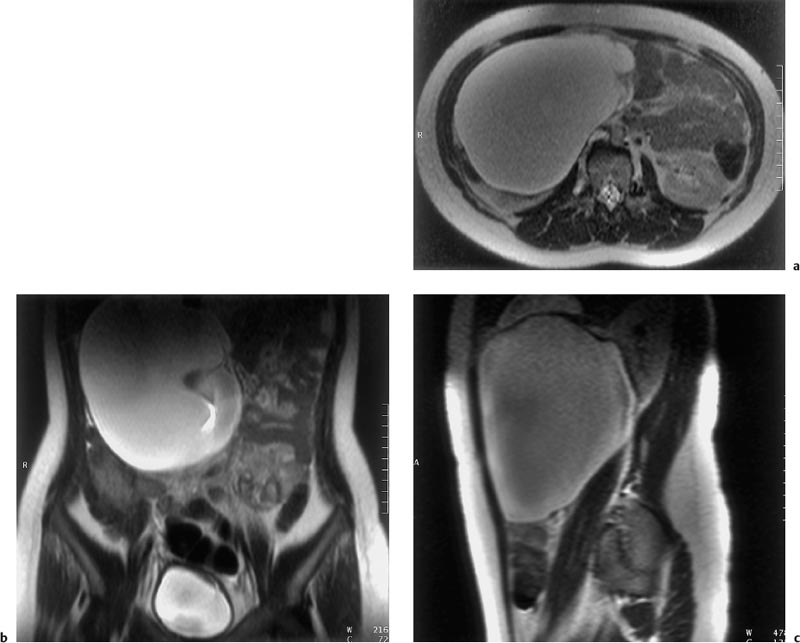
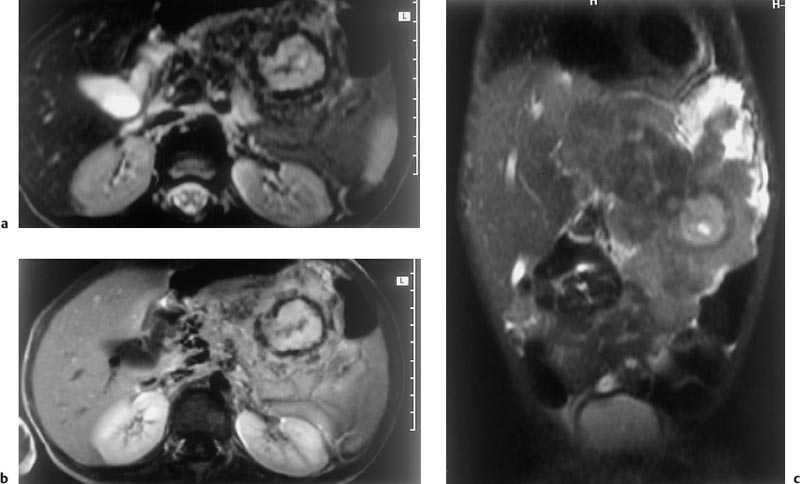
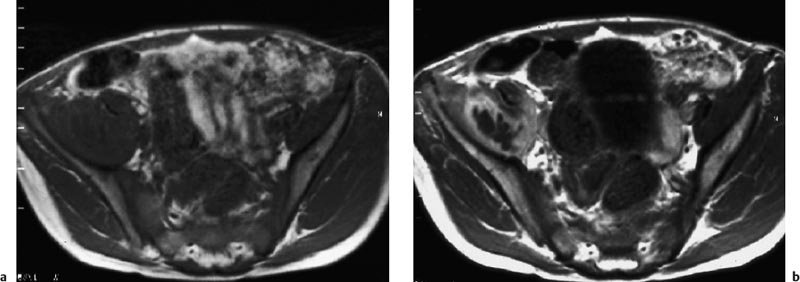
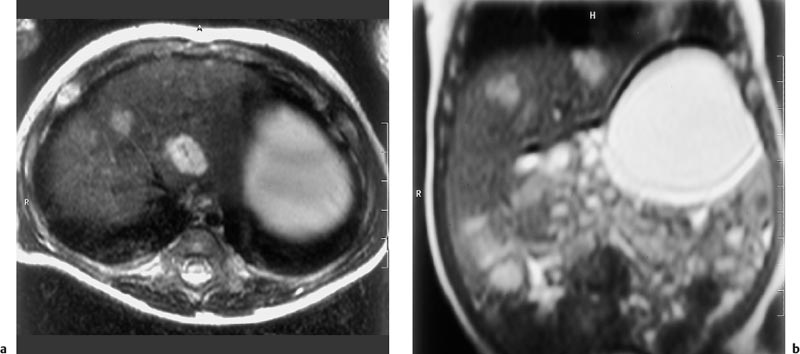
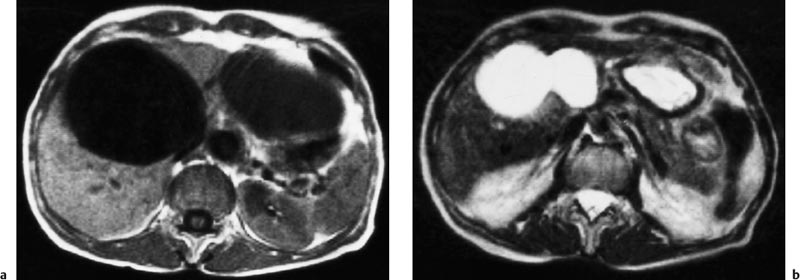
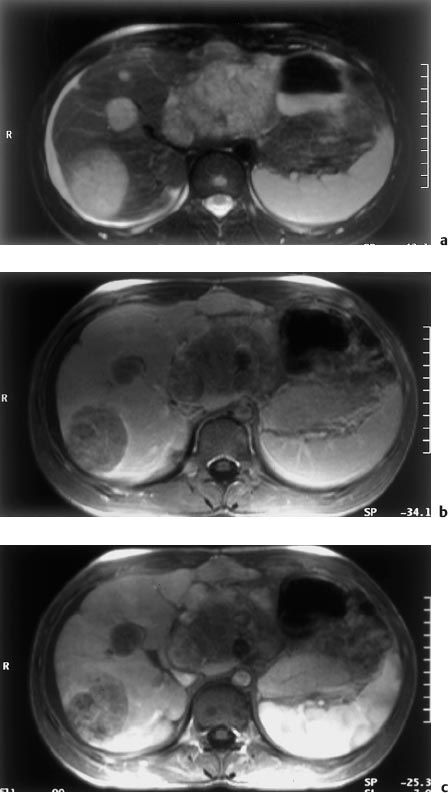
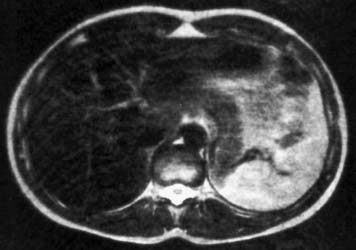
17 Abdominal MRI in Children Minimizing radiation exposure is a primary concern when imaging children. Ultrasonography (US) is the first-line imaging modality for examining the abdomen in pediatric patients. In all cases requiring further diagnostic work-up, MRI should be preferred whenever it is expected to provide the same level of diagnostic information as CT. The indications for pediatric MRI are discussed in relation to the specific disease entities presented in the remainder of this chapter. Children can be examined at 0.2–0.5 T, but, as in adults, image quality is better at higher field strength (1.0–1.5 T). A considerable size discrepancy can exist between the coil and the imaging volume in newborns and infants. Therefore, the smallest coil available to image the target anatomy should be employed to optimize the signal-to-noise ratio (SNR). To compensate for the size discrepancy and to increase image quality, the filling factor of the coil can be improved by placing saline infusion bags inside the coil together with the child, even when imaging neonates with a head or knee coil. Flexible wraparound coils are most suitable to ensure optimal visualization of very small volumes in neonates and infants. Body or torso phasedarray coil systems should only be used in older children. Conventional spin echo (SE) sequences or their rapid counterparts—fast or turbo SE sequences (FSE or TSE)—acquired with T1, T2, or proton density (PD) weighting are the mainstay of abdominal imaging in pediatric patients. The SE sequences can be supplemented by gradient echo (GRE) sequences (e. g., FLASH, FFE). Markedly shorter scan times are achieved by using an inversion-prepared T1w GRE sequence (TurboFLASH) or a very heavily T2-weighted sequence such as single-shot TurboSE or RARE. Heavily T2-weighted sequences accentuate fluid and provide useful information for tissue characterization and narrowing the differential diagnosis within a few seconds. In older children, additional information for tissue characterization can be obtained by acquisition of in-phase (IP) and opposed-phase (OP) images during breath-holds. Fat suppression techniques are especially beneficial in abdominal MRI because they reduce artifacts and improve contrast. Magnetic resonance angiography (MRA) sequences are useful for detecting abdominal vascular malformations and angiomatous tumors, and MRA is increasingly being used to assess the vascular supply of a tumor before surgery or to define vascular anatomy and identify vascular anomalies prior to transplant. More specific information on the most suitable pulse sequences will be provided with the disease entities discussed in this chapter. Careful positioning is especially important in children to compensate for the aforementioned size discrepancy between coils and scan volumes. For most examinations, some fixation inside and outside the coil will be necessary to help prevent spontaneous movement. Anesthesia is rarely needed for an abdominal MRI scan in children. Newborns and infants in the first 3 months of life rarely require sedation. They will be fed immediately before imaging and wrapped up warmly. In contrast, most children aged between 4 months and ca. 4–5 years need to be sedated for the examination. Various sedation regimens, including oral or rectal chloral hydrate and oral diazepam, have shown to be effective. If intravenous sedation is used, reliable venous access must be ensured throughout the examination. To minimize the period of sedation and the risk of adverse effects, including erethic states, intravenous sedation should not be started until after the child has been positioned on the scanner table. Pediatric patients under sedation should be monitored by electrocardiography and pulse oximetry. Depending on the situation, a pediatrician or anesthetist should be present, or at least a nurse. Children will tolerate an MRI examination best if a parent or some other familiar adult stays with them in the scanner room. Although no serious adverse reactions have been observed in children after intravenous administration of contrast medium, strict criteria apply and must be followed in every case. Some of the nonspecific Gd-based MR contrast media (e. g., Dotarem) are approved for all ages. The dose is 0.1 mmol Gd per kg body weight, corresponding to a dose of 0.2 mL/kg for contrast preparations formulated at the usual concentration of 0.5 mmol Gd/mL. Currently, a higher dose of 0.2 mmol Gd/kg is used only for MRA. Manual injection is recommended for babies and young children. Oral contrast media are also beneficial in pediatric patients undergoing abdominal MRI. Gd-based signal-enhancing (positive) agents are no longer on the market. The only commercially available negative oral contrast medium (eliminating signal) is a ferrite preparation (Lumirem) that is not approved for children. Chloral hydrate, which is used for sedation, often also produces good contrast of bowel segments. Whole milk can serve as a positive contrast agent and ensures good delineation of the bowel, especially on T2w images. Perfluorooctyl bromide also acts as a negative oral contrast agent and has been investigated in studies but is not approved as a contrast medium either. Since no serious adverse events are known for oral contrast media in adults, their use in children is justified in individual cases, especially in cancer patients. In children as in adults, a pacemaker is the most important contraindication to MRI. Other implants that may be made of ferromagnetic material include spinal stabilizers or older shunt systems for cerebrospinal fluid drainage.1 Most implants used in interventional procedures are made of nonferromagnetic materials. However, so-called umbrellas used for closure of congenital cardiac defects may be partially ferromagnetic and preclude MRI. In all other cases children with implants can be examined by MRI if the implants are made of materials approved for MRI. Metal splinters may preclude an MRI examination in children who have had an accident. Careful screening for shrapnel is warranted in children from war zones. US is the primary imaging modality for the pathomorphologic evaluation of the gastrointestinal (GI) tract and will diagnose the vast majority of congenital anomalies, infectious diseases, and tumors. MRI can supplement US if it is expected to provide additional information (Fig. 17.1). MRI is performed using SE sequences or GRE sequences with fat suppression. In older children, breath-hold T1w IP and OP images will yield excellent results. Presaturation bands are usually needed to eliminate motion artifacts. For some examinations, an antispasmodic agent may be required to suppress peristalsis. During the first year of life, MRI of the GI tract is limited by the high physiologic respiratory rate and the presence of large amounts of air throughout the bowel. Congenital Anomalies MRI is not the first imaging test in children with a suspected congenital anomaly of the upper GI tract, which is typically diagnosed by prenatal US and confirmed after birth by US and radiography of the chest and abdomen. Intestinal Duplication MRI is rarely used to evaluate intestinal duplication, which results from incomplete separation of the intestine from the primitive neurenteric canal and is typically an incidental finding on prenatal US or presents with a mass effect after birth. MRI is occasionally used to demonstrate the spatial relationship between the mass and the bowel, thereby confirming the sonographically suspected diagnosis. In older children, bowel obstruction can also result from encasement of a bowel loop by a benign mass such as an inflammatory pseudotumor. The tumor extent and its obstructive effects can be evaluated by MRI (Fig. 17.2). Anorectal Anomalies Imperforate anus, or anal atresia, is the most common anorectal malformation, occurring in ca. 1 of 5000 births. The level of the obstruction relative to the levator ani muscle—high, intermediate, or low—can be diagnosed by US. MRI provides information on the developmental status of the sphincter muscles and will also identify fistulas, which may develop between the rectum and the urogenital tract.2,3 The anatomic changes can be diagnosed by T1w SE sequences acquired in all three orthogonal planes with the thinnest slices possible. Fluid-filled fistulous tracts are better revealed on T2w images. Axial slices for demonstration of an imperforate anus are acquired at two levels: one slice through the pubococcygeal muscle where the rectum lies behind the prostate or cervix and is surrounded by the puborectalis sling of the levator ani muscle and the second slice through the ramus of the ischium and the ischial tuberosity to encompass the external anal sphincter (Fig. 17.3). MRI thus provides preoperative information on the level of the defect and its relationship to the levator ani sling as well as on the developmental status of the external anal sphincter muscle. In addition, MRI will reveal suspected fistulas and enables evaluation for concomitant anomalies, e.g., of the genital tract and spinal canal, in the same session. MRI is also indicated in children with fecal incontinence following surgical correction of imperforate anus. In this setting, unless already revealed by preoperative MRI, the examination will provide information on the developmental state of the anal sphincter and other muscles. MRI will also demonstrate anterior displacement of the rectum, which can be corrected in most cases. Displacement of the rectum can cause incontinence if the rectum lies outside the levator sling and external anal sphincter muscle or if the rectum is displaced anteriorly but still within the external sphincter. Inflammatory Bowel Disease Crohn disease is the most common inflammatory bowel disease in childhood, with a prevalence of 1 in 5000. Children are on average 11 years old when the condition is first diagnosed. Ulcerative colitis is less common, affecting 4 in 100 000 children. The mean age at diagnosis is 10.4 years. In children, changes of the bowel wall and mucosa can be diagnosed using US or small-bowel follow-through. However, technical refinements of MRI increasingly enable localization of affected bowel segments and assessment of inflammatory activity. If an MRI examination is performed, unenhanced T1w and T2w imaging is supplemented by a fat-suppressed, contrast-enhanced T1w study using a GRE or SE/TSE sequence. A study of MRI with oral administration of polyethylene glycol in children with Crohn disease has shown that MRI criteria of disease activity—wall thickness of involved bowel, mural signal enhancement after intravenous contrast medium, and length of involved bowel segment—correlate well with the clinical activity index.4 The MRI differentiation between Crohn disease and ulcerative colitis is primarily based on which bowel segments are involved. An advantage of MRI is that it enables transmural assessment.5,6 Fig. 17.3a, b Anterior ectopic anus in an 8-year-old boy (1.5 T). Axial T1w SE image (a) and sagittal T2w single-shot TSE image (b). Anteriorly displaced anus and normal appearance of muscles. MRI has a special role in evaluating complications of inflammatory bowel disease such as fistulas and abscesses. Even an abscess arising from an abdominal organ other than the bowel may occasionally be demonstrated. MRI should therefore always be preferred to CT in children. On T2w images, an abscess has a bright center surrounded by a wall of variable signal intensity. Inflammatory stranding and edema indicate an acute abscess. Delineation from surrounding tissues can be improved by administration of a contrast agent. The enhancement pattern provides clues to the age of an abscess: rim enhancement suggests an acute abscess and uniform enhancement an older abscess (Fig. 17.4). Most fistulas can be adequately assessed without contrast administration on images acquired with a fat suppression technique. A fistula is best revealed if it contains fluid, which has high signal intensity on T2w images. If no fluid is present, only a hypointense or isointense contour is seen. Supralevator fistulas are more clearly depicted than infralevator fistulas. A fistula extending to the anus is detected by an increase in anal signal intensity. A healing fistula may escape detection by MRI. Non-Hodgkin lymphoma (NHL), the most common differential diagnosis of inflammatory bowel disease, is usually suggested by an US examination and confirmed by CT. MRI is less commonly used since oral contrast media are currently not generally administered when examining children. As in adults, the liver parenchyma has short T1 and T2 relaxation times. Consequently, the child’s liver has higher T1 and lower T2 signal intensity than the spleen. Fat-suppressed sequences may provide additional information for characterizing focal liver lesions. Benign Tumors Focal liver lesions are not uncommon in children.7 Hemangioma or hemangiomatosis is one of the most important benign conditions of the liver in childhood. The diagnosis can be made by US or MRI. A definitive diagnosis is possible if multiple hemangiomas can be demonstrated throughout the liver.8 Hemangiomas have a long T2 relaxation time, resulting in low signal intensity on T1w images and very high signal intensity on T2w images (Fig. 17.5). A single hemangioma is sometimes difficult to distinguish from a liver cyst on T2w images. In such cases, a RARE or TSE sequence will establish the diagnosis by depicting a cyst as a homogeneous lesion. If multiple hyperintense lesions are demonstrated throughout the liver in young infants, hemangioendotheliomatosis must be considered in the differential diagnosis. A histologic examination is required for a definitive diagnosis. If the sonographic appearance is indeterminate regarding the diagnosis of a liver abscess, MRI is the next imaging modality employed in children. The same holds true for granuloma. On postcontrast MR images, an abscess shows rim enhancement or, if the lesion is older, complete uniform enhancement. Benign liver tumors such as hamartoma are delineated from the surrounding liver as circumscribed lesions, but their MR signal characteristics do not allow specific characterization, which is only possible histologically. Fig. 17.6a, b Echinococcosis of the liver in a 14-year-old boy (0.23 T). Axial T1w (a) and T2w (b) images. Large lesions of low T1 SI and high T2 SI in both hepatic lobes, consistent with cysts. Another rare benign lesion, adenoma, is hypointense on T2w images and slightly hyperintense on T1w images. MRI is rarely used to diagnose a simple liver cyst. Echinococcosis can also be diagnosed by US, but MRI may provide important information on the extent of abdominal echinococcosis and involvement of other organs (Fig. 17.6). Malignant Tumors Two thirds of all childhood liver tumors are malignant with hepatoblastoma predominating before age 3 and hepatocellular carcinoma (HCC) becoming more common after age 5. Hepatoblastoma The tumor is typically revealed as a well-circumscribed, isolated liver lesion with a tendency to invade the portal vein and liver veins. In conjunction with elevated serum α-fetoprotein, this MRI appearance makes the diagnosis of hepatoblastoma very likely. Hepatocellular Carcinoma HCC is more common in children with bile duct atresia or a metabolic disorder involving the liver such as cystinosis or Wilson disease. Children in whom HCC is suspected on the basis of US findings are examined by MRI. Most HCCs have irregular borders, and a tumor capsule can be demonstrated in 40 % of cases. The presence of a central scar at MRI differentiates HCC from hepatoblastoma. The MR signal intensity is usually nonspecific and inhomogeneous. A characteristic finding is displacement and compression of intrahepatic vessels with secondary invasion. After contrast administration, HCC enhances rapidly, but the degree of enhancement is highly variable (Fig. 17.7). Mesenchymal Sarcoma Hepatic undifferentiated mesenchymal sarcoma is a rare pediatric malignancy diagnosed between 5 and 15 years. The neoplasm is characterized by rapid growth, cystic degeneration, hemorrhage, and necrosis. Degenerative changes within the tumor have low T1 signal intensity. On T2w images, these areas appear hyperintense and typically contain low-signal-intensity septa. A fibrous pseudocapsule also has low signal intensity, while myxoid tumor components have very high signal intensity. The differential diagnosis includes metastases, lymphoma, granuloma, and hamartoma.9 Liver Metastases US continues to be the first-line imaging modality for demonstrating liver metastases in pediatric patients. The MR appearance of liver metastases is highly variable in children. Although they may be indistinct from normal parenchyma on T1w images, most hepatic metastases are of high signal intensity on T2w images. These include metastases from neuroblastoma, a tumor with a tendency to diffusely invade the liver in young children. Hepatic metastases must be differentiated from hamartoma, hemangioma, and abscess. Angiomyolipoma A rare liver tumor in children, angiomyolipoma is depicted by MRI as a well-circumscribed lesion with high signal intensity on non-fat-suppressed T1w and T2w images. Biopsy of Liver Lesions All liver lesions in children require confirmation by biopsy even if the MR appearance and signal characteristics suggest a specific diagnosis. The only exceptions are hemangiomas and cysts. Wilson Disease Wilson disease is a disorder of copper metabolism with deposition of ceruloplasmin–copper complexes in hepatocytes, causing inflammation, fatty transformation, fibrosis, and cirrhosis. Severe cirrhosis is associated with formation of regenerative nodules. Such nodules can accumulate excess iron (siderotic nodules) and are then seen as hypointense foci within the liver on T2w images. Fatty degeneration increases MR signal intensity on nonenhanced images. After contrast administration, inflammatory tissue enhances more intensely than normal liver, and regenerative nodules are revealed as low-signal-intensity lesions. It is still unclear how hepatic signal intensity is affected by copper deposits.10–12 Fig. 17.7a–c Hepatocellular carcinoma in a 15-year-old boy (1.5 T). Axial fat-suppressed T2w image (a) and T1w images acquired after IV contrast administration (b and c). Ill-defined, lobulated tumor of inhomogeneous SI located medially. Tumor displaces intrahepatic vessels and enhances rapidly. Contrast enhancement is heterogeneous and more intense in the tumor periphery. Multiple metastases of variable size in the right hepatic lobe. (Images courtesy of Dr. F. Heinisch, Berlin.) MRI of the head is indicated to identify degenerative changes of the brain, particularly the basal ganglia, in children with Wilson disease who present with neurologic symptoms. Primary hemochromatosis is a rare disease in childhood and is characterized by abnormal gastrointestinal iron absorption and ferritin accumulation in the liver parenchyma, causing cell death and cirrhosis. Secondary hemochromatosis is due to increased iron intake and accumulation of hemosiderin in the cells of the mononuclear phagocyte system (MPS) in the liver, spleen, and bone marrow. The secondary form is observed in children who require repeated blood transfusions because they suffer from thalassemia or other bone marrow diseases such as myelodysplastic syndrome, dyserythropoietic anemia, or aplastic anemia. The paramagnetic effect of hemosiderin shortens T2 relaxation time, resulting in marked hypointensity of the liver, spleen, and bone marrow on T1w sequences (Fig. 17.8). T2 signal intensity of the liver and spleen is also reduced. Measurement of T1 and T2 relaxation times shows that a correlation exists between the amount of excess iron in the liver and the signal intensity difference between liver and muscle. Using this method, iron concentrations of < 100 μg/mg of liver can be differentiated from concentrations > 100 μg/mg. The method is inaccurate at higher iron concentrations.13 A noninvasive modality for monitoring hepatic iron levels is desirable in children undergoing chelation therapy with desferrioxamine. It has been shown that a good intraindividual correlation exists between hepatic iron content and ferritin or the amount of blood received. MRI appears to be more suitable for monitoring chelation therapy compared with measurement of serum ferritin. However, there exist considerable interindividual discrepancies.13,14 Results from larger studies are not available for children. Also, studies investigating whether hepatocellular iron storage can be differentiated from deposition in the MPS on the basis of effects on MR signal intensities have only been performed in adults. The same holds true for the use of MR spectroscopy in iron overload.15 Fig. 17.8 Iron overload of the liver after multiple transfusions in a 13-year-old boy with thalassemia. Axial T1w image shows marked hypointensity of the entire liver. Trauma CT is much faster than MRI and is therefore preferred as the second-line imaging modality in children with acute liver trauma. MRI including MRA can be used after the acute event. MRA may obviate the need for invasive angiography. Bile Ducts Biliary anomalies involving the large bile ducts or gallbladder can be diagnosed using magnetic resonance cholangiopancreatography (MRCP). With MRCP, it is straightforward to visualize choledochal cysts, which are circumscribed ductal dilatations (Fig. 17.9). The most common type is tubular dilatation of the hepatocholedochal duct, which may affect the entire duct including the bifurcation into the right and left hepatic ducts. Caroli syndrome
B. Stoever
Introduction
Indications
Imaging Technique
Coils and Pulse Sequences
Positioning
Sedation
Contrast Media
Contraindications
MRI Appearance of Pathologic Entities
Gastrointestinal Tract
Hepatobiliary System
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree