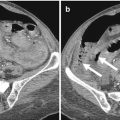
Fig 5.1
Axial MPR CT image. Perforation of the anterior wall of the gastric antrum. Focal defect in the anterior wall of the gastric antrum associated with surrounding mural thickening (white arrow). Pneumoperitoneum (black arrow). Extraluminal fluid with small free air bubble inside (white arrowhead). Intraperitoneal fluid in subhepatic space (black arrowhead)
Other reported causes are traumatic, neoplastic, foreign body ingestion, and iatrogenic.
With regard to iatrogenic causes, blunt trauma usually induces perforation of the descending and horizontal segments of duodenum because of their firm attachment and the compression against the vertebral column.
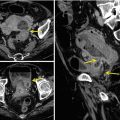
Neoplastic causes usually depend on the presence of a tumor that can lead to obstruction or increased endoluminal pressure (Fig. 5.7).
Perforation can also arise from foreign bodies that can be ingested either intentionally or accidentally; this injury can cause perforation either through direct damage or endoluminal obstruction.
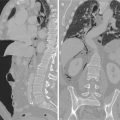
In the era of diagnostic and therapeutic use of esophagoduodenoscopy, iatrogenic lesion represents an increasing cause of gastroduodenal perforation. Other iatrogenic causes are related to the placement of inferior vena cava filter, ERCP, and biliary stents [3] (Fig. 5.5).
5.2 Diagnosis
A correct diagnosis of gastroduodenal perforation strictly relies on signs and symptoms referred by the patient and detected during clinical examination. For example, the presence of intermittent abdominal pain, gastroesophageal reflux, ongoing symptoms and sudden exacerbation of pain in known peptic ulcer disease, and recent trauma or diagnostic/therapeutic intervention followed by worsening pain should alert the clinician for the presence of injury [2].
The location of the pain facilitates definitive diagnosis, because with the time a localized peritoneal inflammation develops exactly at level of the injured organ involving a correspondent abdominal wall segment.
Patients with gastroduodenal perforation usually present with signs and symptoms of either local or generalized peritonitis due to the leakage of luminal contents in the peritoneal cavity.
For instance, a lesion of the gastroduodenal wall provokes intra-abdominal contamination with peritonitis or abscesses [4].
The type and the intensity of peritoneal contamination strictly rely on the site, size, and duration of perforation other than other factors such as time from the last meal, coexistent diseases, presence or absence of an ileus or bowel obstruction, etc.
The anatomic site of perforation heavily influences the type and the severity of enteric contamination [5, 6].
Microbiological contamination increases from proximal to distal side of the gastrointestinal tract; the stomach and duodenum show the lowest number of vital microorganisms per gram of luminal contents due to a hostile local environment from acidic, biliary, and pancreatic secretions, and in fact the bacterial load is inversely related to the toxicity of organ fluid composition [7, 8].
Organ-specific fluid composition affects not only bacterial load but also bacterial species composition with consequent different early presenting symptoms from a perforated hollow viscus that can be helpful for the diagnosis. For example, patients suffering from gastric or duodenal perforation usually present with highly acute pain due to a rapid chemical peritonitis usually followed by a systemic inflammatory response. In the untreated patients or in those who have late presentation, the perforation can also proceed to an infected peritonitis and sepsis [9].
Laboratory tests are usually performed to get a correct diagnosis or to facilitate the differential diagnoses. Routinely ordered tests include a complete blood cell count with differential, coagulation panel, electrolyte panel, liver function tests, urinalysis, lipase or amylase, arterial blood gas, and serum lactate level [10, 11].
Laboratory tests are usually nonspecific, but leukocytosis, metabolic acidosis, and hyperamylasemia may be indicative of the presence of perforation.
Plain abdominal films are the initial diagnostic tool in patients with clinically suspected gastroduodenal perforation. In addition to upright and supine abdominal radiographic images, upright chest films and/or left lateral decubitus abdominal films should be included for the accurate evaluation of perforation [1].
The radiologic feature of perforation is the presence of air and/or fluid in the peritoneal cavity, retroperitoneal spaces, mesentery, or ligaments of organs. In some cases, pneumomediastinum or subcutaneous emphysema can also be detected. About one-third of cases of gastroduodenal perforation do not present with pneumoperitoneum on abdominal radiographs. This situation is usually caused by a very small perforation, perforation well contained by adjacent organs, or empty stomach at the time of perforation [12].
The reported sensitivity in the detection of extraluminal air on plain radiography is 50–70 % [13, 14].
US is considered a useful diagnostic tool because even if it is not actually helpful to identify intraperitoneal free gas, it could identify some suggestive findings of gastrointestinal perforation such as the decreased peristalsis and the presence of intraperitoneal free fluid. It is worth to note that usually in the case of gastroduodenal perforation the evidence of free peritoneal fluid is the only finding of injury, but unfortunately US study is not able to define the exact cause for its presence (peritoneal reaction or perforated intestinal loop) [15, 16].
When a perforation of the gut is not proved by plain radiograph and more accurate assessment regarding the site and cause of perforation is needed, a contrast examination may be indicated. Water-soluble iodinated contrast material is administrated orally, if gastroduodenal tract is the suspected site of perforation. It may demonstrate extraluminal contrast material leakage as a direct sign of bowel perforation. However, the reported sensitiveness of extravasation of oral contrast material on plain radiograph varies from 19 to 42 % [17–19].
CT is now estimated the most valuable imaging technique to identify the presence, site, and etiology of gastrointestinal (GI) tract perforation [17].
CT is indicated in two different cases: when clinical suspicion is high, but there is no pneumoperitoneum on the plain abdominal radiograph; the clinical signs are atypical, or, instead, peritonitis is present with no etiological explanation [20].
Several authors have illustrated the direct and indirect CT findings of bowel perforation, and free extraluminal air has been regarded as a major imaging finding to identify the GI tract perforation [17, 21–24].
CT is more sensitive than plain radiography in determining the presence of perforation because it can also display a small amount of free extraluminal, intraperitoneal, or retroperitoneal air. The overall accuracy of CT for predicting the site of bowel perforation has been reported to range between 82 and 90 %. However, the recent introduction of multidetector row CT has improved the accuracy of CT for predicting the site of GI tract perforation [16, 21, 24–26].
According to the perforation site the CT findings may be different. In this chapter, CT findings of gastroduodenal tract perforation will be reported.
5.3 CT Technique
Whole abdomen, from the dome of the diaphragm to the pelvic floor, should be scanned with a multidetector CT (MDCT). The protocol used with a 64-row MDCT included, after the pre-contrast images have been acquired, a helical axial acquisition at 70 s after the intravenous injection of contrast material (400 mgI/mL; 100–150 mL at a rate of 2–3 mL/s), a 1- to 2.5-mm collimation and reconstruction in 0.625 mm contiguous slices.
The analysis was immediate on a workstation, allowing multiplanar reconstructions that were used systematically. In our hospital, we use CT scanning without oral contrast administration for evaluating bowel perforation. In fact, even if the contrast may improve the detection of the lesions site of the posterior gastrointestinal wall, on the other site, it becomes difficult to identify a perforation in the axial scan, when the lesion lies just near the anterior bowel wall.
Although extraluminal leakage of oral contrast material has been reported to be a specific finding for bowel perforation, several authors queried about the extra benefit of oral contrast [13, 17, 22, 27]. Several reports adduce safety issues (i.e., the risk of aspiration and the subsequent complications), the potential delay in the diagnosis, and the lack of substantial extra benefit for detecting bowel perforation.
Further, the slow progression of the oral contrast material in the GI tract in a patient suffering from paralytic ileum, and the quick sealing of the perforation site, may preclude extraluminal leakage of oral contrast material in patients with GI tract perforation [17].
5.4 CT Findings
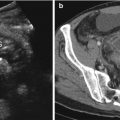
We classified the CT findings of GI tract perforation as direct and indirect findings. The first one included extraluminal air (free air) and direct visualization of GI tract wall rupture. The second one included focal bowel wall thickening (>8 mm in gastroduodenal wall), abnormal bowel wall enhancement, inflammatory changes (abscess and an inflammatory mass adjacent to the bowel), or a fluid collection in the surrounding soft tissues or organs [1, 21, 23, 28, 29]. Direct visualization of the discontinuity of the bowel wall can specify the presence and site of GI tract perforation, which is marked by a low-attenuating cleft that usually runs perpendicular to the bowel wall on CT [17, 24] (Figs. 5.1 and 5.2). However, this cleft has been reported to be observed less frequently than free air on CT, and a cleft is usually seen in less than 50 % of the patients with GI tract perforation [21, 23, 24, 28]. The relatively infrequent detection of this finding is partly due to the small size of the lesion [23]. MDCT with multiplanar reformation images may help identify discontinuity of the bowel wall, and especially when the axial CT images are indeterminate. Although extraluminal air is highly specific for making the diagnosis of GI tract perforation, it may be absent in gastroduodenal perforation, and especially at the onset of symptom [16]. The sensitivity of plain radiograph to detect free extraluminal air is not high [1, 24]; in contrast, CT is highly sensitive for detecting pneumoperitoneum and very small free air bubbles. To enhance this sensitivity, CT images should also be assessed in the wide window setting that distinguishes air from fat densities [11, 14]. The amount and location of free air could be different according to the perforation site. A large amount of intraperitoneal air usually indicates gastroduodenal perforation, except for bowel perforation, which is caused by obstruction or an endoscopic procedure. Air in the lesser sac is commonly due to posterior perforation of the stomach or duodenum. Free air or an air-fluid level crossing the midline and an accentuating falciform ligament (the “falciform ligament sign”) (Fig. 5.6) and free air confined in the intrahepatic fissure for the ligamentum teres (the “ligamentum teres sign”) have been considered to be useful findings in patients with perforation of the duodenal bulb or stomach. Air trapped in the mesenteric folds is seldom seen in gastric perforation. Pneumoretroperitoneum is caused by perforation of descending horizontal duodenal tract. Gas in the retroperitoneum does not spread freely as in the peritoneal space; specifically, when the amounts is small, it tends to remain regional with respect to the boundaries of the retroperitoneal compartment in which it arises. Extraluminal free air in the right anterior pararenal space is the reliable CT finding for diagnosing duodenal perforation beyond the bulbar segment [1, 17, 28, 30] (Fig. 5.5).
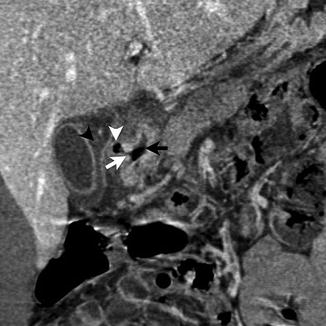
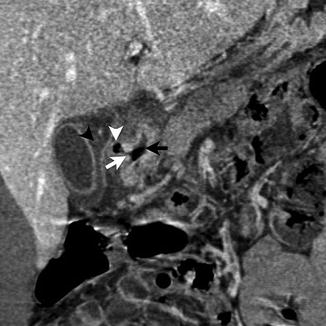
Fig. 5.2
Coronal MIP CT image. Covered perforation of the duodenal bulb. Focal defect in the wall of the duodenal bulb (white arrow). Intraluminal air (black arrow). Small extraluminal free air bubble (white arrowhead). Intraperitoneal fluid (black arrowhead)
It should be noted that extraluminal intra- or retroperitoneal air could occur without GI tract perforation. Various causes can produce air, such as mechanical ventilation and pulmonary barotraumas, peritoneal lavage that is performed prior to CT, pneumothorax, chest injury, and entry of air via the female genital tract. Thus, additional CT findings that are indicative of GI tract perforation intensify the significance of extraluminal free air [17, 23].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree