Personnel qualifications for physicians include training, board certification, ongoing experience with interpretation and reporting, and continuing medical education. Radiologic technologists must meet appropriate licensure and continuing education requirements. Medical physicists must meet training or board certification requirements and must document continuing experience with specific equipment surveys and continuing education.
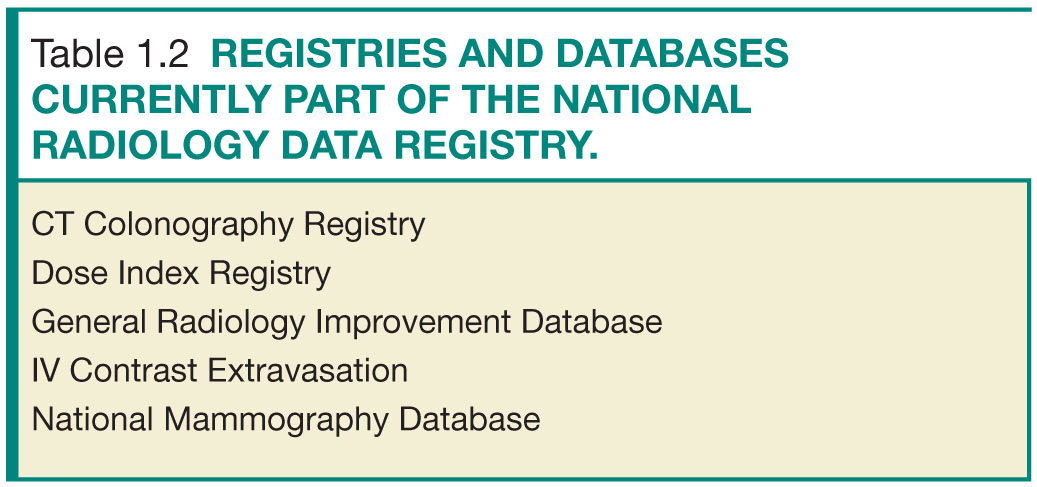
NATIONAL RADIOLOGY DATA REGISTRY
The National Radiology Data Registry (NRDR) is an ACR program that consists of several registries (Table 1.2) and allows participating facilities to compare their own benchmarks with regional and national peers. Currently, the NRDR consists of the National Oncology PET Registry (NOPR), the CT Colonography Registry, the General Radiology Improvement Database (GRID), the National Mammography Database (NMD), IV Contrast Extravasation Registry (ICE), and the Dose Index Registry (DIR).3 In 2014, the NRDR was designated a Qualified Clinical Data Registry (QCDR) for the Centers for Medicare & Medicaid Services’ (CMS) Physician Quality Reporting System (PQRS).
The DIR enables facilities to compare their CT dose indices with aggregate data from other participating facilities, itemized by body part and exam type (Fig. 1.1). DIR data can be used for the practice quality improvement (PQI) component of the American Board of Radiology (ABR) Maintenance of Certification (MOC) program.4
The CT Colonography Registry tracks both process measures and outcome measures for CT colonography (CTC) (Fig. 1.2). Process measures include optimal bowel cleansing and distention, rate of adequacy of diagnostic CTC exam, and rate of adequacy of screening CTC examination. Outcome measures tracked include rate of colonic perforation, true positive rate, and extracolonic findings.5
GRID consists of multiple measures related to MRI, patient safety, process, and outcomes (Table 1.3). Current process measures include patient wait time, time from order to exam, reacquisition rate, and report turnaround time. Outcome measures include rates of nondiagnostic liver and lung biopsies, rate of lung biopsies resulting in pneumothorax that require tube drainage, rates of contrast extravasation, and rate of nonconcordant stereotactic breast biopsies.6 Each participating site is provided with a feedback report showing performance and comparison with other GRID sites (Fig. 1.3).
ICE enables facilities to track their own rates of intravenous contrast extravasation and review treatments and outcomes. Furthermore, participating sites can compare their respective data with those of other institutions, and a PQI project involving ICE is available to participating radiologists.7
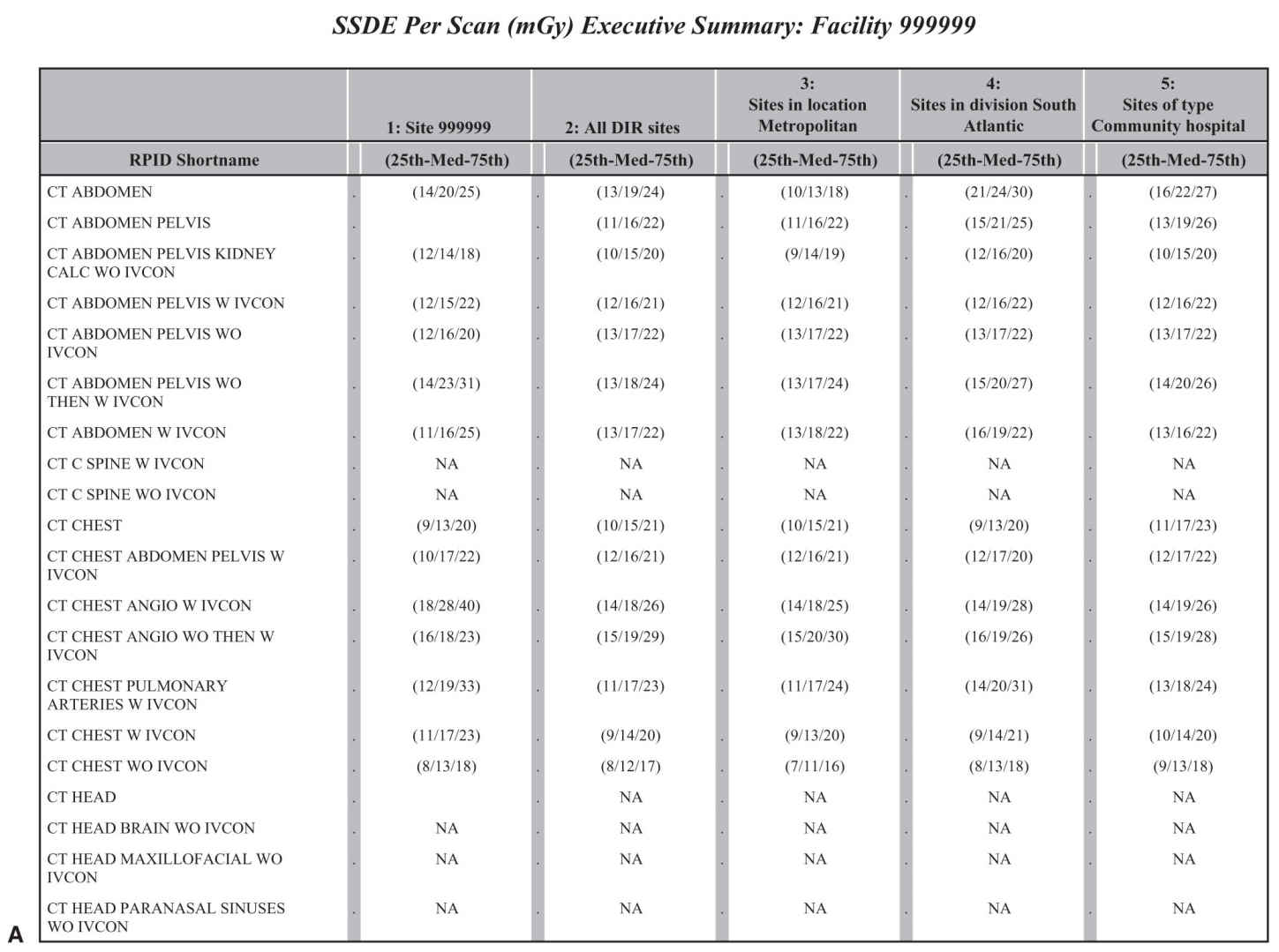
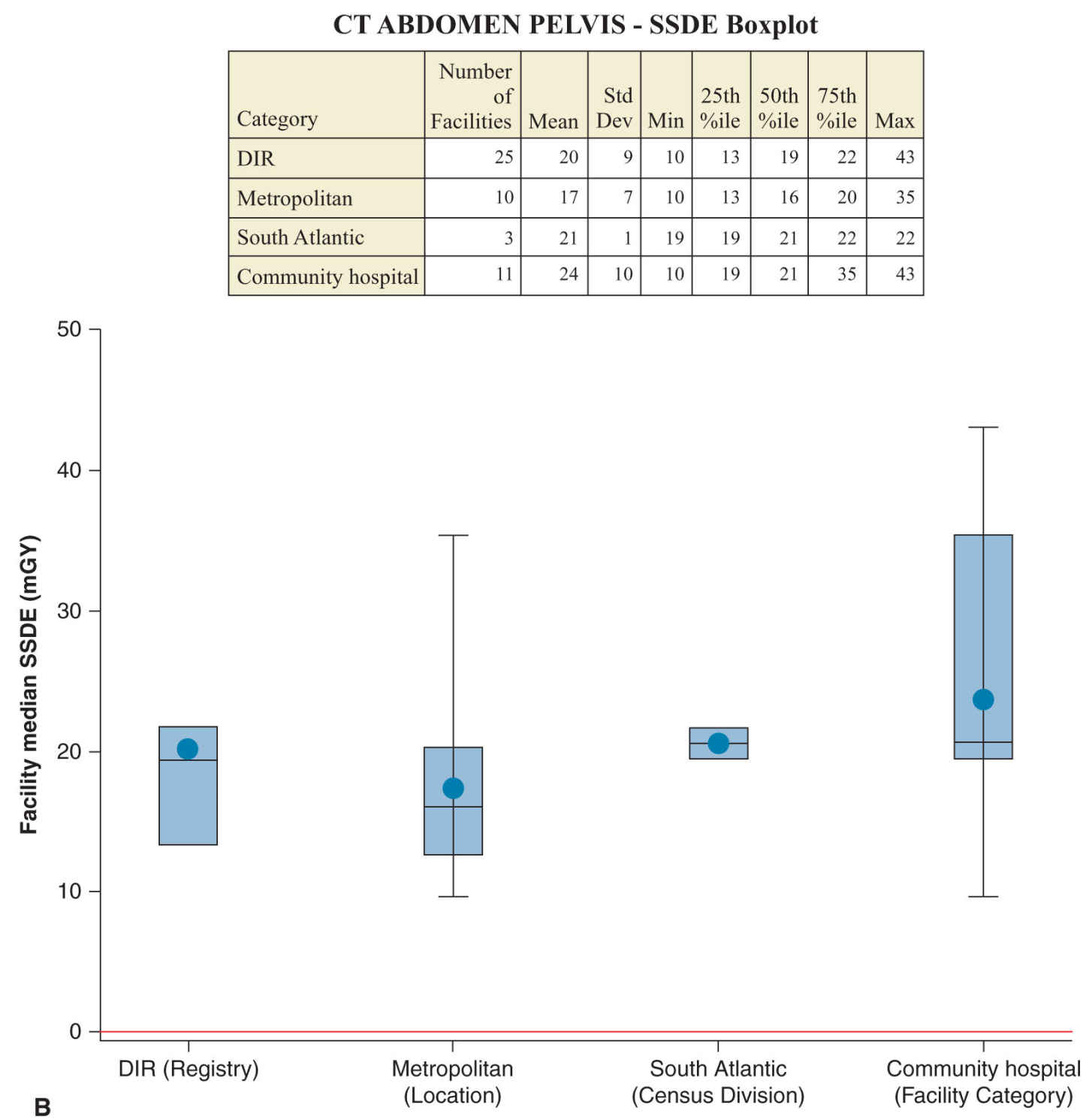
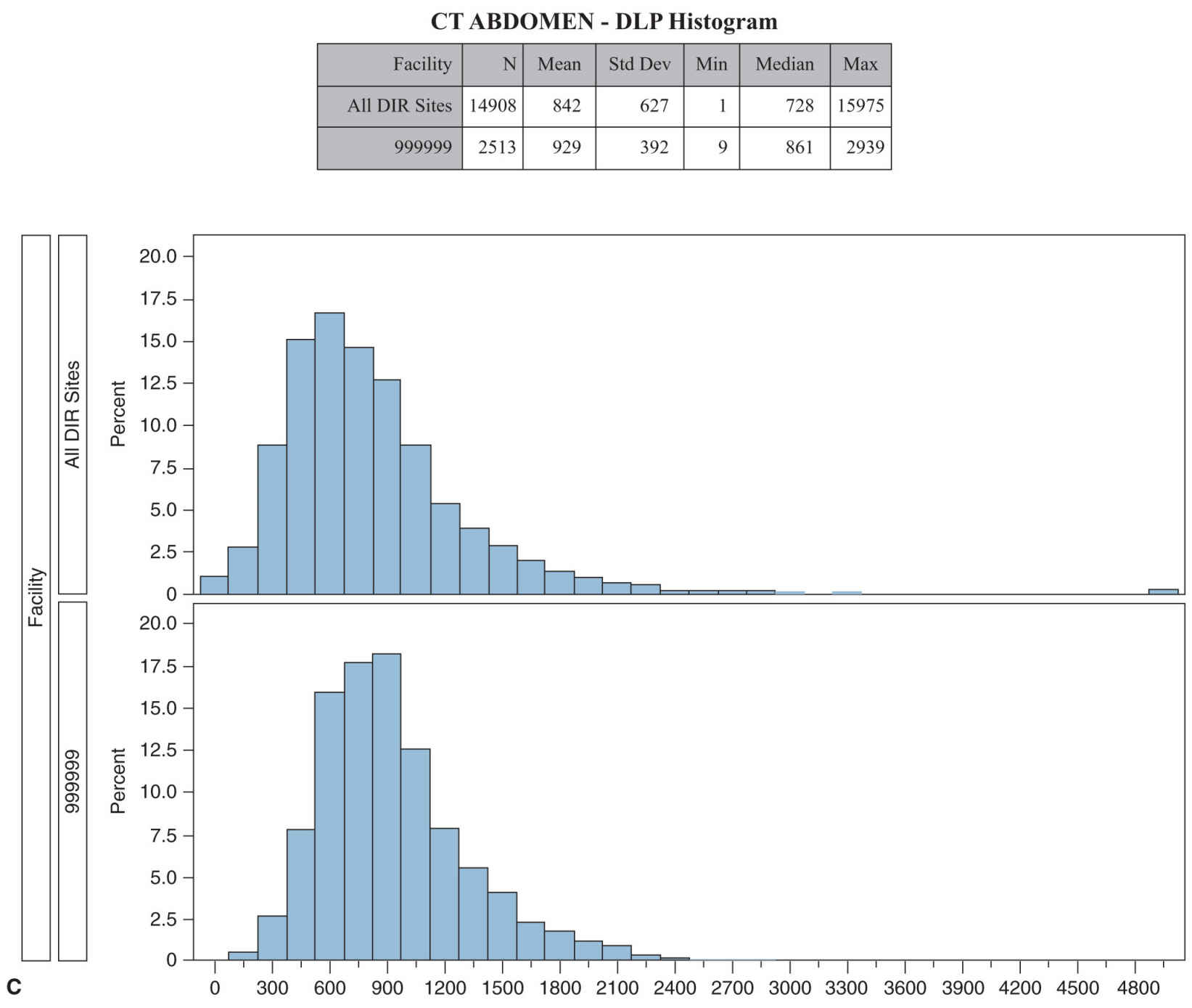
FIG. 1.1 ● A-C: Selected pages from a sample report of ACR’s Dose Index Registry.
NMD allows participating facilities to compare mammographic data with other facilities and with national benchmark data provided by the National Cancer Institute–funded Breast Cancer Surveillance Consortium (Fig. 1.4). Data collected for NMD mirror those mandated by MQSA, and several third-party software packages used in mammography reporting can transmit these data to the NMD. Four outcome measures are currently part of the NMD: diagnostic mammography positive predictive value, screening mammography positive predictive value, cancer detection rate, and abnormal interpretation rate (recall rate).8
ACR DIAGNOSTIC IMAGING CENTER OF EXCELLENCE
ACR offers designation as a Diagnostic Imaging Center of Excellence9 to facilities that meet program requirements, which include ACR accreditation in all modalities employed for which ACR accreditation is offered, DIR and GRID participation, Image Gently and Image Wisely pledges, and a comprehensive site survey. The site survey assesses governance, personnel, facility organization and management, physical environment, equipment and information technology infrastructure, radiation and general safety, quality management, policies and procedures, patient rights, and medical records.
ACR-DESIGNATED LUNG CANCER SCREENING CENTER
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree