
Direct adhesions to hepatic flexure
Omental branches
Internal mammary and superior epigastric artery
Intercostal and lumbar artery
Capsular branches of the right renal artery
Variations of the Hepatic Artery
In more than 40% of cases, the origin and course of the hepatic arteries (Fig. 18.81) vary. Two concepts must be defined. The “replaced” artery originates from a different vessel, related to the standard description and substitutes the typical vessel. The “accessory” artery is an additional vessel to the originated according to the standard description.
Type 1
Type 1 is a replacement of the common hepatic artery, arising from the superior mesenteric artery. The replaced common hepatic artery passes through or behind the head of the pancreas (Figs. 18.81, 18.82). In 10% of the population, the hepatic artery is replaced; that is, a portion of the hepatic blood supply is from the superior mesenteric artery (SMA). The entire hepatic arterial supply is from the SMA in 2.5% of the cases and from the aorta in 2% of individuals.
Type 2
Type 2 is early bifurcation of a short common hepatic artery in right and left hepatic arteries. The right and left hepatic arteries may originate separately from the celiac trunk. The gastroduodenal artery arises from the right hepatic artery (Fig. 18.81).
Type 3
Type 3 is a replaced right hepatic artery that originates from the SMA and the left hepatic artery taking origin from the celiac trunk (Figs. 18.81, 18.83). This is found in 15% of the population.
Type 4
Type 4 is a replaced left hepatic artery, which is a tributary of the left gastric artery, whereas the right hepatic artery originates from the celiac trunk (Figs. 18.20, 18.21, 18.22, 18.81). It runs within the ligamentum venosum and frequently sends smaller branches to the stomach and esophagus. In 12% to 23% of individuals either a branch of the left hepatic artery or the entire left hepatic artery arises from the left gastric artery.
Type 5
The right and left hepatic arteries arise from the celiac trunk, but there is an accessory right hepatic artery from the SMA. The accessory right hepatic artery is in general the first branch of the SMA, and almost always originates the main cystic or accessory cystic artery. The accessory passes through or behind the head of the pancreas (Fig. 18.81). It occurs in 10% to 31% of the population, with 96% of the cases originating from the SMA and 4% from the pancreaticoduodenal trunk. Rare instances of origin from the phrenic artery or gastroduodenal artery have been encountered.
Type 6
Type 6 is an accessory left hepatic artery arising from the left gastric artery (Fig. 18.81). Found in 8% of the population.
Type 7
Type 7 is an accessory left hepatic artery arising from the right hepatic artery (Fig. 18.81).
Type 8
Right hepatic artery passes anteriorly to the common hepatic bile duct, rather than posteriorly (Fig. 18.81).
Splenic Artery
The splenic artery gives branches to the pancreas, to the stomach, and to the spleen. It originates from the celiac trunk in more than 80% of cases. Normal diameter of the splenic artery is 5.6 mm (±1.3 mm). In situations of hypersplenism the splenic artery may be enlarged three- or fourfold. Most of the arteries feeding the body and tail of the pancreas originate from the splenic artery (Figs. 18.84, 18.85, 18.86).
Arteries of the Pancreas
The pancreas does not have a central hilum like other abdominal organs. It is situated between the celiac trunk and the SMA, receiving the blood supply from several arteries originated from those main trunks (Fig. 18.87). The arteries of the head of the pancreas originate from the gastroduodenal artery, and the arteries of the body and tail originate from the splenic artery, celiac trunk, or common hepatic artery.
Pancreaticoduodenal Arcades
The head of the pancreas is encircled by two arterial arcades: the posterior (retroduodenal artery) and anterior
pancreaticoduodenal arcades, branches of the gastroduodenal artery. The posterior arcade is proximal on the gastroduodenal artery, whereas the anterior arcade is a terminal branch of the gastroduodenal artery, together with the right gastroepiploic artery. The anterior pancreaticoduodenal arcade joins the posterior arcade, behind the head of the pancreas, forming a common trunk called inferior pancreaticoduodenal artery (or trunk), and ending in an anastomosis with the SMA or the first jejunal artery. In a number of cases there is an intermediary pancreaticoduodenal arcade, and in some cases it is not a real arcade but a terminal artery to the pancreatic head (Fig. 18.26, 18.27, 18.28, 18.29, 18.30)
pancreaticoduodenal arcades, branches of the gastroduodenal artery. The posterior arcade is proximal on the gastroduodenal artery, whereas the anterior arcade is a terminal branch of the gastroduodenal artery, together with the right gastroepiploic artery. The anterior pancreaticoduodenal arcade joins the posterior arcade, behind the head of the pancreas, forming a common trunk called inferior pancreaticoduodenal artery (or trunk), and ending in an anastomosis with the SMA or the first jejunal artery. In a number of cases there is an intermediary pancreaticoduodenal arcade, and in some cases it is not a real arcade but a terminal artery to the pancreatic head (Fig. 18.26, 18.27, 18.28, 18.29, 18.30)
Dorsal Pancreatic Artery
The main vessel to the neck and proximal body of the pancreas is the dorsal pancreatic artery (Figs. 18.24, 18.87) (also called superior pancreatic artery, colli, suprema, propria, media, isthmi, or dorsalis, and less correctly the arteria pancreatica magna). The dorsal pancreatic artery arises most commonly from the initial splenic artery but also frequently from the celiac trunk bifurcation (Fig. 18.88) or from the common hepatic artery (Fig. 18.89). Less commonly, it originates from the SMA or from a branch of the SMA (Figs. 18.25, 18.90, 18.91). The dorsal pancreatic artery is commonly connected, in the right aspect, with the anterior pancreaticoduodenal arcade or other gastroduodenal artery branch by an anastomotic branch (prepancreatic arcade) and originates the transverse pancreatic artery in the left aspect (arteria transversa pancreatis), which crosses all along the pancreatic body and tail (Figs. 18.87, 18.88). The dorsal pancreatic artery may give rise to omental branches and also an actual or accessory middle colic artery (Fig. 18.92).
Arteria Pancreatica Magna
The body of the pancreas is supplied by the arteria pancreatica magna (arteria corporis pancreatica or great pancreatic artery) (Fig. 18.93). The arteria pancreatica magna may be single, but it is usually a group of comb-shaped branches, perpendicular to the splenic artery. It anastomoses with the transverse pancreatic artery.
Arteria Caudae Pancreatis (Caudal Pancreatic Artery)
The tail of the pancreas is supplied by multiple branches originated from the splenic artery, right gastroepiploic artery or splenic branches (Fig. 18.94). These branches anastomose with the transverse pancreatic artery and branches of the arteria pancreatica magna.
Short Gastric Arteries
The short gastric arteries (rami gastrici breves) arise from the splenic artery, divisional branches, polar arteries for the spleen and splenic parenchyma (Figs. 18.23, 18.31). They supply the cranial part of the gastric greater curvature (Fig. 18.17). It varies in number from one to four. Up to nine arteries may be found. Anastomosis occurs with other gastric branches.
Posterior Gastric Artery
The posterior gastric artery arises from the splenic artery and supplies the posterior fundic portion of the stomach, passing through the gastrosplenic ligament. It may provide splenic branches for the upper pole of the spleen.
Left Gastroepiploic Artery
This artery is also called the left gastro-omental artery. It is most commonly a branch of the splenic artery and arises as a trunk together with the left gastroepiploic artery and the inferior splenic branch. It may, however, arise from the splenic artery isolated. It reaches the greater gastric curvature in the middle and eventually anastomoses with the right gastroepiploic artery (Fig. 18.95). The left omental (epiploic) artery is a major branch of the left gastroepiploic artery and forms the omental arcade in a significant number of cases. Other branches are the omental (or epiploic) arteries and the posterior and anterior short gastric arteries along the gastric body and antrum (Figs. 18.23, 18.31, 18.86).
Terminal Splenic Branches
The splenic branches enter the hilum after division of the main splenic artery in five or more branches (Figs. 18.96, 18.97). The splenic arterial circulation consists of multiple separate segments, with adjacent compartments without arterial interconnections. Within the spleen, the finest arteriolar branches pass out of the trabeculae, their adventitia being replaced by a periarteriolar sheath. These sheaths constitute the white pulp with splenic lymphatic follicles. The arterioles divide into a series of straight vessels termed penicillary arterioles. These pass through the marginal zones of the white pulp, developing the ellipsoids by thickening of the sheath by aggregation of macrophages and fibroblasts. Beyond the ellipsoids, each vessel continues as a fine arteriole or divides in two. Eventually the blood passes into the red pulp and the venous sinusoids, venules, and small veins. The small veins form the larger veins and exit through the hilum.
Segmental Splenic Branches
In more than 80% of cases, there are only two segments, the superior and the inferior. The superior segment is larger and heavier than the inferior segment in more than 65% of cases. In fewer cases, there are three and four splenic segments (superior, intermediate, and inferior).
Variations of the Celiac Trunk
In 55% to 65% of cases, the celiac trunk divides into three branches: the left gastric artery, the splenic artery, and common hepatic artery. In more than 55% of cases, the inferior phrenic arteries also arise from the celiac trunk either as a single trunk or separately. The rest of the population presents one or more replaced arteries in origin. The celiac trunk may be absent, and the three arteries arise independently from the aorta (Fig. 18.98).
Couinaud described the following eight different types of variations of the celiac trunk.
Type 1. Classic Celiac Trunk: Hepato-Gastro-Splenic Trunk
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree