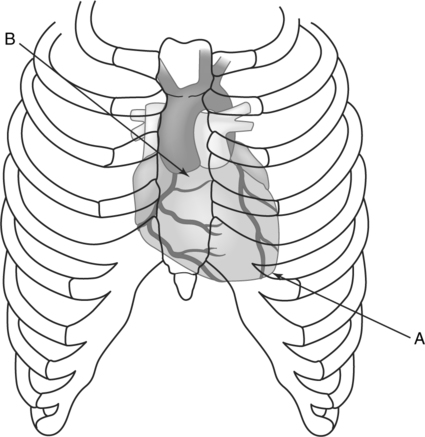
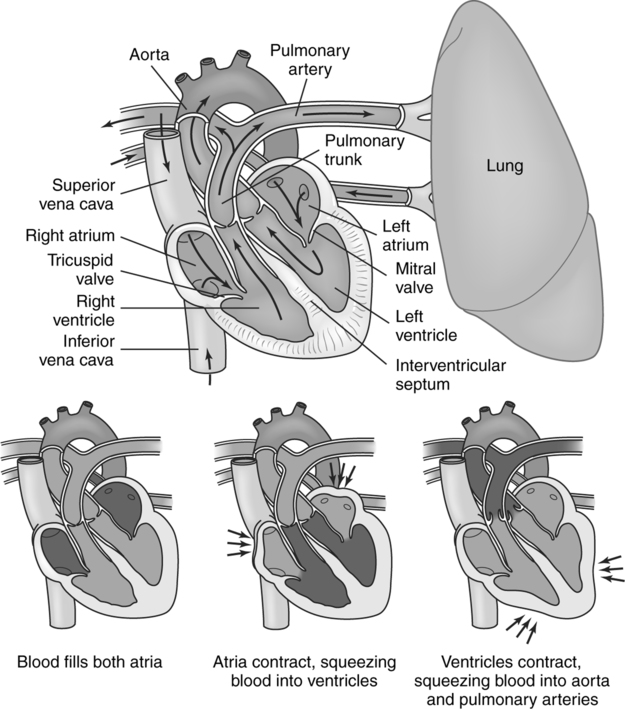
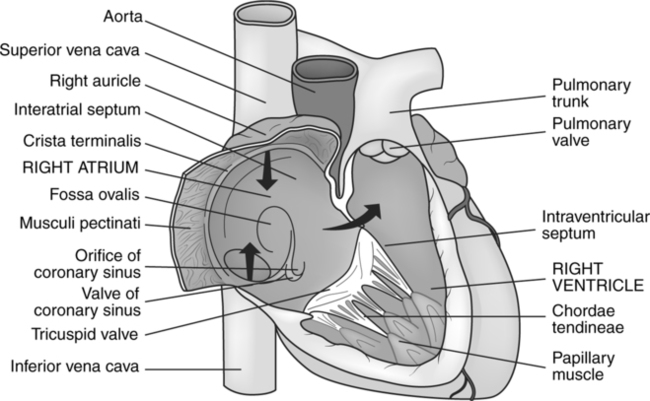
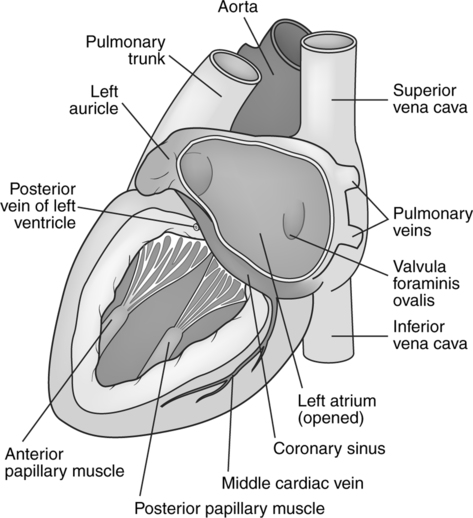
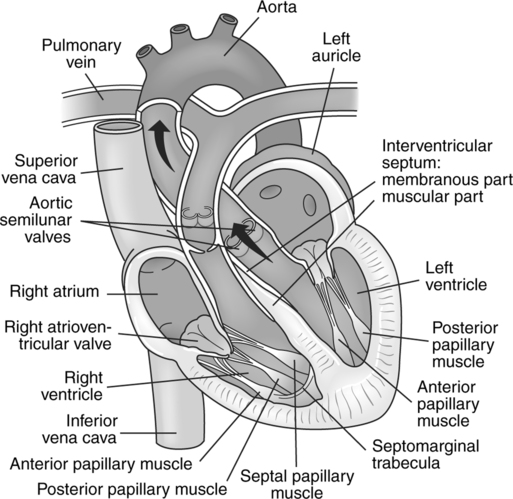
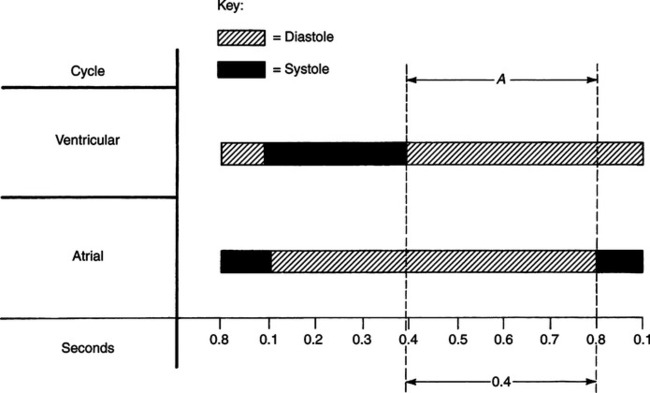
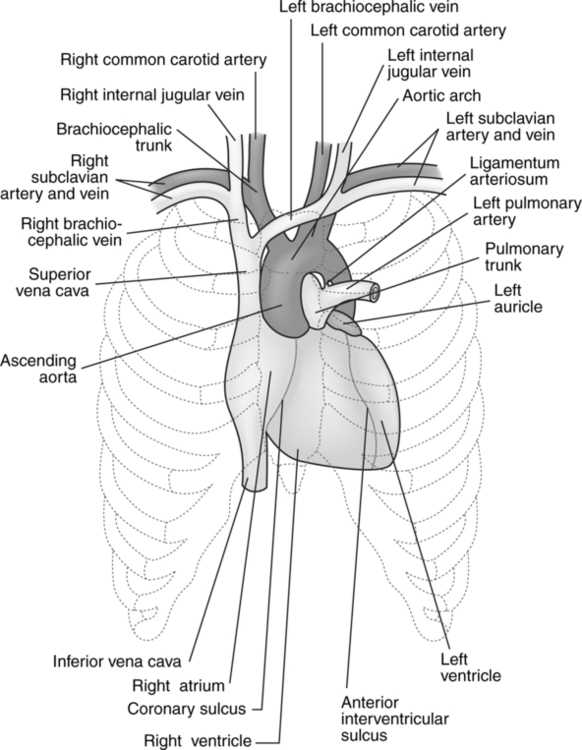
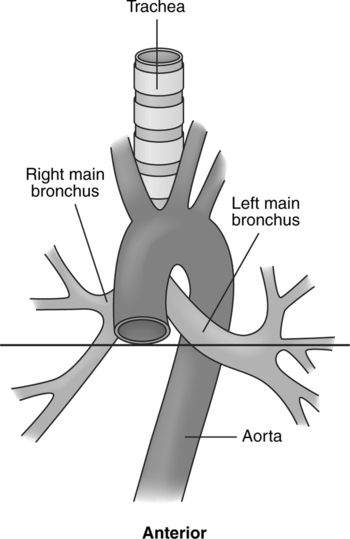
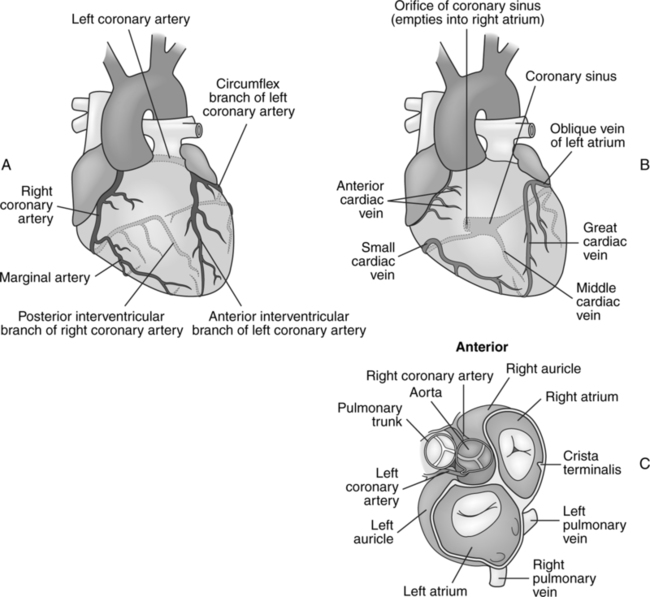
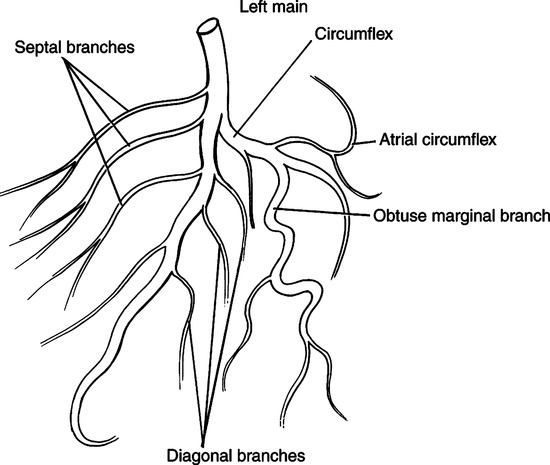
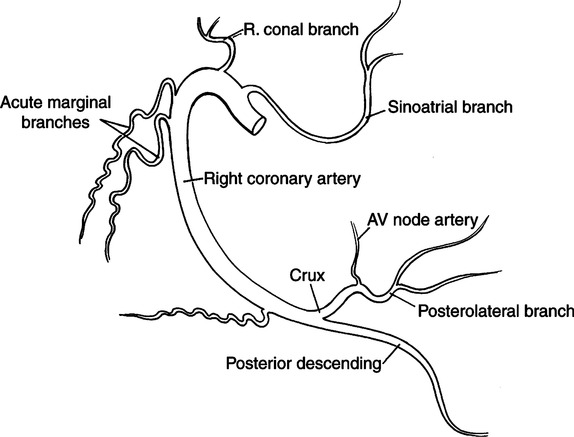
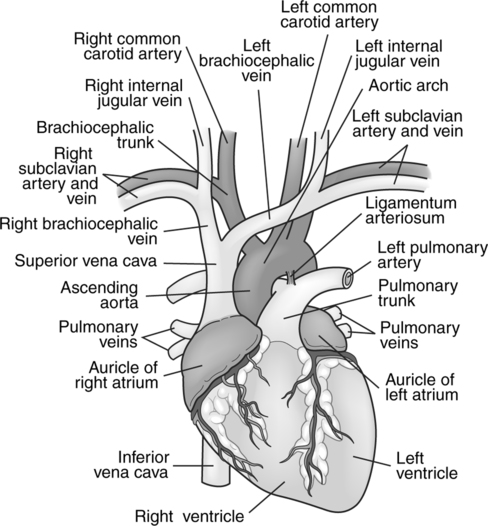
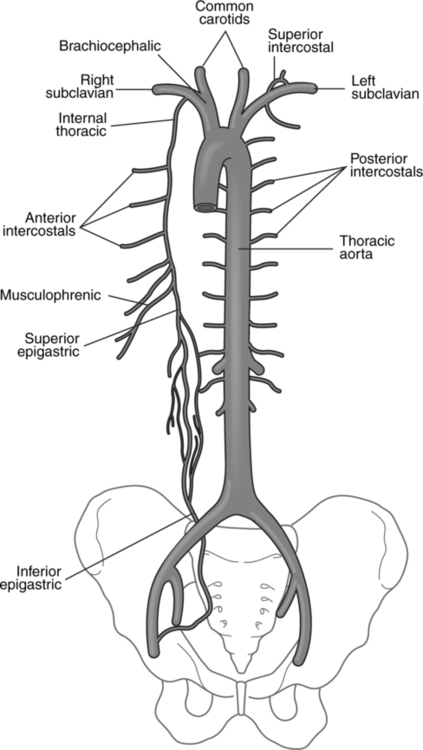
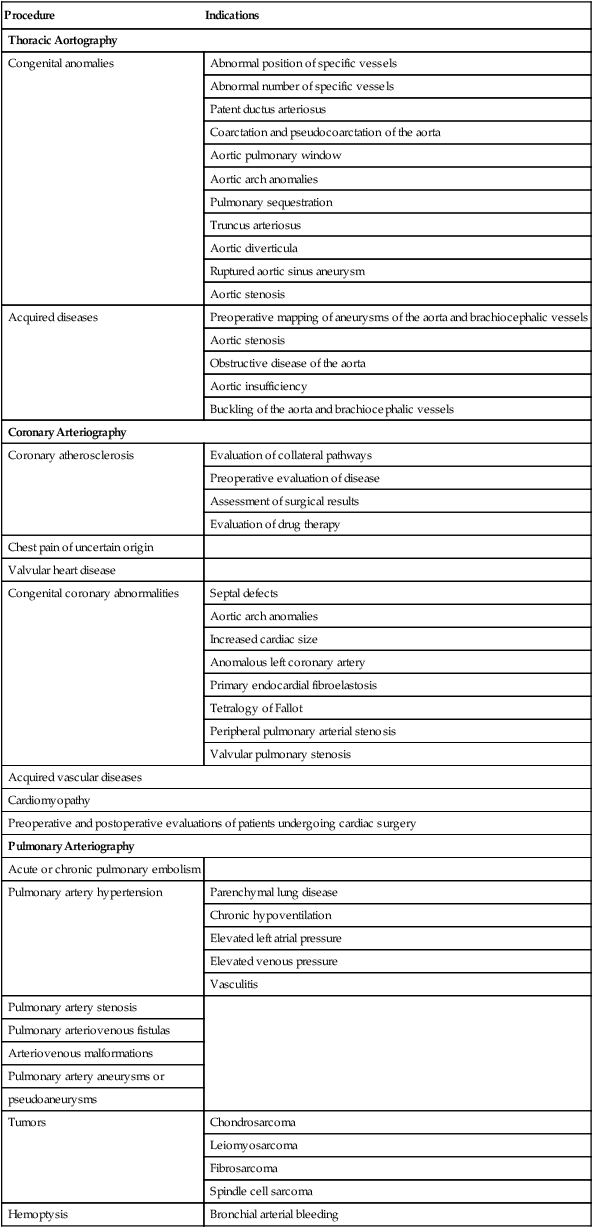
CHAPTER 12 After completing this chapter, the reader will be able to perform the following: Numerous diagnostic studies can be performed on the vasculature of the heart, lungs, and thoracic aorta. In most cases these diagnostic procedures are done with the intent of performing interventions, if possible, in order to correct any pathophysiology that might be identified. The common cardiac and vascular interventions that can be performed will be discussed in Chapters 17 and 18. The interventional studies usually involve the same parameters as the diagnostic procedures, and the basic principles from the diagnostic chapters will not be repeated in the discussion about interventions. The thoracic cavity contains the heart, great vessels, aorta, and pulmonary circulation. Some of the procedures that are performed in this area are aortography, cardiac catheterization, coronary arteriography, and pulmonary arteriography. Discussion of the studies performed on the abdominal aorta and its associated vessels can be found in Chapters 13 and 14. The heart has an apex and a base. The apex is located approximately 8 cm from the median plane at about the level of the fifth or sixth interspace; this level is approximately 2.5 cm inferior to the left nipple. The base of the heart is the most superior portion. It faces up and to the right, and from it emerge the greater vessels (Fig. 12-1). An obliquely placed septum divides the heart into right and left halves. Each half consists of two chambers—an atrium and a ventricle (Fig. 12-2). Blood returning from the systemic veins drains into the venae cavae. These great veins—the superior and inferior venae cavae—empty into the right atrium of the heart (Fig. 12-3). A small amount of venous blood drains from the myocardium directly into the right atrium; however, in general, the greatest portion of venous blood from the systemic circulation drains into the superior and inferior venae cavae. With the contraction (systole) of the right atrium, the blood is forced into the right ventricle through the right atrioventricular aperture. This aperture is equipped with a valve, the tricuspid valve, that prevents the backflow of blood to the right atrium during systole of the ventricle. As the ventricle contracts, the blood is forced past the pulmonary semilunar valve into the pulmonary trunk and the lesser circulation. The arterial, or outflowing, portion of the right ventricle is called the conus arteriosus.1 The pulmonary artery divides into right and left sides, which take the blood through the lungs. Here, the blood gives off carbon dioxide and becomes oxygenated. It is then transported by the four pulmonary veins to the left atrium (Fig. 12-4). As the left atrium contracts, it forces the blood through the left atrioventricular valve into the left ventricle. This is the largest chamber of the heart, and its walls are considerably thicker than those of any other chambers. The thicker walls and larger capacity are necessary to offset the arterial pressure in the aorta. The upper anterior portion of the left ventricle is called the aortic vestibule.1 As the left ventricle contracts, the blood is pushed through the aortic semilunar valve into the aorta and through the systemic circulation (Fig. 12-5). The blood returns from the body tissues through the systemic veins, which ultimately drain into the superior and inferior venae cavae; then the cycle begins again. The cardiac cycle is repeated about 75 times per minute, and the time required for each cycle is about 0.8 s. The cycle consists of three phases—atrial contraction(systole), ventricular contraction (systole), and complete rest (diastole) (Fig. 12-6). The ascending aorta originates at the base of the heart with the root of the aorta. The aortic sinuses are found in the wall of the root of the aorta. These are related to the cusps of the aortic valve and are named for them—right, left, and posterior. Two of these sinuses—the right and the left—contain the orifices of the coronary arteries. The ascending aorta extends anterosuperior from the base of the heart and slightly to the right for approximately 5 cm and terminates by becoming the arch of the aorta, which is usually at the level of the sternal angle (Fig. 12-7). The aortic arch courses from right to left as well as from anterior to posterior. It lies in almost a true sagittal plane (Fig. 12-8). From the sternal angle, the aortic arch ascends toward the left. As it ascends, it is directed posterior. The upper portion of the arch courses posterior to the left of the trachea and esophagus. At about the level of the fourth thoracic vertebra, it turns inferior and runs a short distance before becoming the descending aorta. There are three major branches given off by the aortic arch—the brachiocephalic trunk, the left common carotid artery, and the left subclavian artery (Fig. 12-9). These branches supply the head and upper extremities with blood. The descending aorta is a continuation of the aortic arch. It can be divided into a superior thoracic descending and an inferior abdominal descending portion. The thoracic descending aorta extends from its origin at the level of the intervertebral disk between the fourth and fifth thoracic vertebrae to the point at which it traverses the aortic hiatus in the diaphragm (Fig. 12-10), which is about the level of the twelfth thoracic vertebra. As the thoracic aorta passes through the opening in the diaphragm, it becomes the abdominal portion of the descending aorta. The coronary arteries are the source of blood supplying the heart. The aorta is the origin of the two main coronary arteries (Fig. 12-11). Three small dilations, or sinuses, are located in the root of the aorta. They lie opposite the corresponding cusps of the aortic valve. The coronary arteries arise from two of these, so they are considered coronary sinuses. The third sinus is considered a noncoronary sinus because it does not connect directly with any coronary arteries. This artery originates in the left aortic sinus. It arises from a single opening in the upper portion of the sinus, and its length can vary from 2 to 3 mm to 3 to 4 cm. It divides to form the anterior interventricular branch (left anterior descending artery) and the left circumflex branch (Fig. 12-12). These branches occupy the anterior interventricular sulcus and the atrioventricular sulcus, respectively. This oversimplification of the bifurcation of the left main coronary artery is provided because usually no more than two large branches of this artery can be found.1 Frequently, the right main coronary artery has two aortic ostia, which may arise from the anterior aortic sinus and from a smaller adjacent ostium. When present, the second ostium is very small—about 1 mm in diameter. This is called the conus artery of the right coronary system (Fig. 12-13). It is this artery that frequently anastomoses with an opposing branch from the left anterior interventricular artery, forming Vieussens’ ring. When the right main coronary artery arises from a single ostium in the aortic sinus, the first ventricular branch is considered the conus artery. Some specific indications for the procedure include suspected aneurysms, congenital anomalies, and many acquired diseases affecting the thoracic aorta. Table 12-1 lists specific indications for angiography of the thoracic aorta, cardiac circulation, and pulmonary circulation. TABLE 12-1 Summary of Indications for Angiography of the Structures in the Thoracic Cavity
Cardiac and Thoracic Procedures
 Discuss the anatomy of the heart and its vasculature
Discuss the anatomy of the heart and its vasculature
 Discuss the anatomy of the thoracic aorta
Discuss the anatomy of the thoracic aorta
 Discuss the anatomy of the pulmonary circulation
Discuss the anatomy of the pulmonary circulation
 List the indications and contraindications for angiography in these areas
List the indications and contraindications for angiography in these areas
 List the various procedures that can be performed in these areas
List the various procedures that can be performed in these areas
 Discuss vessel access for these procedures
Discuss vessel access for these procedures
 Discuss hemodynamics and the various calculations performed during cardiac catheterization
Discuss hemodynamics and the various calculations performed during cardiac catheterization
 Discuss the contrast agents used in cardiac catheterization
Discuss the contrast agents used in cardiac catheterization
 List the specialized equipment found in the cardiac catheterization suite
List the specialized equipment found in the cardiac catheterization suite
 List the patient positions for cardiac angiography
List the patient positions for cardiac angiography
ANATOMIC CONSIDERATIONS
Heart
Thoracic Aorta
Coronary Vasculature
Left Main Coronary Artery
Right Main Coronary Artery
INDICATIONS AND CONTRAINDICATIONS
Procedure
Indications
Thoracic Aortography
Congenital anomalies
Abnormal position of specific vessels
Abnormal number of specific vessels
Patent ductus arteriosus
Coarctation and pseudocoarctation of the aorta
Aortic pulmonary window
Aortic arch anomalies
Pulmonary sequestration
Truncus arteriosus
Aortic diverticula
Ruptured aortic sinus aneurysm
Aortic stenosis
Acquired diseases
Preoperative mapping of aneurysms of the aorta and brachiocephalic vessels
Aortic stenosis
Obstructive disease of the aorta
Aortic insufficiency
Buckling of the aorta and brachiocephalic vessels
Coronary Arteriography
Coronary atherosclerosis
Evaluation of collateral pathways
Preoperative evaluation of disease
Assessment of surgical results
Evaluation of drug therapy
Chest pain of uncertain origin
Valvular heart disease
Congenital coronary abnormalities
Septal defects
Aortic arch anomalies
Increased cardiac size
Anomalous left coronary artery
Primary endocardial fibroelastosis
Tetralogy of Fallot
Peripheral pulmonary arterial stenosis
Valvular pulmonary stenosis
Acquired vascular diseases
Cardiomyopathy
Preoperative and postoperative evaluations of patients undergoing cardiac surgery
Pulmonary Arteriography
Acute or chronic pulmonary embolism
Pulmonary artery hypertension
Parenchymal lung disease
Chronic hypoventilation
Elevated left atrial pressure
Elevated venous pressure
Vasculitis
Pulmonary artery stenosis
Pulmonary arteriovenous fistulas
Arteriovenous malformations
Pulmonary artery aneurysms or
pseudoaneurysms
Tumors
Chondrosarcoma
Leiomyosarcoma
Fibrosarcoma
Spindle cell sarcoma
Hemoptysis
Bronchial arterial bleeding
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine