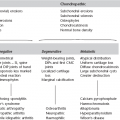
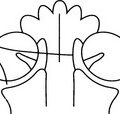
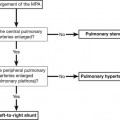
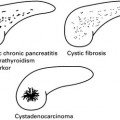
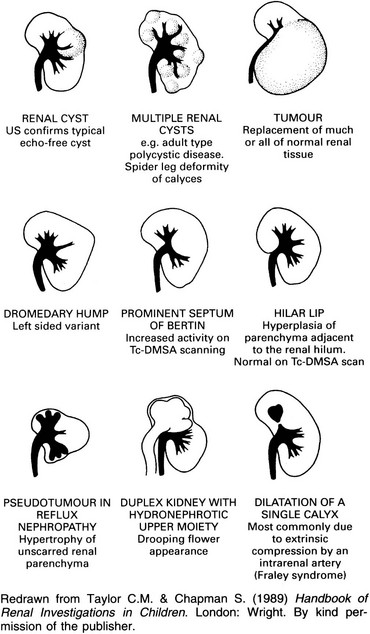
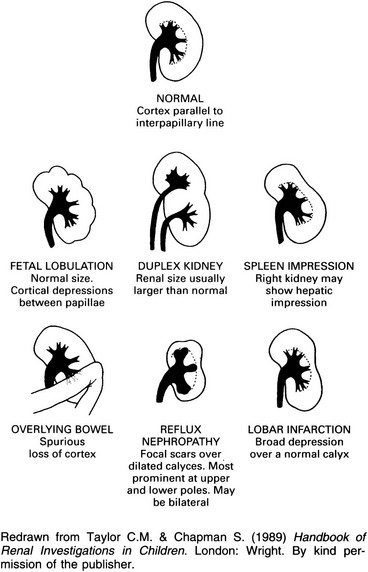
8 8.1 Adrenal calcification 1. Cystic disease – similar to that seen in the child. Blunt abdominal trauma is a much more common cause in adults. Bilateral in 15% of cases. 2. Carcinoma – irregular punctate calcifications seen in 30%. Average size of tumour is 14 cm and there is frequently displacement of the ipsilateral kidney. 3. Addison’s disease – now most commonly due to autoimmune disease or metastasis. Historically, when TB was a frequent cause, calcification was a common finding. 4. Ganglioneuroma – 40% occur over the age of 20 years. Slightly flocculent calcifications in a mass, which is usually asymptomatic. Large tumours may cause displacement of the adjacent kidney and/or ureter. 5. Inflammatory – primary tuberculosis and histoplasmosis. 6. Phaeochromocytoma – calcification is rare but when present is usually an ‘egg-shell’ pattern. 8.2 Incidental adrenal mass (unilateral) 1. Conn’s adenoma – accounts for 70% of Conn’s syndrome. Usually small, 0.5–1.5 cm. Homogeneous, relatively low density due to build-up of cholesterol. 30% of Conn’s syndrome due to hyperplasia, which can occasionally be nodular and mimic an adenoma. 2. Phaeochromocytoma – usually large, > 5 cm, with marked contrast enhancement (beware hypertensive crisis with i.v. contrast medium). 10% malignant, 10% bilateral, 10% ectopic (of these 50% are located around the kidney, particularly the renal hilum. If CT does not detect, MIBG isotope scan may be helpful). 10% are multiple and usually part of MEN II syndrome, neurofibromatosis or von Hippel–Lindau. 3. Cushing’s adenoma – accounts for 10% of Cushing’s syndrome. Usually > 2 cm in diameter. 40% show slight reduction in density. 80% of Cushing’s syndrome due to excess ACTH from pituitary tumour or ectopic source (small cell carcinoma, pancreatic islet cell, carcinoid, medullary carcinoma of thyroid, thymoma) which causes adrenal hyperplasia not visible on CT scan. 10% of Cushing’s syndrome due to adrenal carcinoma. The possibilities for adrenal mass in Cushing’s syndrome are: (a) Functioning adenoma/carcinoma. (b) Coincidental non-functioning adenoma. (c) Metastasis from small cell primary. (d) Nodular hyperplasia, which occurs in 20% of Cushing’s syndrome due to pituitary adenoma. 4. Adrenal carcinoma – 50% present as functioning tumours (Cushing’s 35%, Cushing’s with virilization 20%, virilization 20%, feminization 5%). 1. Metastases – may be bilateral, usually > 2–3 cm, irregular outline with patchy contrast enhancement. Recent haemorrhage into a vascular metastasis (e.g. melanoma) can give a patchy high density on precontrast scan. In patients without a known extra-adrenal primary tumour the vast majority of adrenal masses are benign; even in the presence of a known primary malignant tumour many adrenal masses will still be benign (40% are metastases). 2. Carcinoma – typical features are: 3. Lymphoma – 25% also involve kidneys at autopsy. Lymphadenopathy will be seen elsewhere. 4. Neuroblastoma – > 5 cm. Calcification in 90%. Extends across midline. Nodes commonly surround and displace the aorta and inferior vena cava. 1. Non-functioning adenoma – occurs in 5% at autopsy. Usually relatively small (50% < 2 cm), homogeneous and well-defined. 2. Myelolipoma – 0.2% at autopsy. Rare benign tumour composed of adipose and haemopoietic tissue. 85% are found in the adrenal but extra-adrenal tumours (liver, retroperitoneum, pelvis) have been reported. Low attenuation on CT and may enhance. Mean diameter of 10 cm. 3. Angiomyolipoma – adrenal lesions are very rare in practice. Usually contain vascular tissue and fat density. 4. Cyst – well-defined, water density. 5. Post-traumatic haemorrhage – homogeneous, hyperdense. Occurs in 25% of severe trauma, 20% bilateral, 85% on right. Adrenal haemorrhage can also occur in vascular metastases, anticoagulant treatment and severe stress (e.g. surgery, sepsis, burns, hypotension). 6. Granulomatous disease (TB, histoplasmosis) – present as diffuse enlargement or as discrete mass. Can have a central cystic component, with/without calcification. Boland, G. W., Blake, M. A., Hahn, P. F., Mayo-Smith, W. W. Incidental adrenal lesions: principles, techniques, and algorithms for imaging characterization. Radiology. 2008; 249(3):756–775. Boland, G. W., Dwamena, B. A., Jagtiani Sangwaiya, M., et al. Characterization of adrenal masses by using FDG PET: a systematic review and meta-analysis of diagnostic test performance. Radiology. 2011; 259(1):117–126. Low, G., Dhliwayo, H., Lomas, D. J. Adrenal neoplasms. Clin Radiol. 2012; 67:988–1000. Park, B. K., Kim, C. K., Lee, J. H. Comparison of delayed enhanced CT and chemical shift MR for evaluating hyperattenuating incidental adrenal masses. Radiology. 2007; 243(3):760–765. 8.3 Bilateral adrenal masses 1. Metastases – bilateral in 15%. Common at autopsy. Most common primary sites are lung or breast; also melanoma, renal cell carcinoma, gastrointestinal tract, thyroid, contralateral adrenal gland. Usually does not affect adrenal function; may cause adrenal insufficiency if extensive (replacing > 80% of adrenal gland). 2. Phaeochromocytoma – bilateral in 10%. 3. Hyperplasia – adrenogenital syndromes result in symmetrically enlarged and thickened adrenal glands. Adrenocortical hyperplasia can cause bilateral adrenal enlargement but usually these are not visible on CT. 4. Spontaneous adrenal haemorrhage. 5. Lymphoma – primary adrenal lymphoma is rare. Usually presents with bilateral adrenal masses, often with adrenal hypofunction. Usually diffuse large B-cell lymphomas. Adrenal involvement occurs at autopsy in up to 25% with disseminated lymphoma, usually with no associated adrenal insufficiency. 6. Granulomatous disease – histoplasmosis/TB. Can be acute or chronic. Patients with adrenal masses and adrenal failure caused by chronic disseminated histoplasmosis may have symptoms and CT findings that are indistinguishable from those of malignancy. 8.4 Adrenal pseudotumours 1. Exophytic upper pole renal mass – requires sagittal or coronal reconstructions and thin-section CT. 2. Gastric diverticulum – give oral contrast. 3. Splenic lobation/accessory spleen – give intravenous contrast, should enhance to the same level as the body of the spleen. 4. Prominent lobation of the hepatic lobe, or hepatic tumour. 5. Varices – give intravenous contrast. 6. Large mass in tail of pancreas – give intravenous contrast, pancreatic mass usually displaces splenic vein posteriorly, whereas adrenal mass displaces it anteriorly. 7. Fluid-filled colon – give intraluminal contrast and thin-section CT. Intraluminal gas is diagnostic. 8.5 Mibg imaging The scintigraphic distribution of 131I MIBG occurs in organs with adrenergic innervation or those that process catecholamines for excretion. 8.6 Congenital renal anomalies These may be anomalies of position, of form or of number. 1. Pelvic kidney – ectopic kidney due to failure of renal ascent. There is non-rotation with anteriorly positioned renal pelvis in most cases. Blood supply is from the iliac artery or the aorta. Most ectopic kidneys are asymptomatic, notwithstanding the fact that pelvic kidneys are more susceptible to trauma and infection and may complicate natural childbirth later in life. 2. Ectopic kidney – in the case of intrathoracic kidney, usually an acquired duplication through the foramen of Bochdalek. Can also be presacral or at the lower lumbar level. 1. Horseshoe kidney – two kidneys joined by parenchymal/fibrous isthmus. Most common fusion anomaly with incidence of 1 in 400 births. Fusion of right and left kidneys at lower pole in 90%. Abnormal axis of each kidney (bilateral malrotation). Renal pelves and ureters situated anteriorly and renal long axis medially oriented. Associated with other anomalies in 50% (e.g. vesicoureteral reflux, ureteral duplication, genital anomalies, Turner’s syndrome). 2. Pancake/discoid kidney – bilateral fused pelvic kidneys, usually near the aortic bifurcation. 3. Crossed renal ectopia – kidney is located on opposite side of midline from its ureteral orifice. Usually L > R. The lower kidney is usually ectopic. In 90% there is fusion of both kidneys (= crossed fused ectopia). May be associated with anorectal anomalies and renal dysplasia. Slightly increased incidence of calculi. 4. Renal hypoplasia – incomplete development results in a smaller (< 50% of normal size) kidney with fewer calyces and papillae. Normal function. 1. Unilateral renal agenesis – 1 : 1000 live births. Increased incidence of extrarenal abnormalities (meningomyelocoele, ventricular septal defect, intestinal tract strictures, imperforate anus, unicornuate uterus skeletal abnormalities). Hyperplastic normal solitary kidney – up to twice normal size. 2. Bilateral renal agenesis – Potter syndrome. 1 : 10,000 live births. Invariably fatal in first few days of life due to pulmonary hypoplasia secondary to the associated oligohydramnios. 3. Supernumerary kidney – very rare. Most commonly on left side caudal to normal kidney. Cohen, H. L., Kravets, F., Zucconi, W., et al. Congenital abnormalities of the genitourinary system. Semin Roentgenol. 2004; 39(2):282–303. Philip, J., Kenney, P. J., Spirt, B. A., et al. Genitourinary anomalies: radiologic–anatomic correlations. Radiographics. 1984; 4:233–260. Servaes, S., Epelman, M. The current current state of imaging pediatric genitourinary anomalies and abnormalities. Curr Probl Diagn Radiol. 2013; 42(1):1–12. 8.7 Localized bulge of the renal outline 1. Cyst – well-defined nephrographic defect with a thin wall on the outer margin. Beak sign. Displacement and distortion of smooth-walled calyces without obliteration. 2. Tumour – mostly renal cell carcinoma in adults and Wilms’ tumour in children. See 8.21. 3. Fetal lobation – the lobule directly overlies a normal calyx. Normal interpapillary line. See 8.8. 4. Dromedary hump – on the midportion of the lateral border of the left kidney. Occurs secondary to prolonged pressure by spleen during fetal development. The arc of the interpapillary line parallels the renal contour. 5. Splenic impression – on the left side only. This produces an apparent bulge inferiorly. 6. Enlarged septum of Bertin – overgrowth of renal cortex from two adjacent renal lobules. Usually between upper and interpolar portion. Excretory urography shows a pseudomass with calyceal splaying and associated short calyx ± attempted duplication. Tc-DMSA accumulates normally or in excess. On US echogenicity is usually similar to normal renal cortex but may be of increased echogenicity. CT – enhances similar to cortex. 7. Localized compensatory hypertrophy – e.g. adjacent to an area of pyelonephritic scarring. 8. Acute focal nephritis (lobar nephronia) – usually an ill-defined hypoechoic mass on US, but may be hyperechoic. CT shows an ill-defined, low-attenuation, wedge-shaped mass with reduced contrast enhancement. 9. Abscess – loss of renal outline and psoas margin on the control film. Scoliosis concave to the involved side. Initially there is no nephrographic defect, but following central necrosis there will be a central defect surrounded by a thick irregular wall. Adjacent calyces are displaced or effaced. 10. Non-functioning moiety of a duplex – usually a hydronephrotic upper moiety. Delayed films may show contrast medium in the upper moiety calyces. Lower moiety calyces display the ‘drooping lily’ appearance. Bhatt, S., MacLennan, G., Dogra, V. Renal pseudotumors. AJR Am J Roentgenol. 2007; 188(5):1380–1387. O’Connor, S. D., Pickhardt, P. J., Kim, D. H., et al. Incidental finding of renal masses at unenhanced CT: prevalence and analysis of features for guiding management. AJR Am J Roentgenol. 2011; 197(1):139–145. Silverman, S. G., Israel, G. M., Herts, B. R., Richie, J. P. Management of the incidental renal mass. Radiology. 2008; 249(1):16–31. 8.8 Unilateral scarred kidney 1. Reflux nephropathy – a focal scar over a dilated calyx. Usually multifocal and may be bilateral. Scarring is most prominent in the upper and lower poles. Minimal scarring, especially at a pole, may produce decreased cortical thickness with a normal papilla and is then indistinguishable from lobar infarction. 2. Tuberculosis – calcification differentiates it from the other members of this section. 3. Lobar infarction – a broad contour depression over a normal calyx. Normal interpapillary line. 4. Renal dysplasia – a forme fruste multicystic kidney. Dilated calyces. Indistinguishable from chronic pyelonephritis. Arteriography outlines a small threadlike renal artery. 8.9 Unilateral small smooth kidney 1. Ischaemia due to renal artery stenosis – ureteric notching is due to enlarged collateral vessels and differentiates this from the other causes in this group. See 8.28. 2. Radiation nephritis – at least 23 Gy over 5 weeks. The collecting system may be normal or small. Depending on the size of the radiation field, both, one or just part of one kidney may be affected. There may be other sequelae of radiotherapy, e.g. scoliosis following radiotherapy in childhood. 3. End result of renal infarction – due to previous severe trauma involving the renal artery or renal vein thrombosis. The collecting system does not usually opacify during excretion urography. 8.10 Bilateral small smooth kidneys Chronic papillary necrosis (see 8.26) – with other signs of necrotic papillae. 8.11 Unilateral large smooth kidney 1. Autosomal dominant polycystic kidney disease* – asymmetrical bilateral enlargement, but 8% of cases are unilateral. Lobulated rather than completely smooth. 2. Duplex kidney – F : M = 2 : 1. Equal incidence on both sides and 20% are bilateral. Incomplete more common than complete. Only 50% are bigger than the contralateral kidney; 40% are the same size; 10% are smaller. 3. Crossed fused ectopia – see 8.6. 5. Acute pyelonephritis – impaired excretion of contrast medium ± dense nephrogram. Attenuated calyces but may have non-obstructive pelvicalyceal or ureteric dilatation. Completely reversible within a few weeks of clinical recovery. 6. Trauma – haematoma or urinoma. Davidson, A. J. Renal parenchymal disease. In: Davidson A. J., Hartman D. S., Choyke P. L., Wagner B. J., eds. Radiology of the kidney and genitourinary tract. third ed. Philadelphia, PA: WB Saunders; 1999:73–358. Pickhardt, P. J., Lonergan, G. J., Davis, C. J., Jr., et al. Infiltrative renal lesions: radiologic–pathologic correlation. Radiographics. 2000; 20:215–243. 8.12 Bilateral large smooth kidneys It is often difficult to distinguish, radiologically, the members of this group from one another. The appearance of the nephrogram may be helpful – see 8.25. Associated clinical and radiological abnormalities elsewhere are often more useful, e.g. in sickle-cell anaemia, Goodpasture’s disease and acromegaly. 1. Acute renal papillary necrosis (see 8.26). 5. Acromegaly* and gigantism – as part of the generalized visceromegaly. 8.13 Renal calcification Usually one kidney or part of one kidney. (a) Tuberculosis – variable appearance of nodular, curvilinear or amorphous calcification. Typically multifocal with calcification elsewhere in the urinary tract. (b) Hydatid – the cyst is usually polar and calcification is curvilinear or heterogeneous. 50% of echinococcal cysts calcify. (c) Xanthogranulomatous pyelonephritis – large obstructive calculus in 80% of cases. (d) Abscess – tuberculous abscess frequently calcifies. Pyogenic abscesses rarely calcify. (a) Carcinoma – in 6% of carcinomas. Usually amorphous or irregular, but occasionally curvilinear. (c) Urothelial carcinoma – very rare. 3. Cysts – usually related to previous infection or haemorrhage. 8.14 Renal calculi Uric acid, xanthine, matrix (mucoprotein) and stones related to treatment with indinavir. 1. With normocalcaemia – obstruction, urinary tract infection, prolonged bed rest, ‘horseshoe’ kidney, vesical diverticulum, renal tubular acidosis, medullary sponge kidney and idiopathic hypercalciuria. 2. With hypercalcaemia – hyperparathyroidism, milk-alkali syndrome, excess vitamin D, idiopathic hypercalcaemia of infancy and sarcoidosis. 1. Primary hyperoxaluria – rare. AR. 65% present below 5 years of age. Radiologically – nephrocalcinosis (generally diffuse and homogeneous but may be patchy), recurrent nephrolithiasis, dense vascular calcification, osteopenia or renal osteodystrophy and abnormal metaphyses (dense and/or lucent bands). 2. Enteric hyperoxaluria – due to a disturbance of bile acid metabolism. Mainly in patients with small bowel disease, either Crohn’s disease or surgical resection. Blake, S. P., McNicholas, M. M., Raptopoulos, V. Nonopaque crystal deposition causing ureteric obstruction in patients with HIV undergoing indinavir therapy. AJR Am J Roentgenol. 1999; 171(3):717–720. Dyer, R. B., Chen, M. Y., Zagoria, R. J. Abnormal calcifications in the urinary tract. Radiographics. 1998; 18(6):1405–1424. Sandhu, C., Anson, K. M., Patel, U. Urinary tract stones – Part I: role of radiological imaging in diagnosis and treatment planning. Clin Radiol. 2003; 58(6):415–421. Sandhu, C., Anson, K. M., Patel, U. Urinary tract stones – Part II: current state of treatment. Clin Radiol. 2003; 58(6):422–423. 8.15 Signs of urinary tract stone disease on CT 1. Calcification within the renal collecting system or ureteric lumen. 3. Asymmetric inflammatory change of the perinephric fat. 6. Soft tissue rim sign – refers to a soft tissue ring surrounding the calcification, representing the oedematous wall of the surrounding ureter, and may be helpful in differentiating a phlebolith from a ureteric stone. 8.16 Mimics of renal colic on unenhanced CT urography 1. Pyelonephritis – asymmetric perinephric stranding or mild renal enlargement. Mild disease may have no signs on unenhanced CT. Following intravenous contrast administration, pyelonephritis may be seen as a focal wedge-shaped region of low attenuation or a more widespread striated enhancement of the kidney. Renal or perinephric abscesses are rare sequelae. 2. Congenital pelviureteric obstruction. 3. Ureteric obstruction secondary to abdominal and pelvic lymphadenopathy. 1. Appendicitis – the normal appendix is usually less than 6 mm wide, thin walled, and may contain an appendicolith. Gas in the lumen may be both a normal and abnormal finding. Look for dilatation of the appendix to more than 6 mm, inflammatory stranding of the periappendiceal or pericaecal fat, and surrounding phlegmon or abscess. A faecalith within a fluid collection in the right lower quadrant is very helpful for making the diagnosis of a perforated appendicitis. 2. Diverticulitis – characteristic findings include inflammation of pericolic fat related to diverticula, focal colonic wall thickening, thickening of adjacent fascia, thickening of the root of the mesentery and intra-abdominal abscess. Most inflamed diverticula are usually within the sigmoid or descending colon. 3. Small bowel diverticulitis and Meckel diverticulitis may mimic renal colic. 8. Inflammatory bowel disease. 9. Pancreatic and hepatobiliary disorders 1. Renal infarction – unilateral perinephric stranding is suggestive of a dissection flap into the renal artery. 4. Ruptured abdominal aortic aneurysm – crescent-shaped area of high attenuation, higher than intraluminal blood, in the wall of an abdominal aortic aneurysm. Periaortic stranding or haemorrhage, > 60 HU is indicative of active bleeding. 5. Aortic dissection – high attenuation on unenhanced CT in the wall of the aorta indicates intraluminal haematoma, displacement of intimal calcification into the aortic lumen; renal infarction. 6. Isolated SMA dissection – rare; signs include perivascular fat stranding, vessel enlargement, irregular contour and displacement of intimal calcification. Secondary signs of bowel compromise are bowel wall thickening, pneumatosis and bowel distension. 7. SMA thrombosis or embolism – may present with pain radiating to one side; the signs are an enlarged vessel, perivascular stranding and high-attenuation material within the vessel caused by clotted blood. 8. Intraperitoneal and retroperitoneal haemorrhage – trauma-related, spontaneous haemorrhage is usually related to use of anticoagulants, also in bleeding diatheses, vasculitis (polyarteritis nodosa), splenic rupture and certain neoplasms.
Adrenals, urinary tract and testes
Functioning tumours
Malignant tumours
Benign
Imaging structures mimicking adrenal mass
Anomalies of position
Anomalies of form
Anomalies of number
Prerenal = vascular
Postrenal = collecting system
Renal = parenchymal
Miscellaneous
Dystrophic calcification due to localized disease
Non-opaque
Calcium-containing
Pure calcium oxalate due to hyperoxaluria
Non-stone genitourinary
Gastrointestinal
Vascular