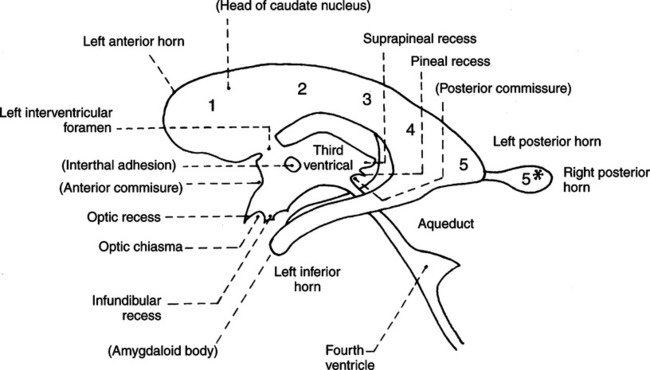
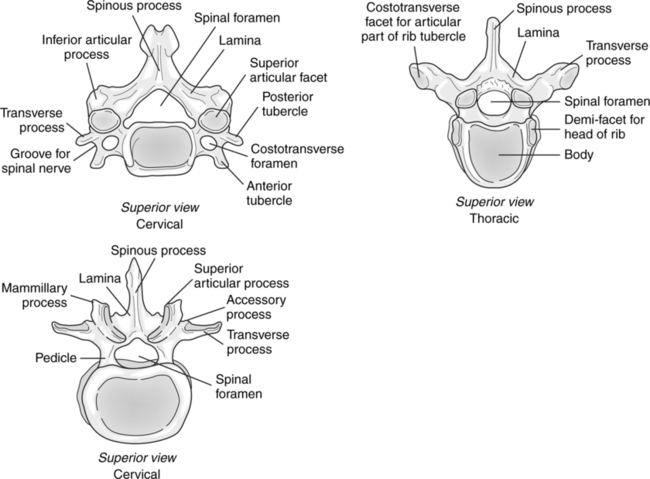
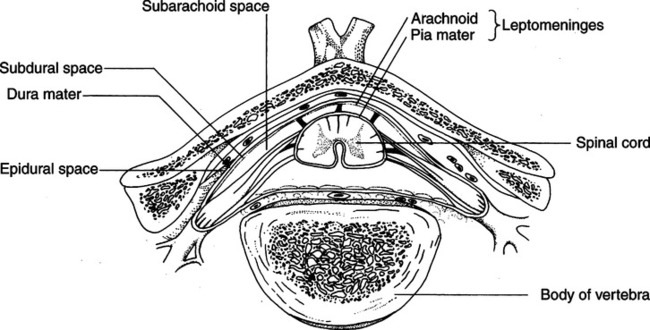
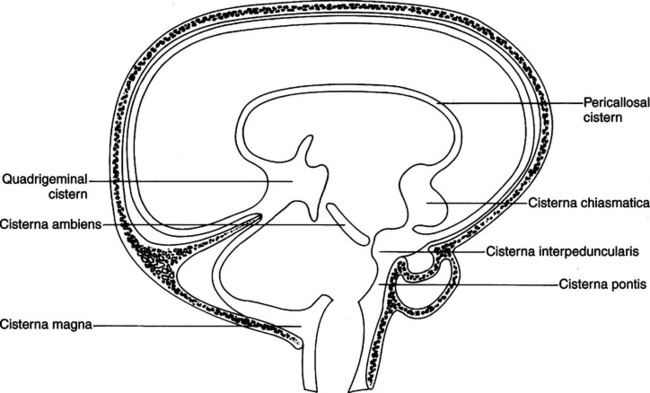
CHAPTER 21 After completing this chapter, the reader will be able to perform the following: In some areas of the brain, the subarachnoid space enlarges to form the subarachnoid cisternae (Fig. 21-1). The cisterna magna extends down to merge with the spinal subarachnoid space. It is triangular and contains approximately 5 to 10 ml of cerebrospinal fluid. The apex of the cisterna magna points toward the vallecula. This is the portion of the subarachnoid space that lies between the fourth ventricle and cisterna magna. When air is injected into the spinal subarachnoid space it must pass through the cisterna magna and vallecula before entering the ventricular system. The flexion of the head must be accurately maintained to prevent air from entering other subarachnoid spaces rather than the ventricular system. There are two lateral ventricles, each located within one cerebral hemisphere. Each lateral ventricle has five divisions (Fig. 21-2): (1) the anterior (frontal) horn; (2) the body; (3) the trigone (isthmus or atrium); (4) the posterior (occipital) horn; and (5) the inferior (temporal) horn. Each lateral ventricle connects on each side with the third ventricle by a narrow channel known as the interventricular foramen of Monro. The anterior (frontal) horns are usually found in the frontal lobes of the brain hemispheres. The vertebral canal tends to be triangular, relatively large in the cervical and lumbar regions, and small and ovoid in the thoracic region (Fig. 21-3). The structures contained in the vertebral canal are the spinal cord and its meninges, spinal nerves and vessels, and the epidural space, which is located between the wall of the vertebral canal and the dura mater. The epidural space contains fat, venous plexuses, and nerves that supply the meninges, intervertebral disks, and ligaments. The three layers—the dura mater, or outer covering; the arachnoid, middle layer; and the pia mater, the inner layer—also enclose the spinal cord and are continuous with the layers surrounding the brain (Fig. 21-4). • Encroachment of intervertebral disks • A tumor or infection, space-occupying lesions • Abnormalities of the blood supply to the spinal cord • Degenerative diseases of the central nervous system • Inflammation of the membrane that covers the brain and spinal cord (arachnoid) • Malformation of the spinal cord Myelography is contraindicated when the patient exhibits signs of increased intracranial pressure.
Myelography
 Identify the anatomy of the brain, ventricular system, and spinal cord
Identify the anatomy of the brain, ventricular system, and spinal cord
 List the indications and contraindications for the procedure
List the indications and contraindications for the procedure
 Describe the patient preparation for the procedure
Describe the patient preparation for the procedure
 Identify the type of contrast media used for the procedure
Identify the type of contrast media used for the procedure
 Describe the two major puncture methods for myelography
Describe the two major puncture methods for myelography
 Describe the needle placements for lumbar, thoracic, and cervical myelography
Describe the needle placements for lumbar, thoracic, and cervical myelography
 Describe computed tomography myelography
Describe computed tomography myelography
 Explain magnetic resonance myelography
Explain magnetic resonance myelography
 List the specialized equipment necessary for the procedure
List the specialized equipment necessary for the procedure
 Describe the patient positioning for the procedure
Describe the patient positioning for the procedure
 Describe the other modalities used to evaluate the central nervous system
Describe the other modalities used to evaluate the central nervous system
ANATOMIC CONSIDERATIONS
Brain
Subarachnoid Cisternae
Lateral Ventricles.
Spinal Cord
INDICATIONS AND CONTRAINDICATIONS
Radiology Key
Fastest Radiology Insight Engine