(1)
Department of Radiology, John H Stroger Jr Hospital of Cook County, Chicago, IL, USA
Miliary Nodules
Imaging Features
1.
Innumerable, tiny, both sharply and poorly defined noncalcified nodules, 1–4 mm throughout both lungs, and generally of uniform size
2.
Diffuse random distribution in both lungs
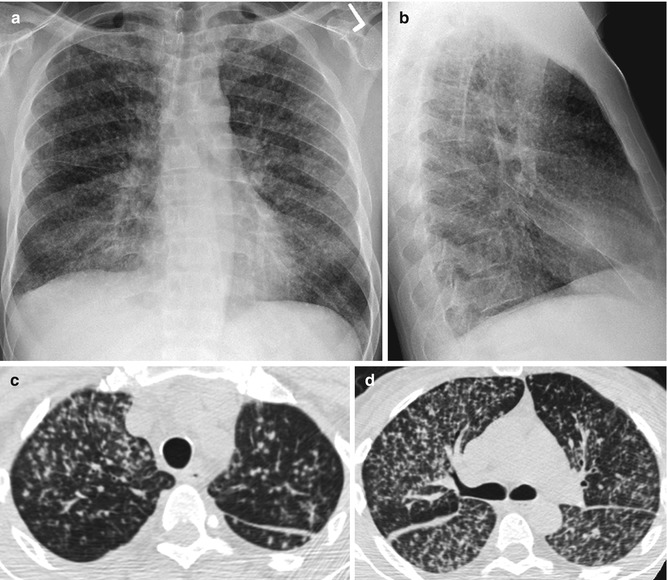
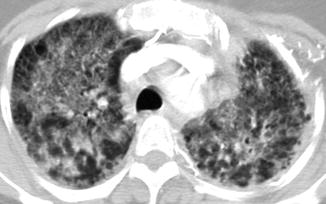
Fig. 8.1
Miliary nodules. History of TB infection presented with cough, fever, and night sweats. (a, b) PA and lateral chest x-ray (c, d) and axial CT of the chest show miliary nodules in random distribution with lower lobe predominance
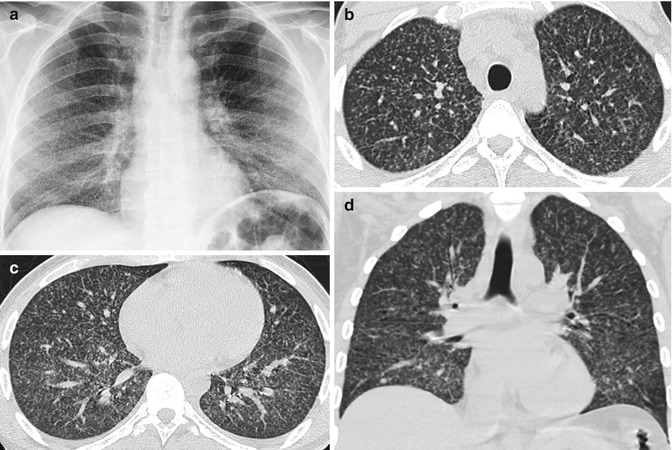
Fig. 8.2
Coccidiomycosis. (a) PA chest x-ray, (b, c) axial CT, and (d) coronal reformatted CT images show miliary nodules in random distribution and mild basilar predominance
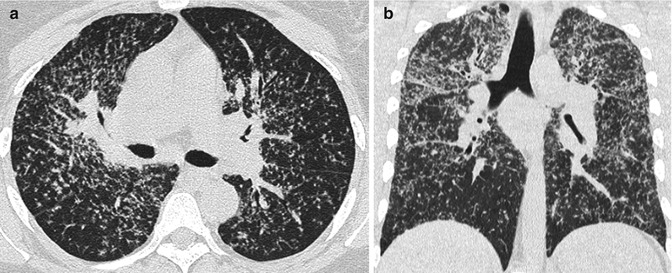
Fig. 8.3
Patient with history of sarcoidosis. (a, b) Axial and coronal reformatted CT show miliary nodules with upper lobe predominance and bilateral hilar lymphadenopathy. Nodules involving pleural surface and septa
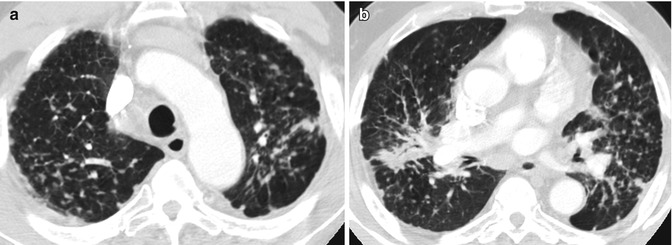
Fig. 8.4
Silicosis. (a, b) Axial CT shows miliary nodule with fibrosis more in the upper lungs involving the septa and pleural surface
Centrilobular Nodules
Imaging Features
1.
Nodules separate from the pleural surface, fissures, and interlobular septa.
2.
May be dense or ground glass in attenuation.
3.
May be a few millimeters to a centimeter in size.
4.
May be a single or a rosette of nodules.
5.
May be patchy or diffuse in distribution.
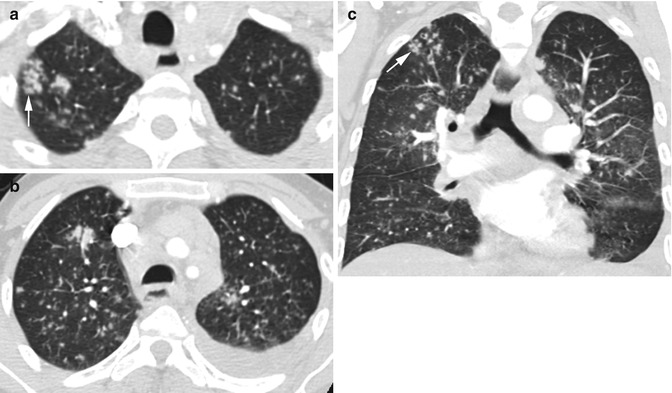
Fig. 8.5
Active TB. History of immune-compromised syndrome with active TB infection. (a, b) Axial and (c) coronal reformatted CT of the chest show centrilobular micronodules sparing the pleural surfaces and fissures and are of varying sizes. Some nodules in the right upper lobe are arranged in rosette, best seen in coronal reformatted image (arrow in a, c), and small left effusion (b, c)
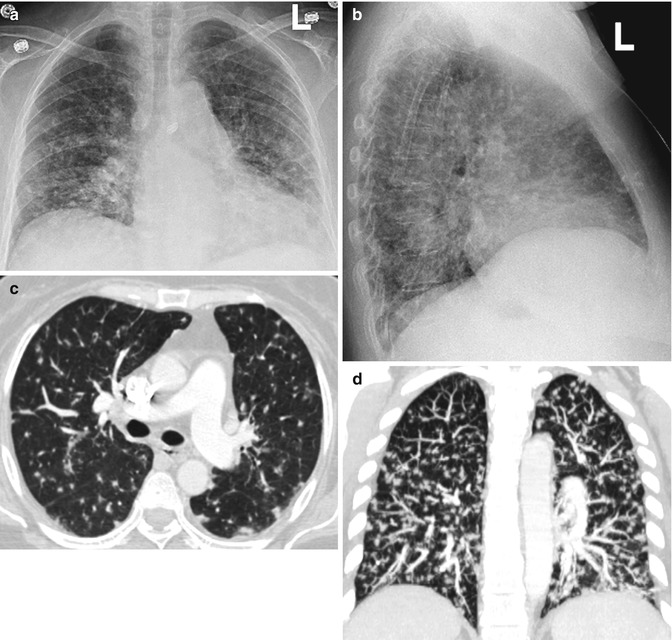
Fig. 8.6
Centrilobular nodules in a patient with ALL and candida infection. (a, b) Chest PA and lateral views, (c, d) axial CT, and coronal reformatted image show micronodules sparing the pleural surface and fissures
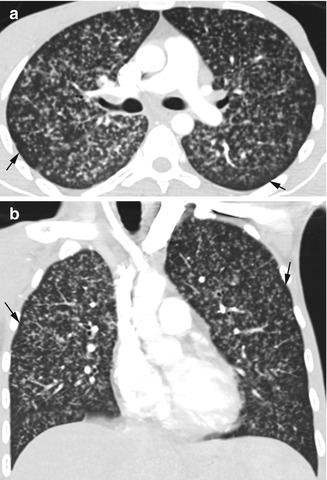
Fig. 8.7
Centrilobular distribution of histoplasma infection in an HIV-positive patient. Urine was positive for histoplasma antigen. (a, b) Axial and coronal reformatted images show diffuse micronodules in both lungs, sparing the pleural surface and subpleural region (arrows)
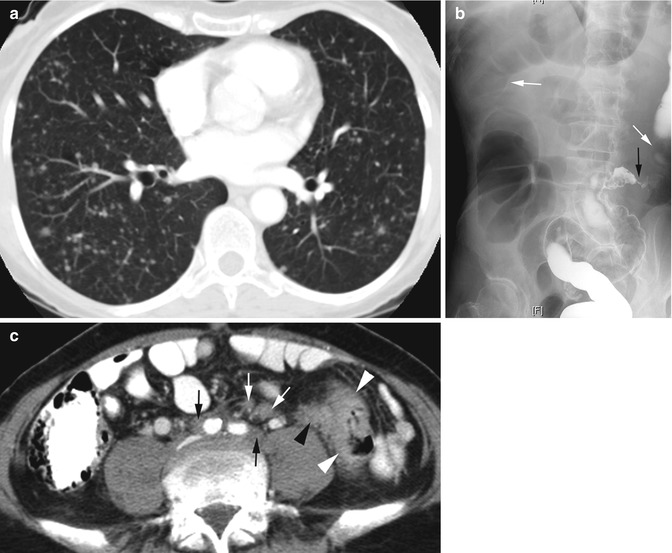
Fig. 8.8
Metastasis with centrilobular nodules from colon cancer. (a) Axial CT of the chest shows centrilobular lung nodules of varying size not involving fissures and abutting the pleura. (b) Double-contrast barium enema shows focal constriction of the proximal sigmoid colon (black arrow) and dilatation of adjacent descending colon (white arrows). (c) Axial CT of the abdomen shows diffuse wall thickening of the sigmoid colon in the same area as seen in the enema study (white arrowheads) with extension of tumor medially outside the colon over the left psoas muscle (black arrowhead). Enlarged lymph nodes or tumor and linear strands extending to common iliac arteries (thin white arrows) and surrounding the iliac arteries (thin black arrows)
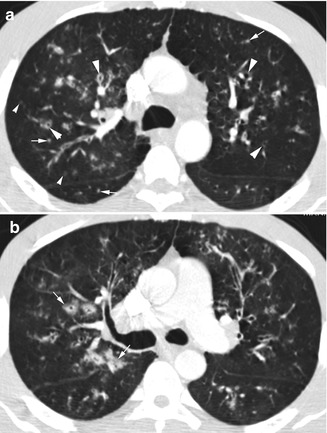
Fig. 8.9
Viral cellular bronchiolitis. (a) Axial CT shows diffuse thick-walled bronchi and bronchioles (thick arrowheads). Diffuse centrilobular nodules are seen, some of which are solid (arrows) and some are subsolid (thin arrowheads). (b) Axial CT at lower level shows some of the thick-walled bronchi to have surrounding ground-glass density (arrows)
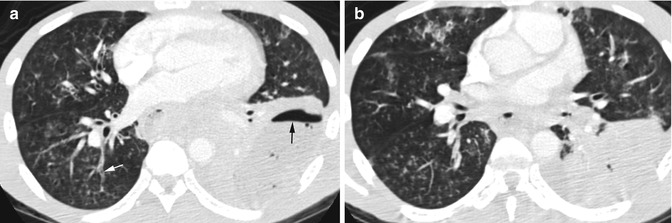
Fig. 8.10
Endobronchial abscess spreads with centrilobular nodules. (a, b) Axial CT shows centrilobular nodules in the middle lobe and right lower lobe from endobronchial spread of the left lower lobe abscess with air-fluid level (black arrow). A right lower lobe bronchus is filled with soft tissues (white arrow)
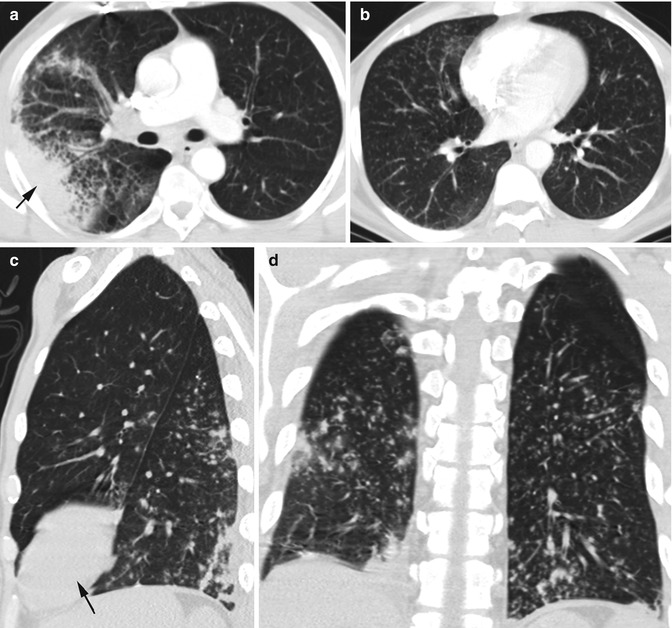
Fig. 8.11
Pneumonia with centrilobular nodules: (a) Axial CT shows consolidation RUL (arrow in a, c) with surrounding interstitial thickening. (b) Axial CT, (c) sagittal, and (d) coronal reformatted images show diffuse centrilobular nodules of the lower lobes bilaterally

Fig. 8.12
Centrilobular nodules due to aspiration. Patient with achalasia. Axial CT shows multiple centrilobular nodules mainly of ground-glass density, distributed mostly in the middle and right lower lobes, fluid-filled right lower lobe bronchus (white arrow), and dilated esophagus (black arrow)
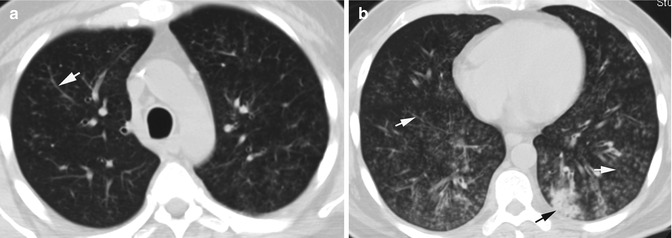
Fig. 8.13
Centrilobular nodules from aspiration. Patient with history of gastric carcinoma experienced choking during eating. (a, b) Axial CT shows diffuse ground-glass nodules in both lungs with lower lobe and posterior segment predominance, some with tree-in-bud sign (white arrow) and small focal consolidation in the left lower lobe (black arrow)
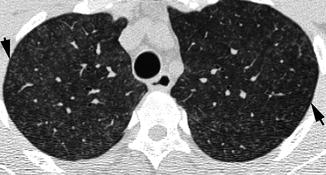
Fig. 8.14
Hypersensitivity pneumonitis in a bird breeder. Diffuse ground-glass centrilobular bilaterally with subpleural sparing (arrows)

Fig. 8.15
Respiratory bronchiolitis. History of chronic cigarette smoking. (a, b) Axial CT shows bronchial wall thickening in RUL (thin arrow), centrilobular emphysema (arrowheads), and centrilobular nodules (thick short arrows). (c) Axial CT shows diffuse centrilobular nodules and mosaic attenuation (white arrows) from obstructive bronchiolitis. (d) Coronal reformatted image shows multiple ground-glass centrilobular nodules (black arrows) which appear more at the lower lung field due to emphysematous changes in the upper lungs
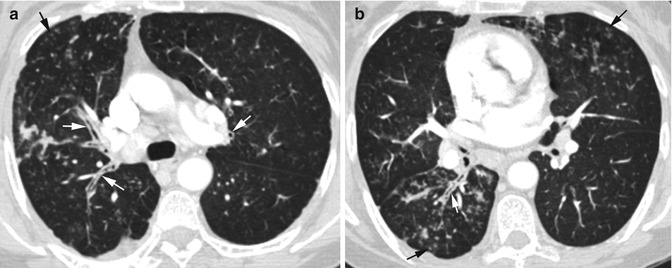
Fig. 8.16
Diffuse panbronchiolitis mimicking asthma. (a, b) Axial CT shows bronchial thickening (white arrows) with diffuse centrilobular nodules (black arrows) of both lungs
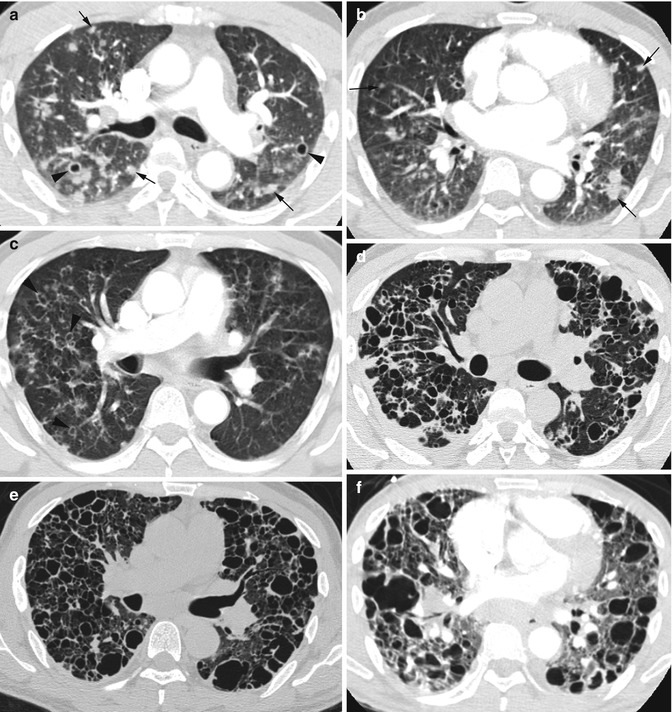
Fig. 8.17
Langerhans cell histiocytosis. Same patient in 2004, 2005, 2006, and 2008. Axial CT (a, b) in 2004 shows multiple mostly solid nodules (arrows) with upper lobe predominance and in centrilobular distribution. A few thick-walled cysts are also seen (arrowheads). (c) In 2005, the cystic spaces have increased (arrowheads) with decrease of solid nodules at same level as (a). (d) 2006, shows further increase in size and a number of the cystic spaces, some are thick walled and others are thin walled. (e, f) 2008, shows further progression in cystic spaces with upper lobe predominance and decrease in normal lung
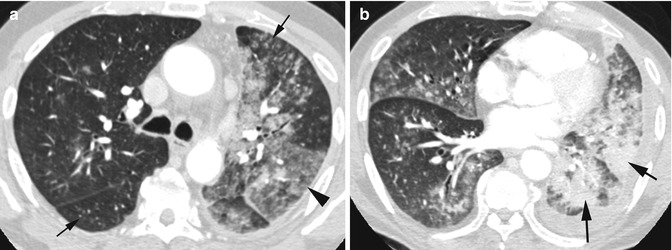
Fig. 8.18
Invasive mucinous adenocarcinoma. (a, b) Axial CT shows multicentric densities with solid (thick arrows) and subsolid areas (arrowhead) in the left lower lobe and lingula and diffuse solid and subsolid centrilobular nodules (thin arrows) bilaterally
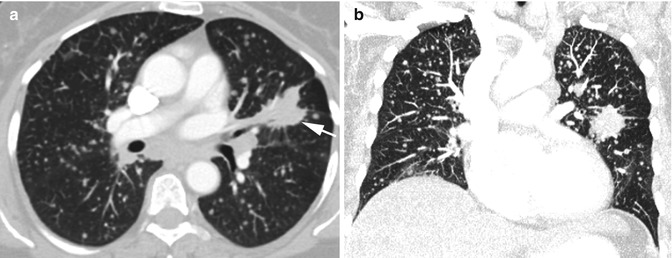
Fig. 8.19
Adenocarcinoma with metastasis. (a, b) Axial and coronal reformatted CT shows a solid invasive spiculated mass in the left perihilum with pleural tags, extension to left hilum (arrow), and diffuse bilateral centrilobular solid nodular metastasis
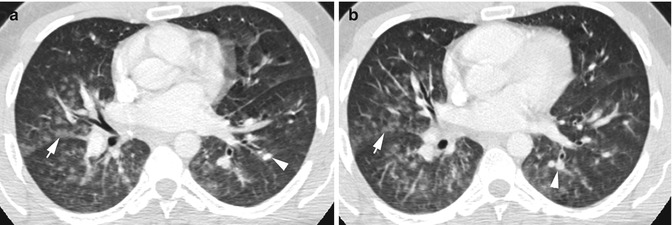
Fig. 8.20
Acute pulmonary edema, postoperative (angiocentric disease). (a, b) Axial CT shows centrilobular ground-glass nodules mostly in the medial and central lungs and more at the bases along the fissures but not involving them (arrows). Dilated arteries more at the lower lung field (arrowhead)
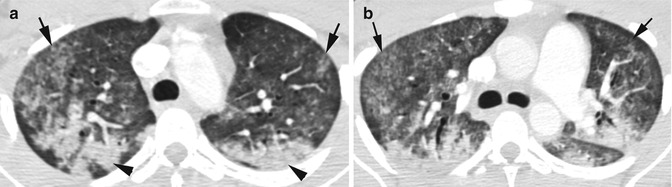
Fig. 8.21
Pulmonary hemorrhage (angiocentric disease) in a patient with SLE and hemoptysis. (a, b) Axial CT shows ground-glass centrilobular nodules bilaterally, sparing the pleural surface (arrows) and lobular consolidation (arrowheads)
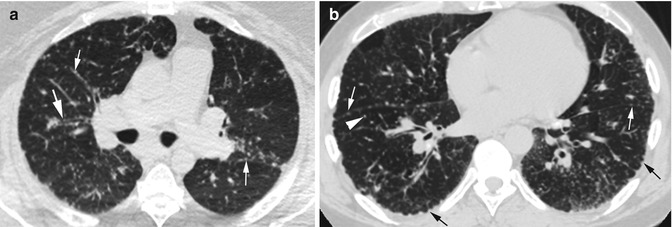
Fig. 8.22
Sarcoidosis, perilymphatic disease. Axial CT shows sharp nodules. (a) Nodules along the bronchial wall (thick white arrow) and vascular markings (thin white arrow). (b) Along fissures (thin white arrow) and centrilobular nodules (thick arrowhead) and nodular thickening of pleural surfaces (black arrows)
Tree-in-Bud Sign
Diagnosis
Centrilobular Nodules—Tree-in-Bud Sign
Imaging Features
1.
Branching appearance with most peripheral nodules several millimeters from the pleural surface
2.
Centrilobular clusters of nodules
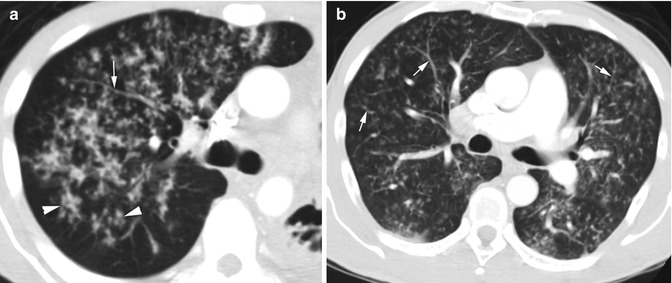
Fig. 8.23
TB in two patients. (a, b) Axial CT shows diffuse centrilobular nodules and with tree-in-bud pattern (arrows). Some of the nodules show centrilobular clustering (arrowheads)
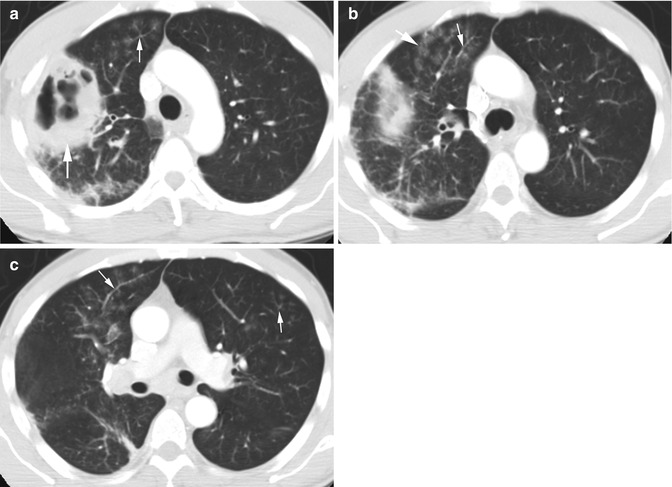
Fig. 8.24
Pseudomonas lung abscess with endobronchial spread. (a) Axial CT shows thick-walled abscess in RUL (thick white arrow) with ground-glass nodules at the end of the bronchi adjacent to it (thin white arrow). (b) Tree-in-bud distribution of ground-glass nodules (thin white arrow) and also linearly arranged ground-glass nodules in bronchovascular distribution (thick white arrow). (c) Axial CT of the chest at lower level shows bilateral centrilobular nodules, some with tree-in-bud arrangement (arrow)
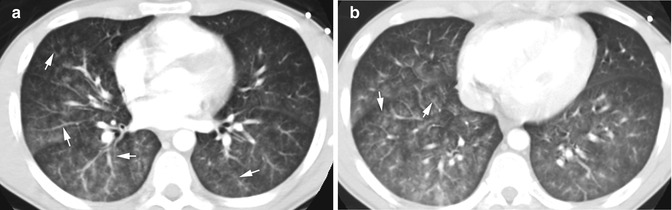
Fig. 8.25
Streptococcus mitis infection. Patient with pre-B-ALL and neutropenic fever. Axial CT of the chest (a, b) shows diffuse ground-glass nodules linearly arranged along the bronchovascular bundles, some showing tree-in-bud distribution (arrows)
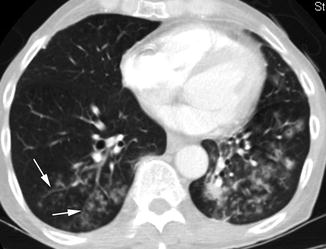
Fig. 8.26
Laryngeal carcinoma with endobronchial spread. Axial CT shows diffuse subsolid nodules, some with tree-in-bud arrangement (white arrows)
Centrilobular Low Attenuation
Imaging Features
1.
Abnormal areas of low attenuation of the secondary lobule.
2.
Walls are imperceptible in emphysema.
3.
Thick walls are seen in bronchiolectasis and cavitary nodules.
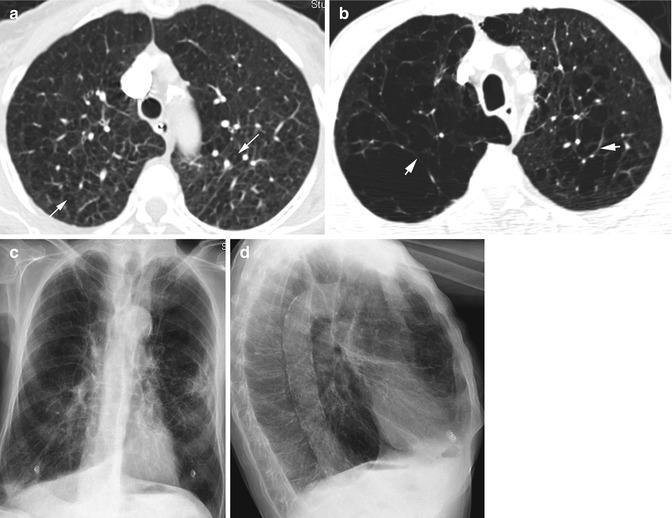
Fig. 8.27
(a, b) Centrilobular (centriacinar) emphysema. (a) Axial CT shows low-attenuation areas in the center of lobules with imperceptible walls. Centrilobular arteries (arrows) are seen in some of the low-attenuated areas. (b) Axial CT of different patients shows larger centrilobular emphysema. Thick visible walls (arrows) with prominent veins are due to fibrosis of the interlobular septa. (c, d) PA and lateral chest x-ray show hyperinflated lungs with flattened diaphragms and increased retrosternal space
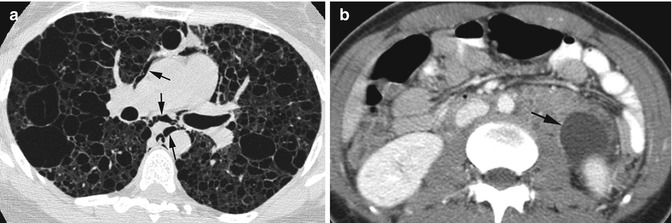
Fig. 8.28
Lymphangioleiomyomatosis. (a) Axial CT of the chest shows diffuse cysts with well-defined walls with intervening normal lung parenchyma and with pneumomediastinum (arrows). (b) Axial CT of the upper abdomen shows retroperitoneal lymphangioma with a large fluid collection adjacent to the upper pole left kidney (arrow)

Fig. 8.29
TSC-associated LAM. (a, b) Coronal and sagittal reformatted CTs show diffuse cysts throughout both lungs (arrow). (c) Axial CT of the abdomen shows angiomyolipoma with fatty foci in the left kidney (arrow). (d–f) CT head, (d) axial, (e, f) and coronal reformatted images show subependymal hamartomas with calcification (arrow) and facial angiofibromas (adenoma sebaceum) (arrowheads)
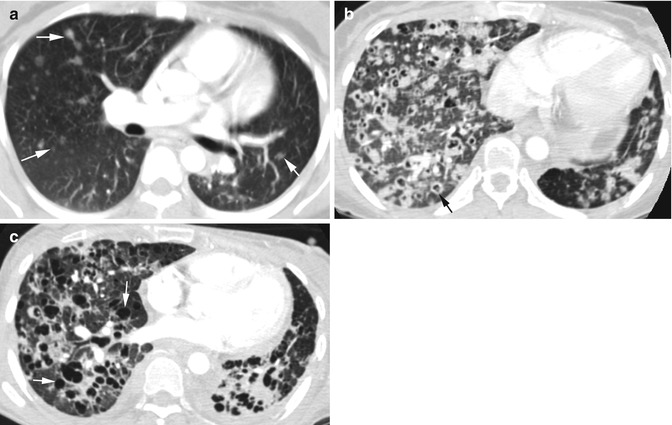
Fig. 8.30
Cavitating metastasis from adenocarcinoma of the lung with left upper lobectomy. Axial CT of the chest (a) shows multiple small nodules of various sizes in both lungs (arrows). (b) Two years later multiple cavitating nodules are seen, some with thick walls (arrow). (c) Five months later the nodules show increased cystic changes, some with very thin walls (arrows)
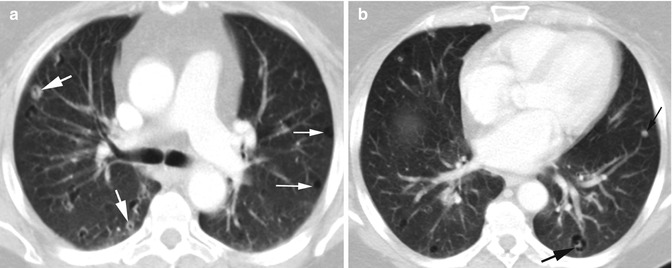
Fig. 8.31
Cystic changes in pulmonary metastases of endometrial carcinoma. (a, b) Axial CT shows the metastasis to range from solid (thin black arrow), thick-walled cavitary (thick white arrow), cystic with solid center (thick black arrow), and purely cystic lesions (thin white arrow)
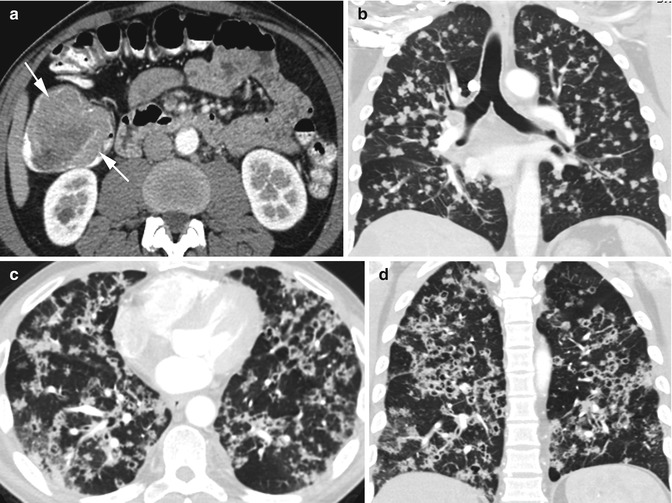
Fig. 8.32
Cavitating centrilobular lung metastasis from colon cancer. (a) Axial CT of the upper abdomen shows a large adenocarcinoma in the proximal ascending colon (arrows). (b) Coronal reformatted image of chest few months later shows diffuse solid centrilobular nodular metastasis bilaterally. (c, d) Axial and coronal reformatted images 1 year later show increase in pulmonary nodular metastasis which now show cavitation
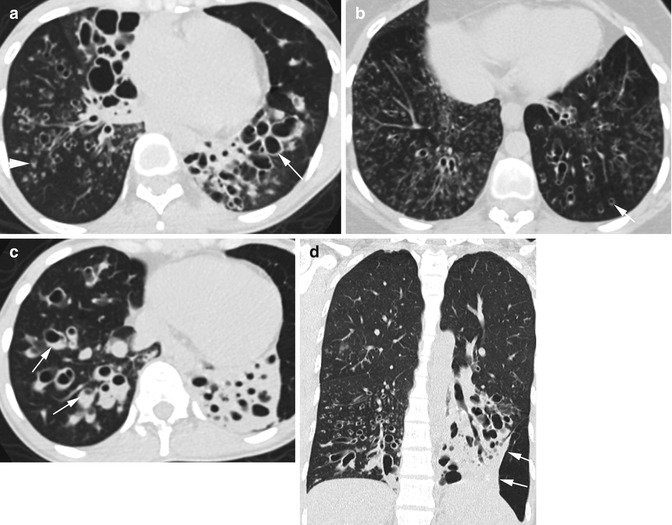
Fig. 8.33
Bronchiolectasis. Dilated bronchi and bronchioles mostly in the lung bases, in two patients. Patient 1: Axial CT (a, b) shows bronchiectasis (thin long arrows) with tree-in-bud centrilobular nodules, some of the latter have central lucencies due to dilated bronchioles (thick white arrows). Patient 2: (c) Some of the bronchi have fluid (arrows). (d) Coronal reformatted image shows the dilated bronchi in the left lower lobe are surrounded with fibrosis as seen by retraction (arrows)
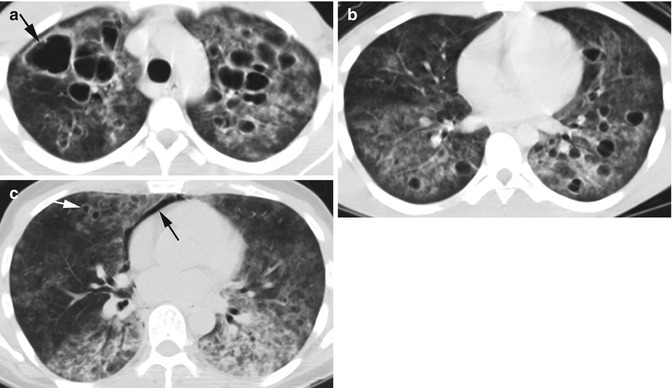
Fig. 8.34
Cystic pneumocystis infection. (a, b) Axial CT shows thick-walled cysts (arrows) in both lungs, with larger cysts in the upper lobes. The cysts are surrounded by diffuse ground-glass infiltration. (c) Axial CT of different patients shows pneumomediastinum (black arrow) in addition to bilateral ground-glass infiltrations and small cysts (white arrow)
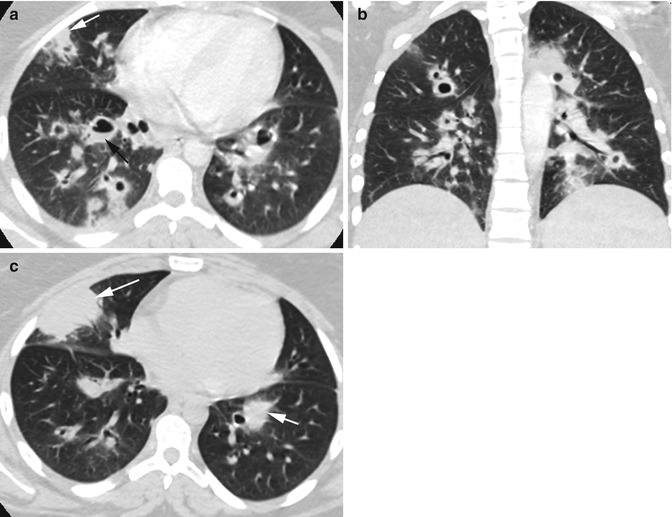
Fig. 8.35
Fungal pneumonia with cavitating nodules. History of a 19-year-old patient with steroid-resistant ulcerative colitis. (a, b) Axial and coronal reformatted CTs show multiple thick-walled cavitary nodules, some with air-fluid level (black arrow) mostly in the mid-lung zone with small areas of consolidation (white arrows). (c) Axial CT several months later shows increase in consolidation areas (arrows) and decreased cavitary nodules
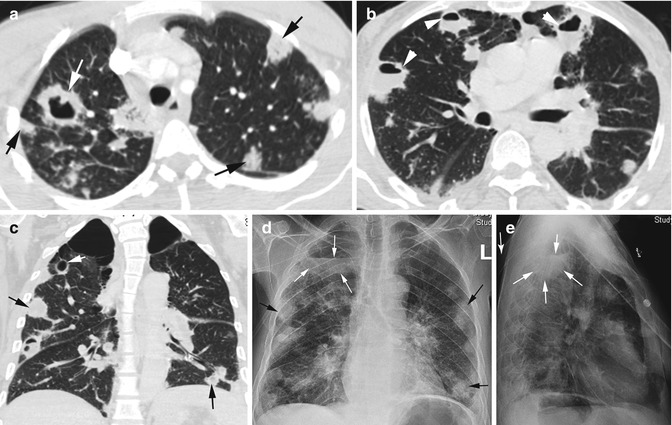
Fig. 8.36
Septic emboli. History of IV drug abuse. (a, b) Axial and (c) coronal reformatted CTs show multiple nodules in the periphery of the lungs and mostly pleural based. Some nodules are solid (black arrows), some show cavitation (white arrow), and some with air-fluid levels from abscess formation (arrowheads), and all with shaggy borders. (d, e) PA and lateral chest x-ray shows peripheral nodules, some showing cavitation (black arrows). A thin-walled infected bulla is also seen in the right lung apex with air-fluid level (white arrow)
Panlobular Abnormalities
Imaging Features
1.
Involvement of single or groups of lobules with normal-appearing adjacent lobules—mosaic attenuation
2.
Lobular increased attenuation from consolidation or ground-glass density
3.
Lobular low attenuation from decreased perfusion, air trapping, or lobular destruction
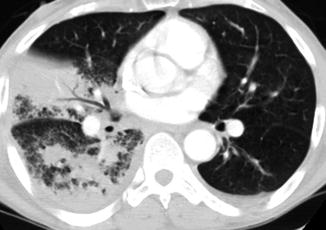
Fig. 8.37
Lobular consolidation from bronchopneumonia. Axial CT shows panlobular consolidation involving a large area of consolidation in RML and multiple small groups of lobules in RLL
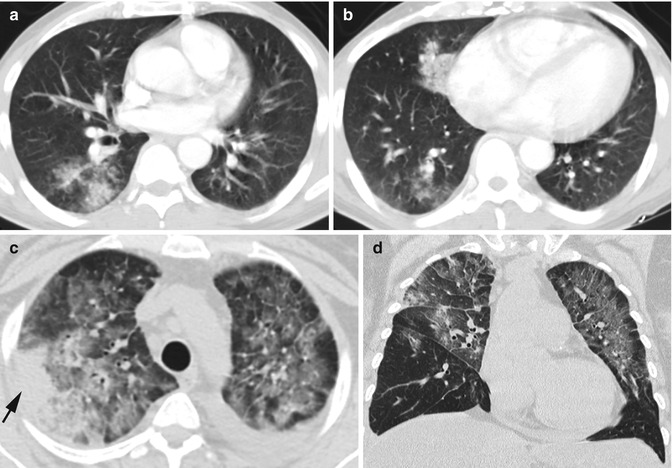
Fig. 8.38
Lobular ground-glass opacity from pneumonia. (a, b) Axial CT in a patient with community-acquired pneumonia with groups of lobules involving the right lower and middle lobes. (c, d) Axial and coronal reformatted CTs in different patients with Legionella pneumonia show focal lobular peripheral consolidation in RUL (arrow) and ground-glass lobular involvement in the rest of the bilateral upper lobes
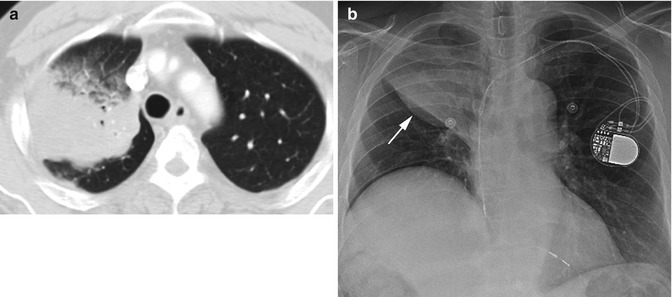
Fig. 8.39
Adenocarcinoma. Axial CT (a) shows large lobular consolidation of the right upper lobe. (b) PA chest x-ray shows Golden “S” sign formed by mass and partial collapse of RUL (arrow)
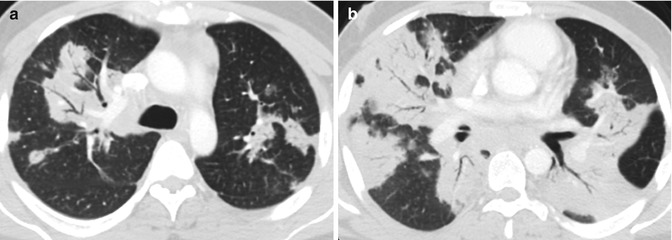
Fig. 8.40
Hodgkin’s lymphoma biopsy proven. (a, b) Patient presented with night sweat and loss of weight. Axial CT shows multiple areas of lobular consolidation
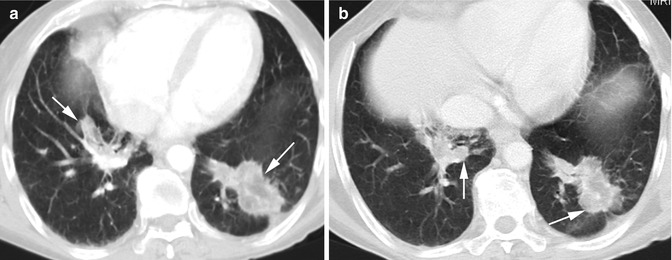
Fig. 8.41
Lipoid pneumonia. (a, b) Axial CT shows with well-marginated ground-glass focal densities in both lung bases (arrows) with density measurement of fatty tissue. Patient was a baker by trade
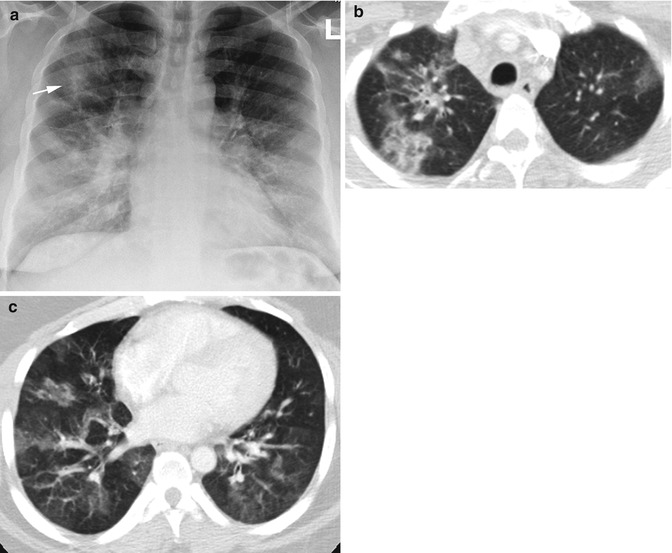
Fig. 8.42
Eosinophilic pneumonia in a patient with congenital erythropoietic porphyria. (a) Chest x ray shows patchy infiltration in the right upper lobe (arrow). (b, c) Axial CT shows lobular ground-glass densities bilaterally more at the bases
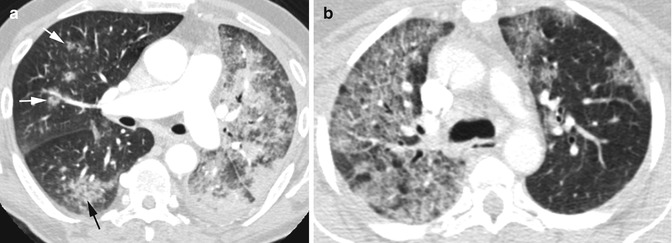
Fig. 8.43
Lung carcinoma. Axial CT shows (a) mucinous adenocarcinoma with multiple focal solid areas and panlobular ground-glass tumor infiltration on the left side, focal lobular infiltration of the right lower lobe (black arrow), and subsolid nodules in the middle lobe (white arrows). (b) Non-small cell carcinoma with panlobular infiltrate of the right lung and patchy lobular ground-glass infiltrate of the left side
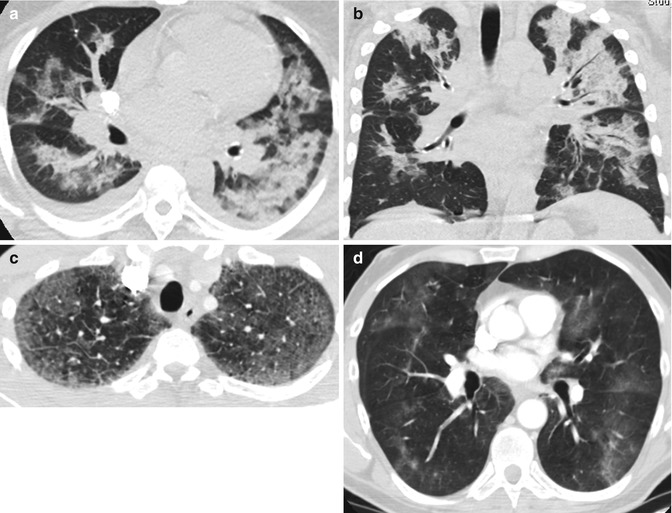
Fig. 8.44
Pneumocystis infection in three patients. (a, b) Axial and coronal reformatted CTs show lobular consolidation and ground-glass densities bilaterally. (c, d) Axial CTs in two different patients show diffuse lobular ground-glass opacities bilaterally
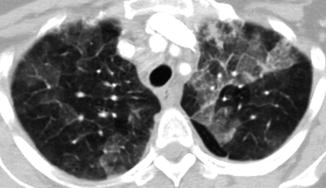
Fig. 8.45
Hypersensitivity pneumonitis. Axial CT shows lobular ground-glass opacities bilaterally
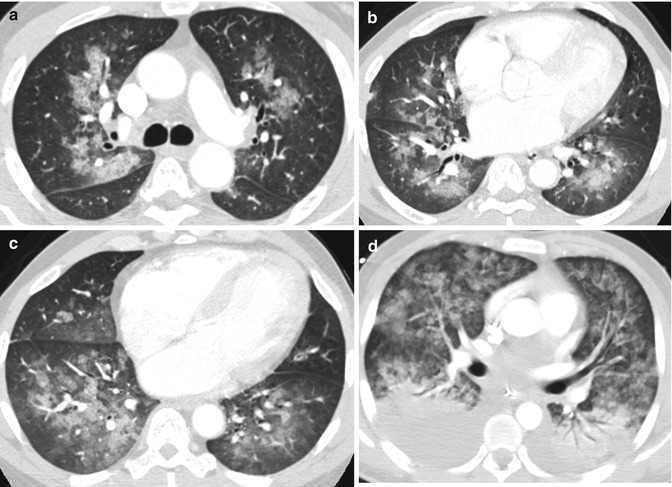
Fig. 8.46
Panlobular ground-glass opacities resulting from acute CHF with pulmonary edema in two patients. (a–c) Axial CT in a patient with mitral valve disease. (d) Axial CT in a patient with end-stage renal disease. There is also lobular consolidation of both lower lobes in this patient
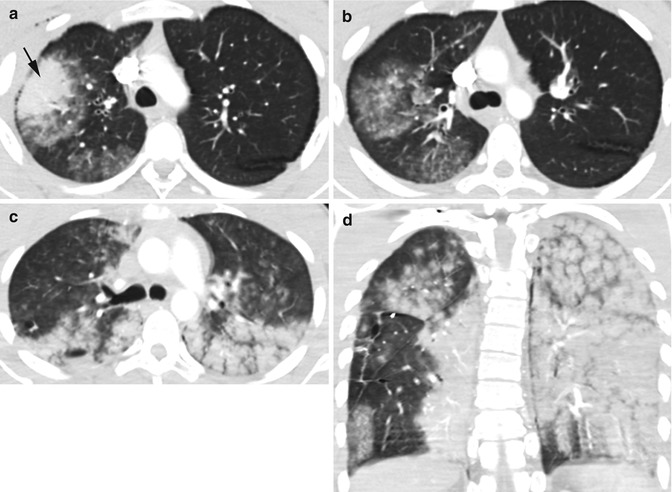
Fig. 8.47
Panlobular ground-glass opacity in pulmonary contusion from GSW in two patients. Patient 1: (a, b) Axial CT shows lobular consolidation (black arrow) with surrounding lobular ground-glass opacities in RUL. Patient 2: (b, c) Axial CT shows diffuse lobular ground-glass densities bilaterally
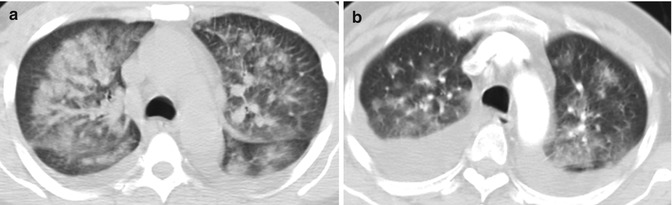
Fig. 8.48
Alveolar hemorrhage in two patients. Patient 1: (a) Hemorrhagic necrotizing pneumonia in a patient with acute renal failure with E. coli bacteremia and hemoptysis. Axial CT of the chest shows bilateral lobular ground-glass densities with small bilateral effusion. Patient 2: (b) Acute renal failure on anticoagulation and bronchoscopy confirmed alveolar hemorrhage. Axial CT of the chest shows bilateral lobular ground-glass densities and bilateral pleural effusion
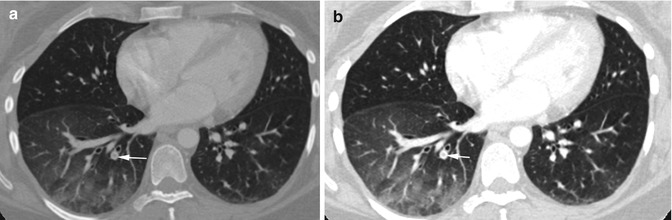
Fig. 8.49
Acute pulmonary infarction with lobular infarction with ground-glass density. (a, b) Axial CT of the chest shows thrombus in a right lower lobe branch of the pulmonary artery (arrow) with surrounding ground-glass lobular densities
Lobular Ground-Glass Opacity and Crazy Paving
Imaging Features
1.
Ground-glass opacity with superimposition of septal thickening
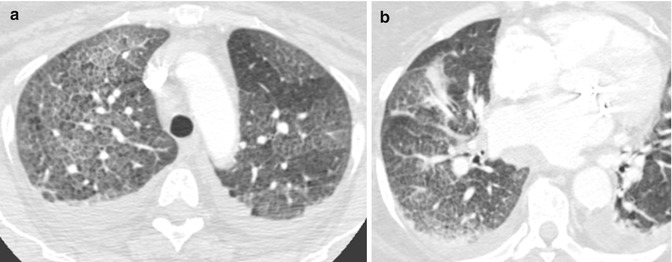
Fig. 8.50
CHF with cardiomegaly, pulmonary edema, and bilateral effusion. History of mitral and tricuspid valve repair and diastolic CHF. (a, b) Axial CT shows diffuse ground-glass density with increased reticular pattern especially in the right lung giving a crazy paving appearance
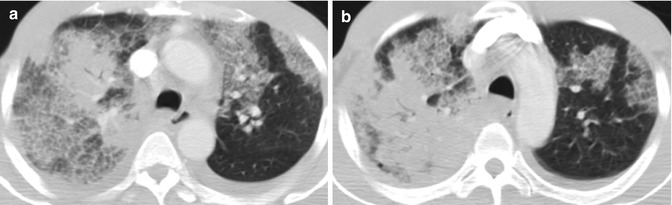
Fig. 8.51
Klebsiella pneumonia. (a, b) Axial CT of the chest shows lobular ground-glass opacities with crazy paving. There are also large areas of lobular consolidation in the right lung and bilateral small pleural effusion
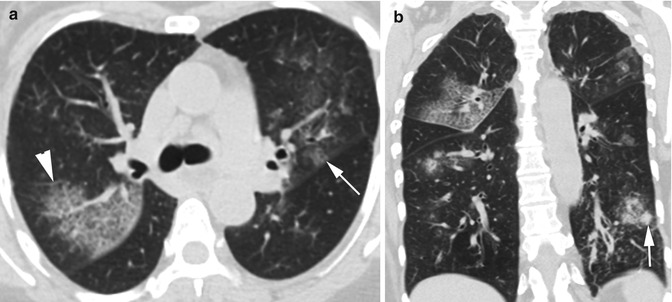
Fig. 8.52
Multilobar bronchopneumonia. (a, b) CT axial and coronal reformatted images show multiple lobular areas of ground-glass attenuation with crazy paving (arrowhead), smaller lobular ground-glass densities (thin arrow), and focal consolidation (thick arrow)
Fig. 8.53
Lung abscess. (a–c) Axial, coronal, and sagittal reformatted CTs show large lobular area of consolidation with central air-fluid collection of necrotic abscess. Reactive changes of the surrounding lung showing crazy paving. (d, e) Chest x-ray, PA, and lateral views showing same abscess (arrows)
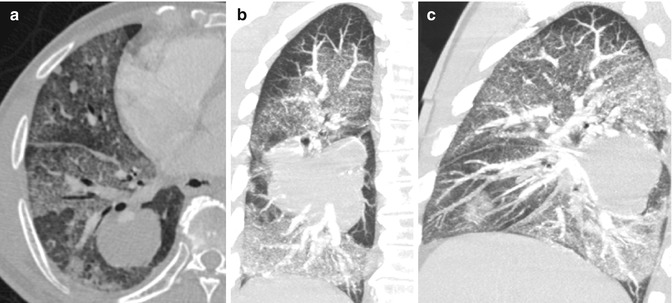
Fig. 8.54
Radiation pneumonitis with crazy paving surrounding stage IV adenocarcinoma. (a–c) Axial, coronal, and sagittal reformatted CTs show a large solid mass with surrounding diffuse panlobular ground-glass density with a crazy paving appearance