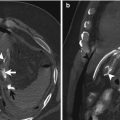
Fig. 17.1
A 51-year-old woman presenting with dyspnea after a liver transplant. Axial CT image shows free intraperitoneal liquid (black arrow), the collapsed inferior vena cava (arrowhead), and the “round belly sign” (blue arrow). The intravesical pressure was 21 mmHg. The occurrence of abdominal compartment syndrome is about 30 % after liver transplantation

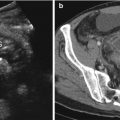
Fig. 17.2
A 19-year-old man with acute abdominal pain. Axial contrast-enhanced CT image shows massive dilatation of colic loops over spread by fecal material (toxic megacolon). The “round belly sign” and bilateral renal displacement and compression are evident. The patient underwent colectomy
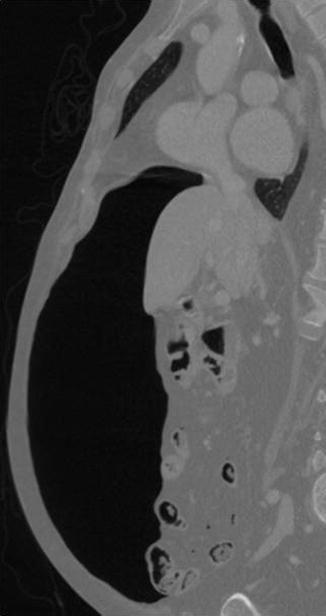
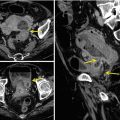
Fig. 17.3
An 84-year-old woman with colonic perforation. Multidetector-row computed tomography (sagittal reconstruction) with intravenous contrast medium showing pneumoperitoneum with compression of the intra-abdominal viscera
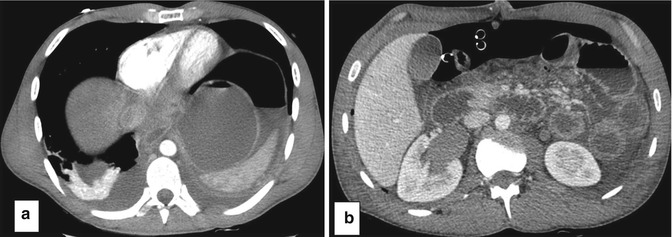
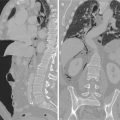
Fig. 17.4
A 19-year-old man (the same patient of Fig. 17.2) with sudden hypotension, tachycardia, and respiratory failure after colectomy due to toxic megacolon. Axial contrast-enhanced CT images show (a) an elevated left diaphragm and free intraperitoneal air and liquid and (b) bowel wall thickening. The intravesical pressure was 20 mmHg. The patient underwent emergency abdominal laparotomy but died due to severe heart failure
Epelman et al. [29] evaluated the preoperative abdominal CT scans of three children with proven ACS to identify signs of elevated IAP. Findings common to these patients included narrowing of the inferior vena cava, direct renal compression or displacement, bowel wall thickening with enhancement, and a rounded appearance of the abdomen. Other investigators described elevation of the diaphragm (Fig. 17.4) in association with IAH [30]. Al-Bahrani et al. [31] evaluated the abdominal CT examination performed in 24 critically ill patients and affirmed that the presence of the round belly sign and the bowel wall thickening with enhancement on CT images of critically ill surgical patients should alert clinicians to the possibility of the presence of IAH and ACS.
It is important to recognize that the CT examination should be viewed as an adjunct toward the recognition of IAH, but not as a substitute to the measurement of the intravesical pressure in at-risk patients. Individual CT signs such as elevated hemidiaphragm, flattened inferior vena cava and renal veins, and increased bowel wall enhancement are neither sensitive nor likely specific for abdominal compartment syndrome. However, when a combination of these findings is present in the appropriate clinical setting or if the signs are seen to worsen on sequential imaging studies, the radiologist should raise the possibility of abdominal compartment syndrome [27, 32]. Identifying patients with IAH and/or ACS at earlier stages could potentially improve the outcome of these patients by early radiological drainage of large fluid collections and/or surgical intervention with abdominal decompression (laparotomy).
17.6 Conclusions
ACS has tremendous relevance in the practice of surgery and the care of critically ill patients because of the effects of elevated pressure within the confined space of the abdomen on multiple organ systems. ACS has been identified to be a cause of significant morbidity and mortality among critically ill surgical, medical, and pediatric patients. With an incidence of IAH that approximates 30–80 % and from 4 to 30 % for ACS depending on the population, this disease entity can no longer be ignored in the critically ill/injured.
The most important factor in the diagnosis of abdominal compartment syndrome is proper suspicion in the appropriate clinical setting. Multidetector row Computed Tomography can provide evidence of an increased intra-abdominal pressure in patients at risk for developing abdominal compartment syndrome.
References
1.
Kron IL, Harman PK, Nolan SP (1984) The measurement of intra-abdominal pressure as a criterion for abdominal re-exploration. Ann Surg 199:28–30PubMedCrossRefPubMedCentral
2.
3.
4.