Differential diagnosis
Unilateral lesion
Adrenal adenomas (functional vs. nonfunctional)
Myelolipoma
Adrenal cyst
Metastases
Primary adenocarcinoma
Pheochromocytoma
Lymphoma
Neuroblastoma
Bilateral lesions
Hyperplasia
Hemorrhage
Infection (histoplasmosis or tuberculosis)
Metastases
Bilateral pheochromocytoma
Lymphoma
Indications and Patient Selection
Adrenal biopsy can be performed to establish a diagnosis in an indeterminate lesion, stage a known malignancy, or establish a diagnosis of malignancy in diffuse disease [14]. The indication for biopsy of an adrenal lesion is clear in patients with known extra-adrenal malignancies or suspected infection; however, not all adrenal masses warrant tissue sampling, and the role of percutaneous biopsy in the evaluation of adrenal “incidentalomas” is less certain.
An adrenal incidentaloma is defined as an adrenal mass, ≥1 cm in diameter, that has been incidentally discovered during a radiologic examination performed for purposes other than the evaluation of adrenal disease [10]. Most adrenal incidentalomas are benign, nonfunctioning adenomas; however, other common diagnoses include cortisol-secreting adenomas, pheochromocytomas, adrenal cortical carcinomas, and metastatic disease [15, 16]. According to the 2003 National Institutes of Health State-of-the-Science statement on adrenal incidentalomas, all patients with an adrenal incidentaloma require evaluation with a complete history and physical examination and hormonal testing [17]. It is recommended that all patients undergo a 1-mg overnight dexamethasone suppression test and measurement of fractionated urinary or plasma metanephrines and catecholamines. In hypertensive patients, additional evaluations of the serum potassium levels and plasma aldosterone concentration-plasma renin activity ratio are needed to assess for primary aldosteronism. If the biochemical test results are consistent with a functional adrenal cortical tumor or pheochromocytoma, surgical management is recommended [10, 17]. If the biochemical test results are normal, the radiologic images should be reviewed for lesion morphology, as larger lesions are associated with an increased risk for malignancy. An incidentaloma >4 cm in size is associated with an increased risk of malignancy of approximately 70 % and the risk increases to 85 % if the incidentaloma is >6 cm; conversely, nearly all lesions <4 cm are benign [10, 15, 17]. Given the increased risk of malignancy, surgical management is usually recommended for lesions ≥4 cm [10, 18]. For lesions <4 cm, yearly biochemical testing and repeat imaging at 6, 12, and 24 months following the initial scan are suggested [10, 17]. Percutaneous biopsy may be considered in patients with an incidentaloma and a history of malignancy; however, there are few studies demonstrating the utility of percutaneous biopsy in patients with an incidentaloma who do not have a history of malignancy [10, 17].
Contraindications
There are no absolute contraindications to adrenal gland biopsy. Relative contraindications include uncorrectable coagulopathy, an uncooperative patient, and lesion inaccessibility. Generally, biopsy of a suspected pheochromocytoma is not indicated as it can precipitate a potentially life-threatening hypertensive crisis.
Preprocedural Workup
Preparation for adrenal biopsy involves a review of the patient’s diagnostic imaging results, procedural indications, biochemical studies of adrenal function, and coagulation profile. Diagnostic images should be reviewed to confirm that biopsy is indicated, determine a trajectory for the biopsy needle, establish the modality for guidance, and anticipate patient positioning during the procedure. If positron emission tomography (PET) or PET/CT is available, the images may aid with targeting a specific area of the lesion that is fluoro-2-deoxy-d-glucose (FDG) positive to improve diagnostic yield.
It is essential to review all available biochemical studies, as they can affect the clinical management of adrenal masses: functional lesions do not require biopsy. Additionally, adrenal biopsy should not be performed until a pheochromocytoma has been excluded biochemically [19–21]. If biopsy of a suspected pheochromocytoma is categorically required, pre-biopsy consultation with an endocrinologist, who can provide for prophylactic blockade of the adrenergic receptors prior to the procedure, and anesthesiology support during the procedure, are strongly recommended.
Coagulation studies (platelet count, prothrombin time, international normalized ratio (INR), and partial thromboplastin time) should be examined and coagulopathies should be corrected prior to biopsy. In general, an INR ≤ 1.5 and a platelet count ≥50,000/L are acceptable parameters for solid organ biopsy. Written informed consent must be obtained before each procedure. Adrenal biopsy is well tolerated and can be performed either with local anesthesia alone or with monitored, conscious sedation using intravenous midazolam and fentanyl citrate. Preprocedural, prophylactic antibiotics are not routinely recommended.
Technique
Imaging
Ultrasound guidance can be used for very large adrenal lesions and provides the advantage of real-time monitoring of the needle during biopsy; however, CT is usually the imaging guidance modality of choice for adrenal biopsy. CT clearly delineates the anatomic detail of the adrenal gland and adjacent structures. It also demonstrates the position of the biopsy needle within the lesion and can be used to detect procedure-related complications, such as intra-abdominal hemorrhage or pneumothorax, quickly. Non-contrast-enhanced CT is usually adequate for procedure planning and execution. Axial images acquired in 3- or 5-mm thick slices are obtained to confirm the location of the lesion and to plan needle trajectory.
Devices
Small-caliber needles (20–22 gauge) provide fine-needle aspirates for cytologic assessment, and cutting needles (18–20 gauge) provide core biopsy samples for histologic analysis. Coaxial technique using a 16–19-gauge guide needle is often used during adrenal biopsy to allow for the acquisition of both fine-needle aspirates and core biopsies. Thin-wall Chiba needles, with a beveled tip, are common guide needles. A Hawkins needle, with interchangeable blunt and sharp stylets, may be useful when the needle path lies in close proximity to major vessels or when artificial paravertebral widening with saline injection is planned.
Approaches and Relevant Anatomy
The adrenal glands are located deep within the upper abdomen, surrounded by lung, liver, kidney, spleen, and pancreas (Fig. 16.1). The presence of these overlying structures can make adrenal gland biopsy technically challenging. Most image-guided adrenal biopsies are performed from a posterior approach. With the patient in the prone position, a direct, vertical approach to the adrenal gland is often not possible without transgressing the pleural space, which is associated with a risk of pneumothorax (Fig. 16.2). To avoid this potential complication, special techniques, such as angled approaches with or without CT gantry angulation, have been developed [22–24]. The triangulation method involves the construction of a right triangle and the use of the Pythagorean theorem and tangent ratios to calculate an extrapleural, extraperitoneal route to the lesion of interest with the patient in the prone position [23] (Fig. 16.3). The point on the skin directly overlying the lesion is marked (Z), and the depth from the skin surface to the center of the lesion is then calculated. This length (B) represents one side of the right triangle. A point on the skin surface, in the same parasagittal plane as point Z, is chosen for the needle entry site. The entry site should be below the posterior pleural reflection, either lower than the 12th rib or the transverse process of the first lumbar vertebra. The length (A) between the skin entry point and point Z represents the second side of the right triangle. The hypotenuse (C), representing the actual needle distance and an extrapleural, extraperitoneal path from the entry site to the center of the lesion, can now be calculated using the Pythagorean theorem for right triangles, (A2 + B2 = C2). The angle of needle insertion is determined from the tangent ratio of the two sides of the right triangle. Once the ratio is calculated, the angle can be extrapolated from a table of trigonometric ratios. It should be noted that with the angled approach, the entire needle length will not be visualized on a single transverse slice, and successive cephalad scans may be required to locate the needle tip (Fig. 16.4).
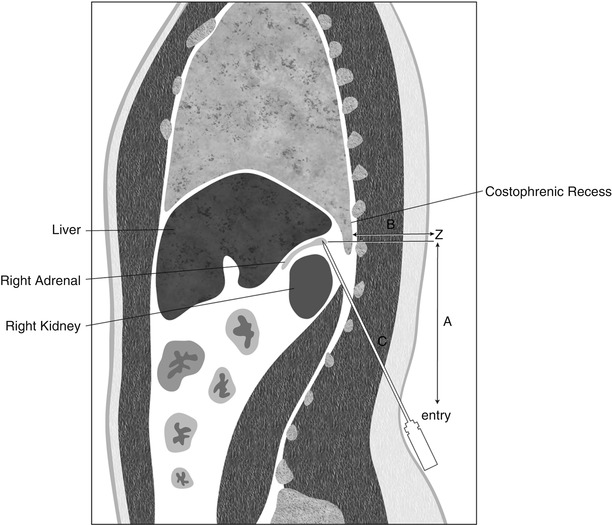
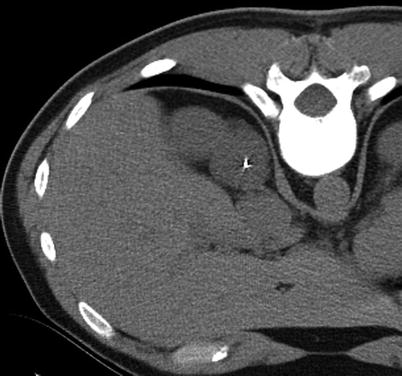
Fig. 16.1
Anatomy of the upper abdomen. Schematic representation of the adrenal glands lying within the upper abdominal cavity and their anatomic relationships to other surrounding solid organs
Fig. 16.3
Triangulation method. Schematic representation of use of the Pythagorean theorem and tangent ratios to calculate an extrapleural, extraperitoneal route to the adrenal gland in a patient in the prone position
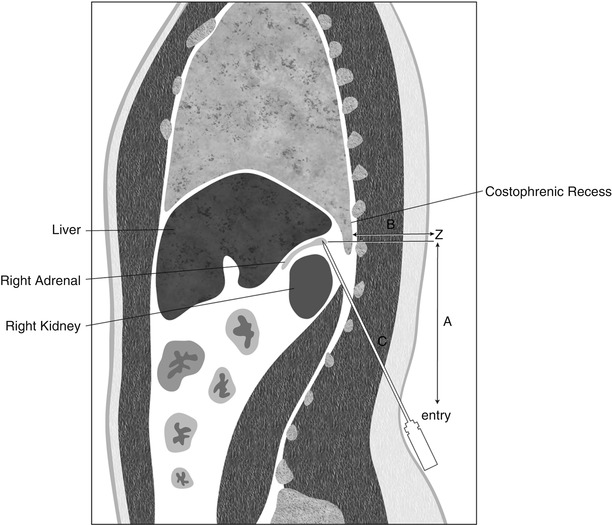
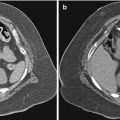
Fig. 16.2
Posterior approach for biopsy of adrenal gland. (a) Axial non-contrast-enhanced CT image demonstrates a direct, extrapleural, posterior approach to a left adrenal gland mass in a patient in the prone position. A coaxial biopsy technique was used where the 18-gauge Chiba guide needle has been positioned at the periphery of the left adrenal gland and a 22-gauge Chiba needle has been inserted coaxially into the left adrenal gland lesion. Both fine-needle aspiration and core biopsy were obtained and the pathologic diagnosis was metastatic non-small cell lung cancer. (b) Axial non-contrast-enhanced CT image shows a posterior approach, involving traversal of the pleural space, to a right adrenal gland lesion in a patient in the prone position. The pathologic diagnosis of metastatic colon cancer was made. Traversal of the pleural reflection resulted in a post biopsy pneumothorax as shown on the axial non-contrast-enhanced CT image in lung windows (c). The pneumothorax remained stable in size during the observation period and the patient was discharged home without a chest tube being placed
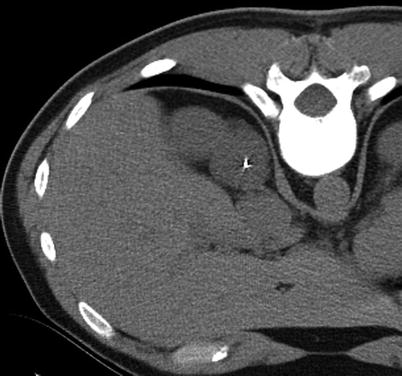
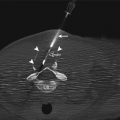
Fig. 16.4
CT-guided adrenal biopsy using triangulation method. The triangulation method was used to biopsy the right adrenal lesion, and an axial non-contrast-enhanced CT image demonstrates the tip of the biopsy needle within the adrenal lesion. The angled, subcostal approach avoids traversal of the pleural space by the biopsy needle; however, as is common with the angled approach, the entire needle length is not visualized on this single transverse image
Alternatively, with the patient in the prone position, angulation of the CT gantry towards the patient’s feet to create a caudocephalad beam direction can be used to avoid the posterior costophrenic sulcus during adrenal biopsy [22, 24]. With this technique, the biopsy needle is inserted along the plane of the angled CT gantry. Beam angulation then allows for visualization of a direct path to the adrenal lesion without having to perform geometric calculations. Another advantage of this technique is that the entire path of the needle can often be seen on a single transverse slice. Beam angulation between 15° and 25° has been shown to be sufficient for most adrenal lesions.
Other authors recommend a posterior approach to the adrenal gland while the patient is in an ipsilateral decubitus position, with the side of the gland of interest down [14, 25, 26]. In the decubitus position, the dependent diaphragm is elevated, removing the risk of costophrenic sulcus transgression, and allows for a more direct approach to the adrenal gland (Fig. 16.5).
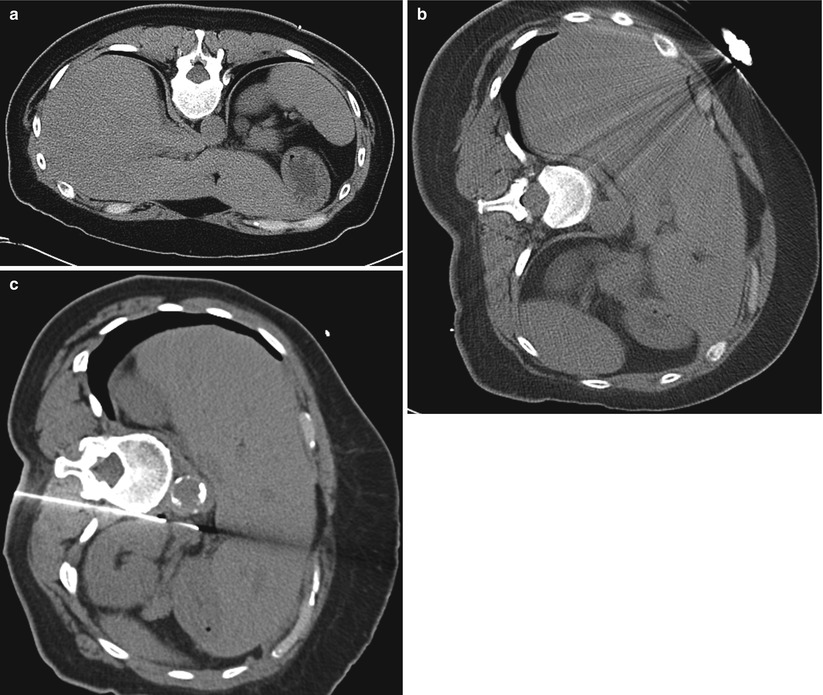
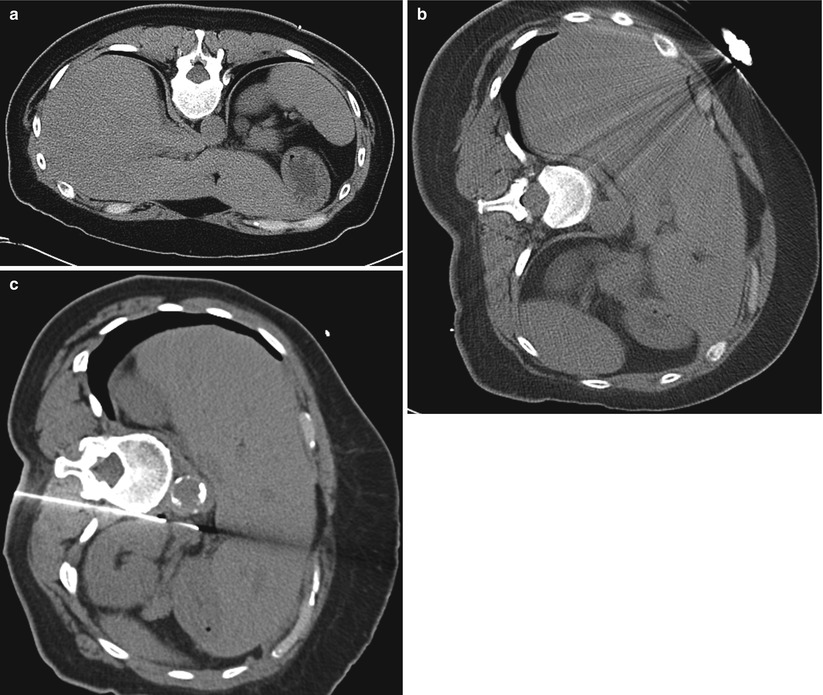
Fig. 16.5
Effects of position change on biopsy approach to adrenal gland. (a) A 39-year-old woman with lung cancer presented with a 1-cm left adrenal nodule. In the prone position, the left lower lobe of the lung is interposed between the skin and the left adrenal nodule. (b) Repositioning the patient into the ipsilateral decubitus position (left side down) elevates the dependent diaphragm, moves the lung out of the path of the biopsy needle, and provides a more direct approach to the adrenal lesion. (c) Axial non-contrast CT image depicts the coaxial technique using an 18-gauge Hawkins guide needle and a 22-gauge Chiba needle for biopsy of a different patient with a left adrenal lesion in the ipsilateral decubitus position
Besides the presence of interposed lung, access to the adrenal gland in the prone position may be hampered by the kidney or vertebral body (Fig. 16.6). Artificial widening of the paravertebral space using the injection of saline is a well-known technique in the biopsy of mediastinal lesions; this technique can also be applied to the biopsy of the adrenal gland [27]. Injecting saline into the posterior paravertebral space results in lateral displacement of the parietal pleura, providing an extrapleural path to the adrenal lesion (Figs. 16.7 and 16.8). When no alternative access to the adrenal gland is available, transrenal adrenal biopsy can be performed [25] (Fig. 16.9).

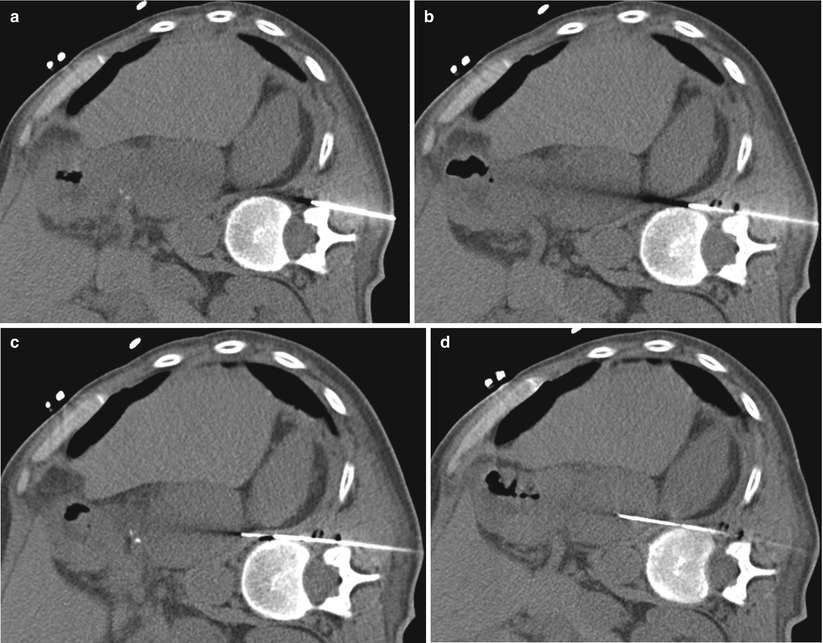
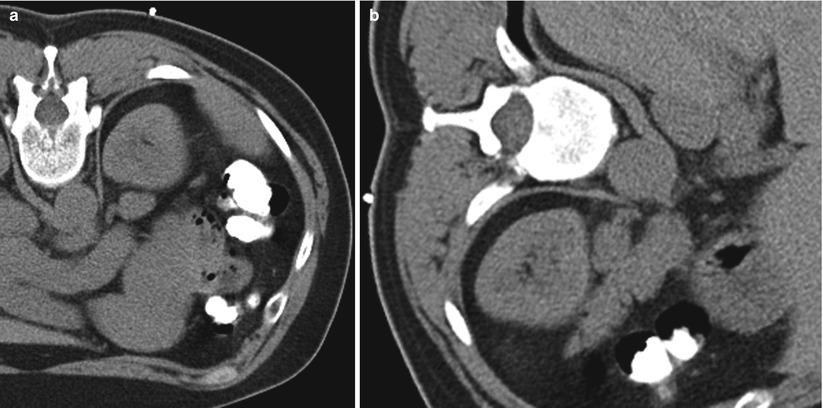
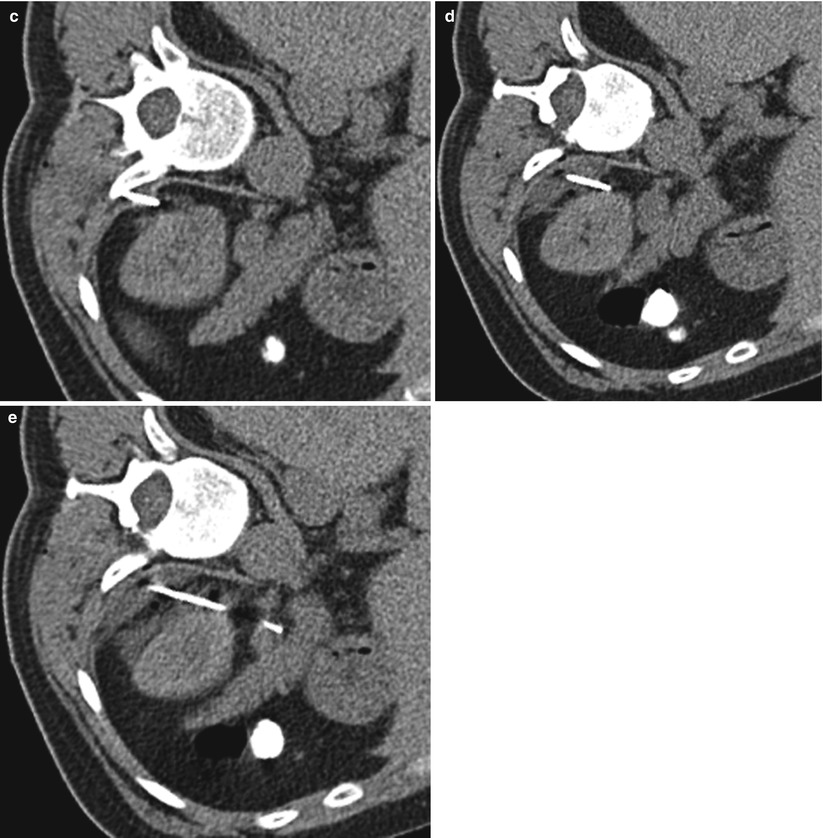

Fig. 16.6
Ipsilateral decubitus approach for biopsy of adrenal gland. Axial non-contrast-enhanced CT image demonstrates an extrapleural, paravertebral approach to a left adrenal gland lesion with the patient in the ipsilateral decubitus position. Note the slight curvature on the 22-gauge Chiba needle within the adrenal lesion. Putting a small curve on the 22-gauge biopsy needle can help to redirect the needle into the lesion. The pathologic diagnosis was metastatic renal cell carcinoma
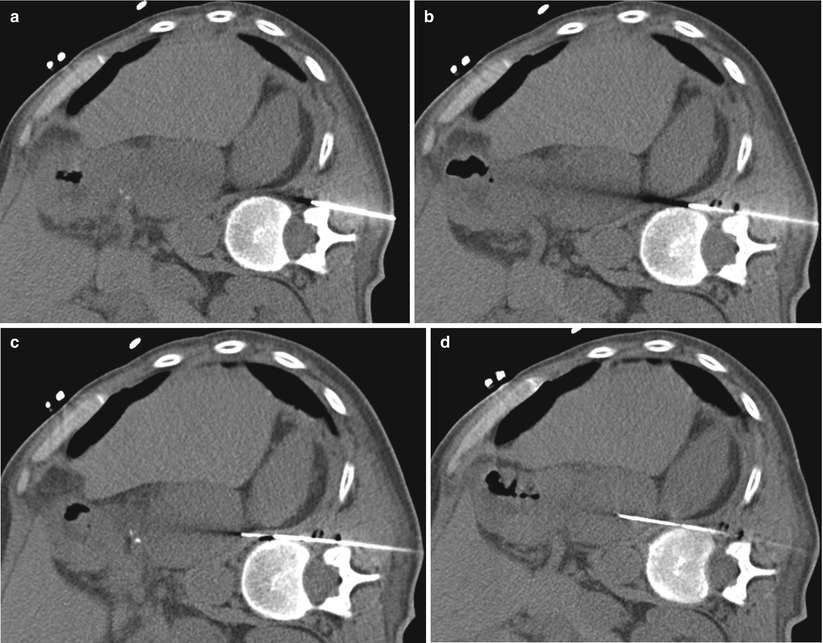
Fig. 16.7
Injection of saline to create an extrapleural approach for biopsy of adrenal gland. Saline can be injected to widen the paravertebral space to create a larger space for the needle to pass. The injected saline will also displace the parietal pleural laterally, thus decreasing the risk of pleural transgression (a, b, c, d). This patient was placed in the contralateral decubitus position because of the significant beam-hardening artifact from residual contrast in the colon (not shown). The pathologic diagnosis was metastatic non-small cell carcinoma
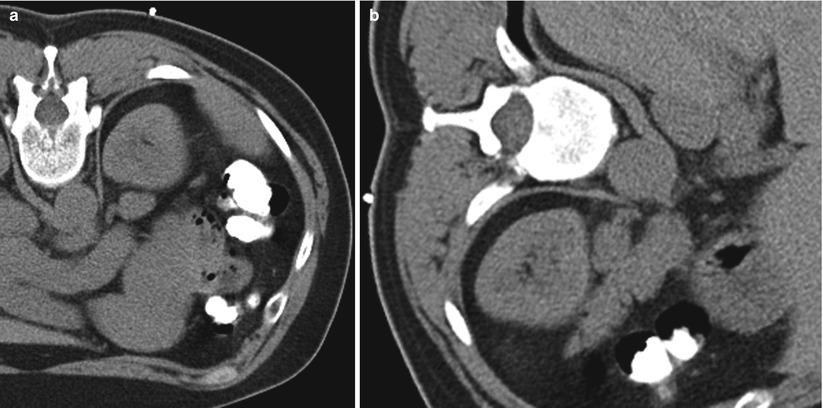
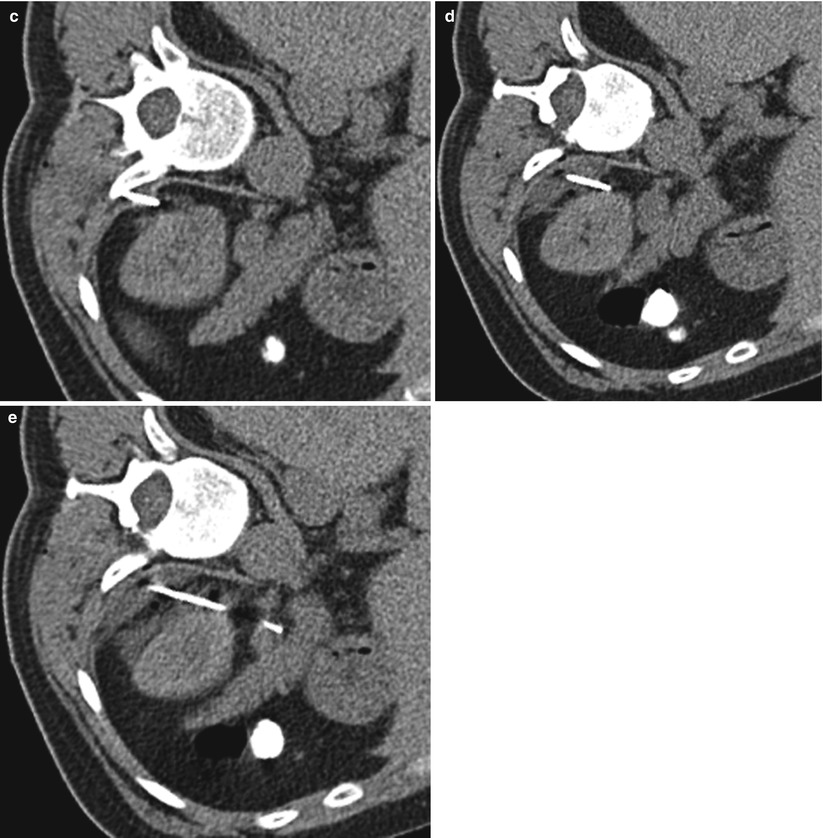
Fig. 16.8




Injection of saline to displace kidney during biopsy of adrenal gland. (a) A 43-year-old woman with squamous cell carcinoma of the right tonsil presented with a left adrenal mass. Axial non-contrast-enhanced CT image with the patient in the prone position demonstrates the left kidney directly overlying the left adrenal gland without a clear approach to the adrenal gland for the biopsy needle. (b) Repositioning the patient in the ipsilateral decubitus position was not particularly helpful as the left kidney still prevented direct access to the left adrenal gland. (c) The injection of saline during needle placement provided adequate displacement of the kidney laterally and to allow for left adrenal gland biopsy without traversing the left kidney (c, d, e). The low-density posterior and medial to the left kidney represents the injected saline. The pathologic diagnosis in this case was an adrenal cortical adenoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree