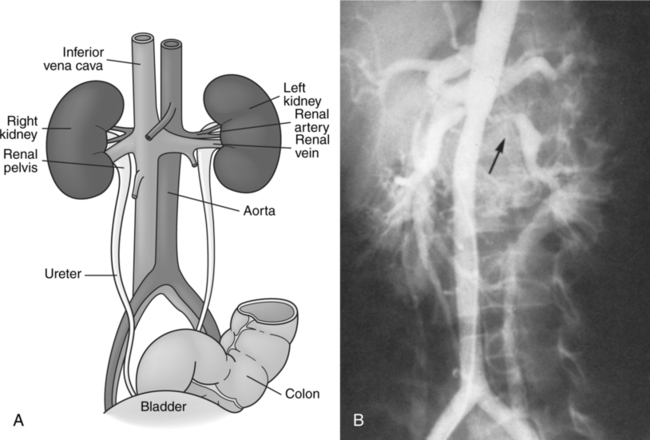
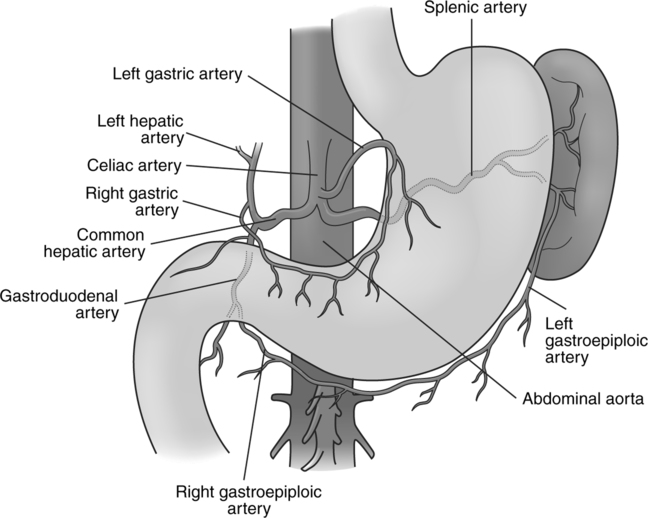
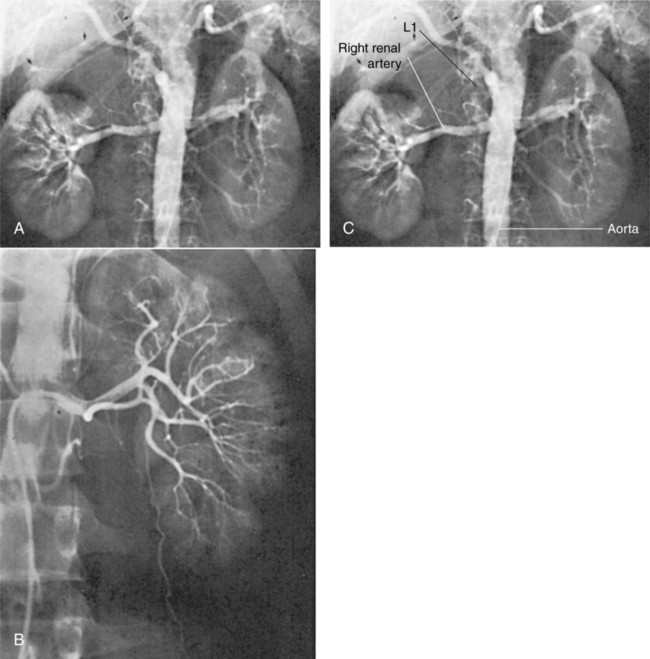
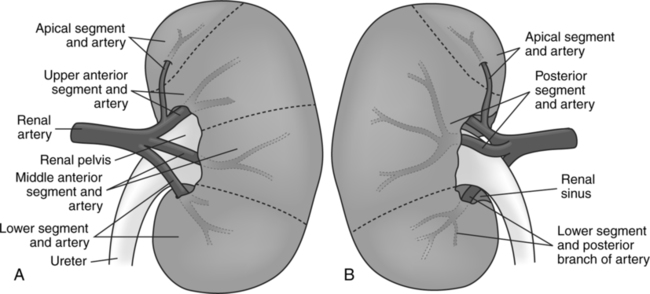
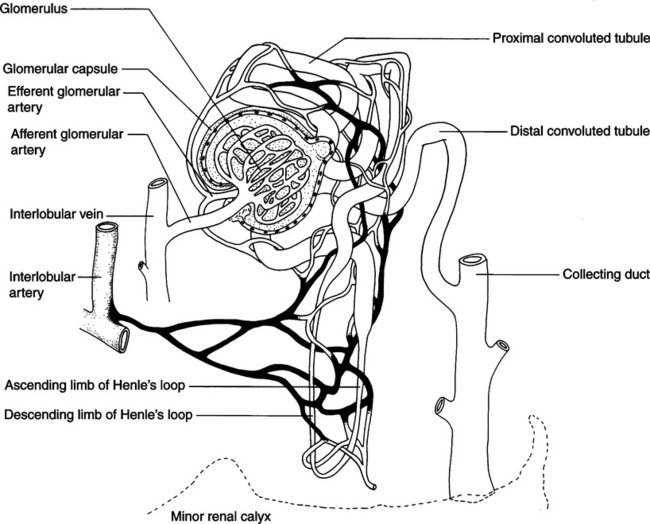
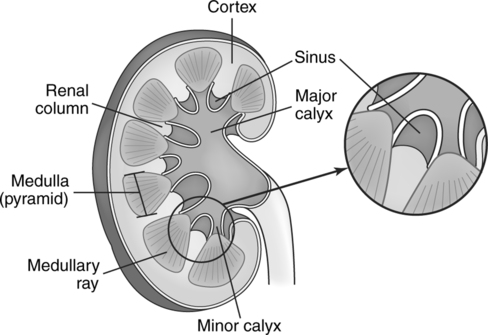
CHAPTER 13 After completing this chapter, the reader will be able to perform the following: The abdominal aorta courses toward the midline anterior to the vertebral column. At the level of the fourth lumbar vertebra, the abdominal aorta bifurcates (splits) into the right and left common iliac arteries ((Fig. 13-1), A and B). The bifurcation can be topographically located slightly inferior and to the left of the navel. This point is considered the termination of the aorta. The common iliac arteries are the major arteries of the pelvis. Each common iliac artery divides into an internal and an external iliac artery. The external iliac arteries then form the femoral arteries of the lower extremities. The first main branch originating on the ventral aorta is the celiac trunk. The main areas supplied by this vessel are the esophagus, stomach, liver, spleen, and pancreas (Fig. 13-2). The celiac trunk bifurcates and gives off the left gastric, splenic, and the common hepatic arteries. The left gastric artery, as its name implies, runs off to the left to supply the stomach coursing along the lesser curvature and connects with the right gastric artery. The splenic artery also runs off to the left and gives off numerous branches to supply the pancreas. The internal structure of the kidney is divided into two areas—the cortex, or outer area, and the medulla, or inner portion. The cortex contains the glomeruli, which are capsules that enclose a convoluted group of capillaries. The glomeruli are portions of the nephrons, the functional units of the kidney (Fig. 13-3). The cortex also comprises other portions of the nephron, the convoluted tubules, and portions of the origins of the collecting ducts. The medulla comprises straight tubules, continuations of the convoluted tubules called Henle’s loop, and collecting ducts. The medulla has the appearance of many pyramids, the apex of which terminates in the cuplike indentation of the minor renal calyx (Fig. 13-4). The renal arteries originate as branches of the abdominal aorta at about the level of the interspace of the first and second lumbar vertebrae (Fig. 13-5). They run transversely toward each kidney, with the right renal artery passing posterior to the inferior vena cava. The superior mesenteric artery is just above the origin of the renal arteries. Before the renal arteries enter the hilum of the kidney, each divides into five branches corresponding to the five renal segments. These enter the renal sinus and course both anteriorly and posteriorly to the renal pelvis (Fig. 13-6). The renal sinus is a recess containing the renal vessels and the renal pelvis, the upper expanded portion of the ureter. Table 13-1 summarizes, in order of filling, the vessels seen during the various phases of renal arteriography. It should be noted that when renal masses are evaluated with intravenous digital subtraction angiography (DSA), the catheter is placed in the inferior vena cava via the femoral approach. This technique demonstrates the patency of the inferior vena cava during the initial phase of the study. The later phases appear as stated in Table 13-1 TABLE 13-1 Summary of Renal Circulatory Pattern
Abdominal Aortography and Genitourinary System Procedures
 Identify the anatomy of the abdominal aorta
Identify the anatomy of the abdominal aorta
 Identify the vascular anatomy of the urinary system and celiac and mesenteric circulation
Identify the vascular anatomy of the urinary system and celiac and mesenteric circulation
 Describe the vascular anatomy of the reproductive system
Describe the vascular anatomy of the reproductive system
 List the various procedures that can be performed in these areas
List the various procedures that can be performed in these areas
 List the indications and contraindications for angiography in these areas
List the indications and contraindications for angiography in these areas
 Identify vessel access for these procedures
Identify vessel access for these procedures
 Describe the contrast agents used in angiography of the genitourinary system
Describe the contrast agents used in angiography of the genitourinary system
Anatomic Considerations
Abdominal Aorta
Celiac Trunk and Mesenteric Circulation
Urinary System
Renal Circulation
Phase
Vessels Observed
Arterial
Abdominal aorta (nonselective studies only)
Renal artery with extrarenal branches
Segmental branches
Interlobular arteries
Nephrogram
Arcuate arteries
Interlobular arteries
Afferent arterioles
Efferent arterioles
Venules
Interlobular and medullary veins
Arcuate veins
Interlobular veins
Venous
Main renal veins
Abdominal Aortography and Genitourinary System Procedures