This article presents an overview of advanced magnetic resonance (MR) imaging techniques using contrast media in neuroimaging, focusing on T2*-weighted dynamic susceptibility contrast MR imaging and T1-weighted dynamic contrast-enhanced MR imaging. Image acquisition and data processing methods and their clinical application in brain tumors, stroke, dementia, and multiple sclerosis are discussed.
- •
Studying brain perfusion and permeability is possible without an additional dose of gadolinium-based contrast agent.
- •
Dynamic susceptibility contrast magnetic resonance (MR) imaging) using T2- or T2*-weighted imaging is the most commonly used MR perfusion technique of the brain.
- •
Dynamic relaxivity contrast-enhanced MR imaging using T1-weighted relaxivity imaging is the most commonly used MR permeability technique.
- •
Dynamic susceptibility contrast and dynamic relaxivity contrast-enhanced MR imaging can provide clinically useful physiologic information to complement conventional contrast-enhanced MR imaging, particularly of brain tumors and stroke.
Introduction
Contrast agent injection is essential to characterize abnormalities in neuroimaging (see the articles by Guttierrez and colleagues, Kim and colleagues elsewhere in this issue for further exploration of this topic). However, contrast enhancement is nonspecific reflection of blood-brain barrier (BBB) disruption. The injection of gadolinium-based contrast agents (GBCAs) allows characterization of the brain’s hemodynamic processes (ie, brain perfusion) and the BBB leakage-permeability. It is now recognized that advance MR imaging techniques, such as those used to study perfusion and permeability, provide physiologic instead of simply the morphologic data obtained with conventional magnetic resonance (MR) imaging.
Dynamic contrast imaging can be separated into 2 main categories according to the contrast agent properties: the dynamic susceptibility contrast (DSC) MR imaging using T2- or T2*-weighted imaging and the dynamic relaxivity contrast-enhanced (DCE) MR imaging) using T1-weighted relaxivity imaging. Both perfusion and permeability measurements could be extracted from these 2 technique categories, but DSC-MR imaging is commonly referred to as “perfusion” imaging and DCE-MR imaging is commonly referred to as “permeability” imaging.
DSC-MR imaging is the most used technique in clinical imaging of brain tumor and stroke. This technique can provide hemodynamic metrics such as cerebral blood flow (CBF), cerebral blood volume (CBV), and mean transit time (MTT). Compared with DSC-MR imaging, DCE-MR imaging has less widespread use, likely owing to more stringent acquisition and complex requirements to explore BBB permeability.
The aim of this review is to give an overview of the basic principles and common neuroimaging applications of these 2 advanced techniques using contrast media.
Imaging technique
Perfusion: DSC-MR Imaging
Principle
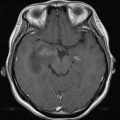
DSC-MR imaging, also known as perfusion-weighted MR imaging, MR perfusion, or bolus-tracking MR imaging, is a technique to track the first-pass of an exogenous, paramagnetic, nondiffusible contrast agent, typically a GBCA through the tissue. Since it was first described by Villringer and colleagues in 1988, DSC-MR imaging has emerged as a dominant method to study the brain microvascular component. To record the signal loss caused by susceptibility effects during the first passage of a GBCA through the tissue of interest, T2- or T2*-weighted images should be dynamically acquired at a rate faster than the time it takes the bolus to pass through the tissue. With the application of tracer kinetic models for intravascular tracers and the use of the central volume theorem, the major perfusion parameters CBV, CBF, and MTT can be estimated ( Fig. 1 ).
Images acquisition
A single-shot echo planar imaging (EPI) is generally used because it provides a means for very rapid image acquisition. EPI is generally performed in conjunction with multislice gradient-echo (GRE) or spin-echo (SE)-EPI techniques. GRE-EPI methods (T2*-weighted images) are able to provide better spatial coverage of the brain, are sensitive to both large and small vessels with better signal-to-noise ratio, and require half the dose of a GBCA compared with multislice SE (T2-weighted images). Compared with GRE, SE techniques seem to be more sensitive to smaller vessels (capillaries) and have less image distortion and artifacts at the brain–bone interface. Despite these advantages, studies have shown that GRE sequences are superior in their ability to predict glioma grade compared with SE sequences. Even if combinations of the 2 techniques have been reported, the GRE-EPI method is the most widely used technique. Both 2-dimensional (2D) EPI and 3-dimensional sequences are used; however, 2D sequences are usually preferably compared because of their ability to achieve better spatial resolution and shorter repetition times (TR) and provide a more accurate characterization of bolus passage. The typical acquisition time for the first-pass T2* DSC-MR imaging acquisition is on the order of 90 seconds. A temporal resolution on the order of 1 to 2 seconds is desired to obtain the correct shape of the concentration–time curve. The recommended matrix resolution is 128 × 128. Slice thickness could range between 2 and 5 mm depending on the need for whole brain volume coverage. A combination of a phase-array coil and parallel imaging, in particular at 3 T, offers a good compromise in the quality of images.
Injection protocol
A GBCA bolus injection should commence within 20 seconds after the start of the T2* DSC sequence to establish a precontrast baseline. A power injector is used to inject at a minimum rate of 4 mL/s, followed by a saline flush at the same rate, through an 18- to 22-gauge peripheral intravenous line. A 0.1 mmol/kg dose of GBCA is generally recommended. When the possibility of contrast agent extravasation exists (ie, evaluation of brain tumors), a preload-correction approach is recommended. Although the optimal amount of preload dosing of GBCA is not entirely clear, work by Hu and colleagues found that at 3 T, a preload dose of 0.1 mmol/kg administered 6 minutes before the DSC acquisition injection seemed to provide correction for leakage effects and to obtain the highest accuracy of CBV. If combined permeability and perfusion MR imaging is being performed, then it is recommended that the dose be split into 2 equivalent 0.05 mmol/kg doses.
There is no clear consensus in the choice of GBCA. High relaxivity contrast agents such as gadobenate dimeglumine allows high-quality (relative CBV [rCBV]) maps. Gadobenate dimeglumine and high-concentration GBCA gadobutrol give similar high-quality perfusion maps at a dose of 0.1 mmol/kg at 1.5 T, although at 3 T gadobutrol seems to offer advantages over gadobenate dimeglumine. A recent study concluded that DSC-MR imaging with a blood pool agent such as ferumoxytol may provide a better monitor of tumor rCBV than DSC-MR imaging with gadoteridol.
Image processing
First, the GBCA concentration–time curve is calculated based on the susceptibility signal intensity–time curve. GBCA concentration is assumed to be proportional to the change in relaxation rate ΔR2* (or ΔR2 if SE sequence is used), which can be calculated from the signal intensity via use of Equation 1:
where S(t) is the signal intensity in the voxel at time t and S0 is the baseline signal intensity before the bolus arrives.
A gamma-variate function is then generally fitted to the curve to eliminate contribution of tracer recirculation.
The most common processing methods used in clinical work give qualitative parametric maps assuming a constant arterial input function in all the pixels. rCBV is calculated from the area under the curve, realtive MTT (rMTT) is calculated from the first moment of the measured efflux concentration–time curve (ie, the weighted arithmetic mean of the time values represented in the concentration–time curve), and rCBF is equal to rCBV/rMTT according to the central volume principle. These maps do not afford quantitative assessment of brain hemodynamics but provide indicators of hemodynamic disturbances that are very useful in a clinical setting. They can be interpreted visually or semiquantitatively by calculating the ratio or difference between the values in a region of interest (ROI) placed in the abnormal area and a contralateral ROI placed in the area considered as a normal reference.
To quantitatively determine CBF (mL/100 g/min) and MTT (seconds), the arterial input function (AIF) must be known to correct for bolus delay and dispersion. Following deconvolution of the concentration–time curve with the AIF, MTT and CBF can be determined from the tissue residue function: CBF is the peak of the residue function and MTT is the weighted arithmetic mean of the time of transit values. CBV (in mL/100 g) is then equal to CBF × MTT according to the central volume principle.
As opposed to the relationship between attenuation and contrast agent concentration in CT perfusion, there may not always exist a linear relationship between MR signal intensity and tissue contrast agent concentration in DSC-MR imaging. In clinical context, this nonlinear relationship is often ignored; this can lead to substantial errors in absolute quantification of DSC-MR imaging.
Permeability: DCE-MR Imaging
Principle
DCE-MR imaging is used to characterize the functional integrity of the BBB via estimation of microvascular permeability parameters. During T1-weighted DCE-MR imaging, the contrast agent accumulation results in T1-shortening and positive enhancement. Through pharmacokinetic modeling of contrast agent accumulation into the extravascular-extracellular space (EES), several parameters can be determined (see Fig. 1 ) :
- •
Transfer constant ( K trans ), frequently called vascular permeability, is a combination of capillary wall permeability surface area product per unit volume of tissue ( PS ) and capillary blood flow ( F )
- •
Volume of the EES per volume of tissue ( v e )
- •
Fractional blood-plasma volume ( v p )
- •
Rate constant between EES and blood plasma ( k ep , where k ep = K trans / v e )
Image acquisition
Baseline T1 mapping is performed before the acquisition of the DCE images. This is necessary to apply pharmacokinetic modeling because the relationship between the measured signal intensity and contrast agent concentration is nonlinear. The most commonly used method is a multiple flip angle gradient echo acquisition but inversion or saturation recovery techniques could also be used.
Then rapid repeated T1-weighted images are acquired before, duringm and after bolus GBCA administration for several minutes. This is commonly performed using gradient-echo sequence (spoiled gradient echo [SPGR], volume interpolated gradient echo [VIBE], magnetization-prepared rapid acquisition with gradient echo [MPRAGE]) that provides adequate compromise between temporal resolution, volume coverage and sensitivity to T1 effects. Although 2D sequences could be used, 3-dimensional sequences are the preferred technique because of its better signal-to-noise-ratio and less severe distortions.
The acquisition time for the dynamic acquisition should be at least 3 to 5 minutes, and a temporal resolution of between 3.5 and 6 seconds would be optimal. The recommended matrix resolution is 128 × 128. Slice thickness could range between 2 to 7 mm depending on the need for volume coverage. To improve temporal and/or spatial resolution, parallel imaging methods or other undersampling methods such as highly constrained back-projection or compressed sensing methods can be used.
Injection protocol
GBCA bolus injection should commence within 20 seconds after the start of the T1 DCE sequence to establish a precontrast baseline. A power injector is used to inject through an 18- to 22-gauge peripheral intravenous line, at a rate of 2 to 5 mL/s, followed by a saline flush at the same rate. A 0.1 mmol/kg dose of contrast agent is generally recommended. If combined permeability and DSC-MR imaging is being performed, then it is recommended that the dose be split into 2 equivalent 0.05 mmol/kg doses followed by a 10-mL saline flush.
Image processing
Many methods have been described to analyze DCE-MR imaging, from simple measurement of MR signal changes to physiologic methods using pharmacokinetic models.
Descriptive methods examine simple descriptions of the signal intensity–time curve, such as percentage of enhancement, curve shape, wash-in and wash-out slopes, or time to 90% enhancement. To improve reproducibility and repeatability, determination of the contrast–concentration curve could be derived from signal intensity–time curve. A simple descriptor as the initial area under the contrast agent concentration–time curve can be calculated without pharmacokinetic modeling. It is widely used in drug trials and seems to have fair reproducibility. However, what it represents physiologically is unclear because it is a combination of blood volume, flow, permeability, and EES volume.
Permeability metrics can also be extracted from the concentration–time curve using pharmacokinetic models, which in theory should limit individual patient variation, scanner type, or imaging technique. Most of pharmacokinetic models applied to DCE-MR imaging are compartmental models. A simplification of the pharmacokinetic model was proposed by Patlak and colleagues, to estimate K trans with a graphic approach in case of limited permeability. Models proposed by Toft and Kernode and Larson and colleagues define K trans (min −1 ) and v e neglecting the contribution of the intravascular compartment. However, when there is a large increase in blood volume (ie, in high-grade tumor), ignoring the contribution of the intravascular tracer may be problematic. Extensions of this model that take into consideration the contribution the intravascular contrast have been developed that allow modeling of v p in addition to K trans and v e . These models provide a more accurate calculation of K trans and v e . Because K trans is a composite parameter depending on the relationship between flow and PS, more complex models, such as the adiabatic tissue homogeneity model, separate flow and PS. However, these models demand a very high temporal resolution and a high quality of data.
An AIF is needed for the models just described. Ideally, the AIF should be determined in an artery local to the tissue of interest for each examination. But an accurate measurement is challenging. Several techniques have been proposed, but many groups use an idealized mathematical function, based on population-averaged AIF.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree