Chapter 26
Abnormal Fetal Echocardiography
• Describe the echocardiographic protocol for evaluating the fetal heart.
• List the various septal defects and their sonographic appearances.
• Differentiate between a complete and a partial atrioventricular septal defect.
• Name the echocardiographic findings in the tetralogy of Fallot.
• List the echocardiographic findings in a fetus with critical aortic stenosis.
• Describe the sonographic characteristics of hypoplastic left heart syndrome.
• Identify the risk factors associated with congenital heart disease.
• Describe how the sonographer may identify transposition of the great arteries.
Sonographic Evaluation of the Fetal Heart
Fetal Cardiac Rhythm
Fetal Echocardiogram
Ideally, a clear redundant view of the cardiac anatomy occurs when the fetus is at least 20 to 22 weeks of gestational age. Although reports in the literature have demonstrated some congenital heart defects with transvaginal sonography in the first trimester,1 it is difficult to image all of the cardiac anatomy clearly. In addition, some cardiac lesions may not show changes until much later in fetal development (e.g., HLHS).
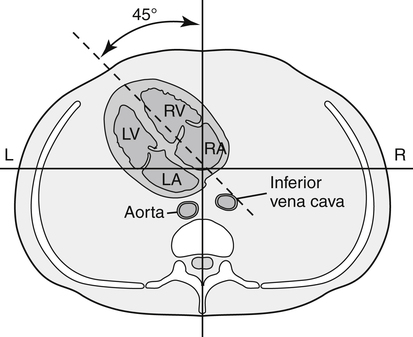
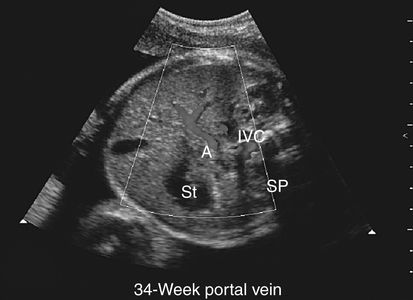
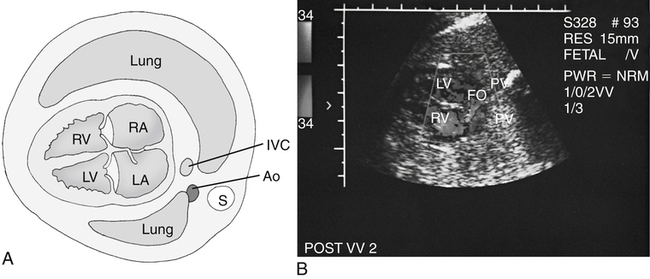
A fetal echocardiogram always begins with the determination of fetal lie, fetal number, activity level, location and size of the placenta, evaluation of the umbilical cord, gestational age, and fluid assessment. The visceroatrial situs should be determined. A transverse view of the abdomen reveals the aorta anterior and to the left of the spine (closest to the left atrium); the inferior vena cava is anterior and to the right with drainage into the right atrium (Fig. 26-1; see Color Plate 33). The stomach should be anterior and leftward.
Four-Chamber View
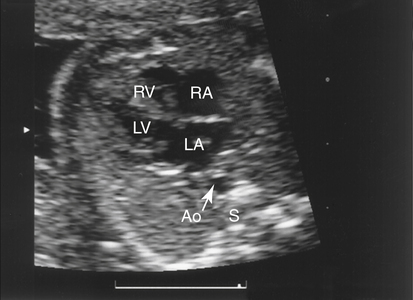
The four-chamber view provides the groundwork for the cardiac examination. The normal position of the fetal heart is in the left thorax with the apex directed about 45 degrees to the left (Fig. 26-2). The size of the heart should be less than one-third of the area of the thorax, and the heart circumference should be less than half of the thoracic circumference. Four chambers of the heart should be clearly present with the right-sided chambers slightly larger than the left-sided chambers (Fig. 26-3).
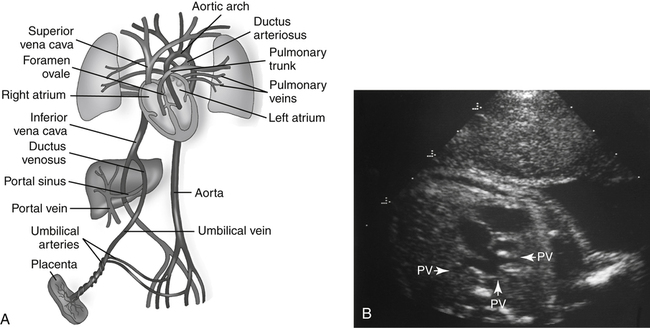
Venous Drainage
The venous drainage of the heart is through the coronary sinus, which may be seen coursing from left to right just superior to the mitral groove. Enlargement of the coronary sinus may prompt evaluation for an abnormality known as left-sided superior vena cava. Four pulmonary veins drain into the left atrium (two upper and two lower). These veins deliver oxygenated blood flow from the lungs to the heart after birth. Usually at least two or three of these veins may be identified as they drain into the left atrium (Fig. 26-4). Color Doppler imaging may aid in their visualization.
Ventricles
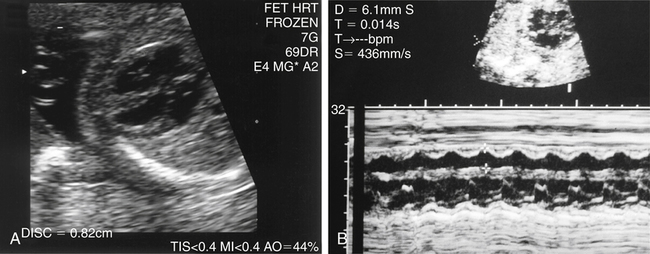
The right and the left ventricles should extend to the cardiac apex, and both ventricles should squeeze simultaneously during systole (Fig. 26-5). There is a bright linear structure near the apex of the trabeculated right ventricle, which is the moderator band. The blood leaves the right ventricle through the pulmonary artery via the right and left pulmonary arteries to their respective lung. The left ventricle is smooth-walled compared with the right ventricle. The aorta delivers blood from the left ventricle to the rest of the body.
Atrioventricular Valves
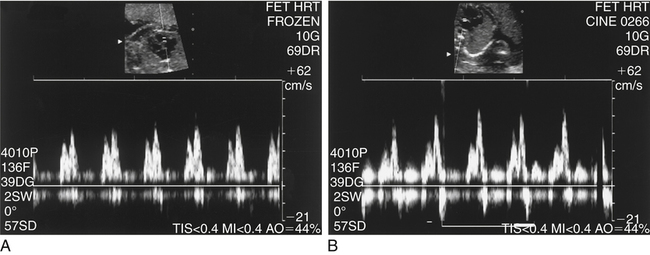
The two atrioventricular valves separate the filling chambers (atria) from the pumping chambers (ventricles). The septal leaflet of the tricuspid valve is slightly more apical than the left-sided mitral valve leaflets. These leaflets should be thin, pliable structures that open fully with ventricular diastole and close completely during systole. Doppler evaluation of the atrioventricular valves shows a biphasic motion as the valve opens in diastole and closes in systole (Fig. 26-6).
Semilunar Valves and Great Arteries
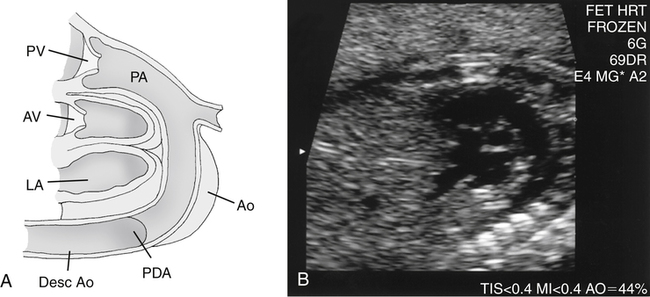
The pulmonary anulus should be at least the same size, if not slightly larger, as the aortic anulus (Fig. 26-7; see Color Plate 34). The long-axis view is best to image the base of the aorta, ascending aorta, and sometimes the arch. The normal aorta should be seen in the “center” of the heart, arising from the base of the left ventricle. Continuity between the anterior wall of the aorta with the interventricular septum is normal; continuity between the posterior wall of the aorta and anterior leaflet of the mitral valve should be present. The pulmonary artery is anterior and to the right of the aorta as it arises from the right ventricular cavity. The main pulmonary artery bifurcates into right and left pulmonary artery branches that drain into the lungs. The semilunar valves should be thin, lunar-shaped cusps that open fully in systole.
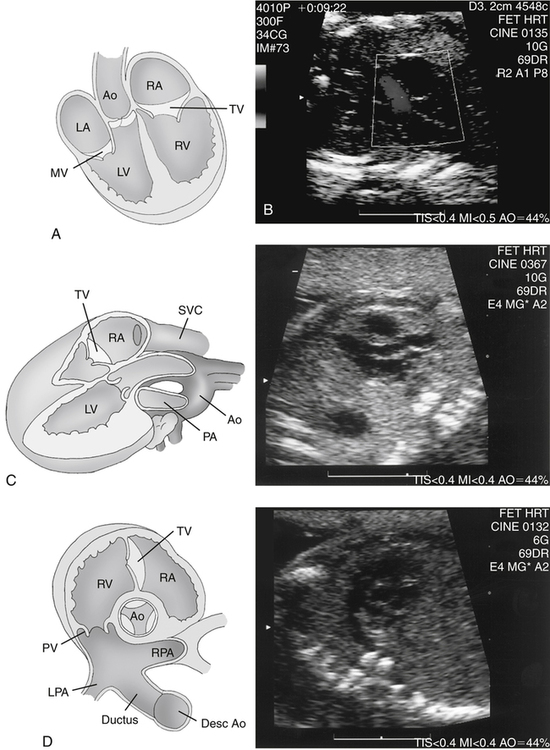
Ductal Arch
The ductal arch may be seen best on the high short-axis view or sagittal view (Fig. 26-8). This short-axis view demonstrates the trifurcation of the main pulmonary artery into the right pulmonary artery (which wraps around the aorta in the short-axis view), the left pulmonary artery, and the large ductus arteriosus. The sagittal view shows the ductus resembling a “hockey stick” as it drains into the descending aorta.
Congenital Heart Anomalies
Atrial Septal Defects
Secundum Atrial Septal Defect
Secundum ASD is the most common atrial defect and occurs in the area of the foramen ovale (Fig. 26-9; see Color Plate 35). Usually an absence of the foramen ovale flap is noted, with the foramen ovale opening larger than normal. The size of the normal foramen should measure at least 60% of the aortic diameter (i.e., if the aorta measures 4mm, the foramen should be at least 2.4mm).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree