Acute and chronic ankle inversion injuries are a common source of pain and a diagnostic challenge. Several studies have shown a variety of injury patterns after inversion injury both in acute and chronic settings. Although traditional assessment with clinical examination and radiographs is generally accepted for inversion injuries, MR imaging is a useful tool to detect occult injuries and in patients with chronic symptoms. This article examines a range of MR imaging findings that may be present in patients with lateral ankle pain following an acute or chronic inversion injury.
Key points
- •
MRI is the method of choice to characterize soft tissue and osseous injuries, which can involve both the lateral and medial ankle after inversion injuries.
- •
Injury to anterior talofibular ligament is the most common sequela of ankle inversion injury, however additional ligamentous and bony lesions may be present.
- •
MRI can detect occult injuries that are not apparent during radiographic or clinical workup, which may affect functional outcome.
Introduction
Acute ankle injuries rank among the most common musculoskeletal injuries, affecting both elite athletes and the general population, resulting in up to 10% of emergency room visits. Approximately 80% to 90% of injuries involve the lateral ankle ligaments, being more common in sports that require running and jumping, which account for up to 25% of total injuries. Importantly, long-term residual symptoms after an acute injury are increasingly reported. In prior studies, 74% of patients had recurrent or residual symptoms up to 4 years after an acute inversion injury, and 32% of patients had recurrent complaints up to 7 years following the initial injury.
Traditional assessment with clinical examination and radiographs is usually performed for inversion injuries. However, clinical examination alone can be unreliable in the acute setting because of pain, with standard and stress-view radiographs being limited by ankle orientation, amount of force applied, and the patient’s ability to cooperate with the examination. In contrast, MR imaging grading of ligamentous injury can predict clinical outcomes and correlates with return to sporting activity. MR arthrography may also be useful in patients with chronic lateral ankle instability compared with stress radiographs and conventional MR imaging when assessing for full-thickness tears. Importantly, the accurate delineation of soft tissue and osseous anatomy and the characterization of ankle ligamentous injury by MR imaging have been well documented.
Although anterior talofibular ligament injury is by far the most common occurrence in ankle inversion injuries, additional findings that go underdiagnosed by usual radiographic or clinical work-up may affect the clinical course and outcome in both acute and chronic cases. Osteochondral injuries and occult fractures, complex lateral ankle ligament tears, syndesmotic injury, sinus tarsi syndrome, countercoup and deltoid ligament injury, as well as tendon and retinacular injury occur in inversion injuries and can be diagnosed by MR imaging. Therefore, familiarity with features of ankle inversion injury by MR imaging is important to comprehensively characterize the consequences of this type of skeletal trauma.
Introduction
Acute ankle injuries rank among the most common musculoskeletal injuries, affecting both elite athletes and the general population, resulting in up to 10% of emergency room visits. Approximately 80% to 90% of injuries involve the lateral ankle ligaments, being more common in sports that require running and jumping, which account for up to 25% of total injuries. Importantly, long-term residual symptoms after an acute injury are increasingly reported. In prior studies, 74% of patients had recurrent or residual symptoms up to 4 years after an acute inversion injury, and 32% of patients had recurrent complaints up to 7 years following the initial injury.
Traditional assessment with clinical examination and radiographs is usually performed for inversion injuries. However, clinical examination alone can be unreliable in the acute setting because of pain, with standard and stress-view radiographs being limited by ankle orientation, amount of force applied, and the patient’s ability to cooperate with the examination. In contrast, MR imaging grading of ligamentous injury can predict clinical outcomes and correlates with return to sporting activity. MR arthrography may also be useful in patients with chronic lateral ankle instability compared with stress radiographs and conventional MR imaging when assessing for full-thickness tears. Importantly, the accurate delineation of soft tissue and osseous anatomy and the characterization of ankle ligamentous injury by MR imaging have been well documented.
Although anterior talofibular ligament injury is by far the most common occurrence in ankle inversion injuries, additional findings that go underdiagnosed by usual radiographic or clinical work-up may affect the clinical course and outcome in both acute and chronic cases. Osteochondral injuries and occult fractures, complex lateral ankle ligament tears, syndesmotic injury, sinus tarsi syndrome, countercoup and deltoid ligament injury, as well as tendon and retinacular injury occur in inversion injuries and can be diagnosed by MR imaging. Therefore, familiarity with features of ankle inversion injury by MR imaging is important to comprehensively characterize the consequences of this type of skeletal trauma.
MR imaging protocol
A detailed description of MR imaging technique for foot and ankle is beyond the scope of this article and is covered elsewhere (see Won C. Bae, Thumanoon Ruangchaijatuporn, Christine B. Chung’s article, “New Techniques in MR Imaging of the Ankle and Foot ,” in this issue).
However, brief general comments on technique are worth emphasizing in the context of lateral ankle ligamentous injury. MR imaging of the ankle is challenging because of a combination ankle spatial configuration, anatomic complexity, and inherent small size of ankle ligaments. Accurate diagnosis of disorder after an inversion injury hinges on the ability to assess the integrity of ligaments and articular cartilage, as well as identify subtle areas of bone marrow or soft tissue edema. Hallmarks of high-quality ankle MR imaging include uniform fat suppression, high signal-to-noise ratio (SNR), and elimination/minimization of artifacts. Although 3.0-T MR imaging systems allow higher spatial resolution and/or shorter imaging times, MR imaging at 1.5 T has proved effective for almost all musculoskeletal imaging applications, including the ankle. Nonetheless, the benefit of obtaining ankle MR imaging at higher field strengths is apparent when assessing subtle ligamentous injury that may require higher spatial resolution, or when attempting to grade the severity of ligamentous injury, which may benefit from higher SNR.
Fat-suppressed images are necessary to detect subtle soft tissue or bone marrow edema, which are critical to fully characterize an injury. Although frequency-selective suppression of fat signal on fast spin-echo imaging is accepted practice, alternative techniques are emerging to improve fat suppression, increase SNR, and optimize image quality. One such technique uses multiecho Dixon techniques for fat and water separation to produce more uniform fat suppression with high SNR. This technique is less sensitive to magnetic field inhomogeneities and eliminates the need for selective fat suppression, which frequently is uneven adjacent to curved surfaces of the ankle. This characteristic may be especially problematic adjacent to the malleoli and in the setting of prior metallic hardware placement, and can be exacerbated when using higher field strengths.
In order to adequately evaluate the lateral ankle ligaments and adjacent soft tissues, it is necessary to optimize the imaging planes and coverage during MR imaging examination. Coronal and axial images are most appropriate for ankle ligament assessment. Axial coverage should extend from above the distal tibiofibular syndesmosis to the plantar soft tissues to ensure visualization of all lateral ligamentous structures. The coronal plane should be optimally placed along a line connecting both malleoli, which provides the best depiction of medial and lateral ligaments. If more detailed assessment is required, multiplanar reconstruction from two-dimensional or three-dimensional image data sets may be useful to provide nonstandard planes to visualize medial and lateral ankle ligaments.
The optimal positioning of the foot and ankle before imaging is debated, with evidence showing no significant difference in ligament assessment between dorsiflexion and usual position of the ankle (20° of plantar flexion) in the supine position. Further, strict positioning of the ankle during MR imaging examination may not be reproducible depending on foot size, coil configuration, and discomfort during scanning. Therefore, a balance between optimal positioning and comfort to avoid motion should be considered. Although no uniform standard exists for appropriate coil selection in ankle imaging, dedicated MR imaging coils with multichannel phase-array elements provide best results. However, excellent images can also be obtained with surface or extremity coils, as long as adequate coverage and contact are achieved.
Disorders
Lateral Ligamentous Injuries
Anterior talofibular ligament, calcaneofibular ligament, posterior talofibular ligament
Biomechanical studies have shown that the anterior talofibular ligament (ATFL) is the weakest of the lateral ankle ligaments, followed by the calcaneofibular ligament (CFL) and posterior talofibular ligament (PTFL). As such, the ATFL is most susceptible to injury, with the remaining ligaments being involved sequentially based on their biomechanical properties. The PTFL is rarely torn, except in cases of complete ankle dislocation and/or severe tibiofibular syndesmotic injury, and is consistently associated with injury of ATFL and CFL. The most common mechanisms for lateral ankle ligamentous injury are inversion and plantar flexion.
The ATFL originates at the anterior margin of the lateral malleolus and attaches to the talar body, anterior to the articular surface. Although variation does occur, the normal thickness of the ATFL on MR imaging has been described to be approximately 2 mm. The ATFL is generally divided into 2 bands by perforating branches of the peroneal artery, which occasionally can be appreciated on MR imaging. The number of ATFL bands varies between 1 and 3, with different descriptions found in the literature. Although these bands are inconsistently visualized on MR imaging, the increasing use of high field strength imaging has made such identification more common. Functionally, the ATFL is important during plantar flexion, preventing anterior displacement of the talus. As such, the ATFL is vulnerable to injury especially under plantar flexion and inversion, placing the ligament under maximal strain.
The CFL originates from the anterior aspect of the lateral malleolus, often with a partial connection to the ATFL at the fibula, and runs caudally and posteriorly to its attachment site on the lateral calcaneus. It is the second most commonly injured ligament of the lateral ankle. The CFL can be injured even in the absence of dorsiflexion or plantar flexion if stressed under varus foot positioning. The CFL is an important lateral stabilizer and helps restrain calcaneal inversion, elongating mostly during dorsiflexion and pronation. The peroneal retinaculum is in close proximity to the CFL and should not be confused with the ligament, because the retinaculum courses superficial, whereas the CFL runs deep to the peroneal tendons. The normal thickness of the CFL on MR imaging has been described to be approximately 3 mm. When evaluating the CFL by MR imaging, note that the peroneal tendons travel superficial to the ligament, often resulting in an indentation.
The PTFL is the strongest of the lateral ankle ligaments and is rarely injured. It spans from the lateral malleolar fossa to the posterolateral talus, with a horizontal trajectory. It is usually interconnected with fibers from the posterior intermalleolar ligament and contains numerous fascicles that yield a normal striated appearance on MR imaging, which should not be confused with abnormality. Dorsiflexion increases tensile stress to the PTFL and the ligament limits anterior and posterior displacement of the talus in relation to the tibia and fibula.
During an acute ankle sprain, an acute inflammatory response occurs during the first 3 days and a hematoma can form at the margins of a complete ligamentous tear. Defects within the ligament can generally be seen within the first 2 weeks of injury, and by 7 weeks reparative remodeling has occurred to the point that the defect is no longer visualized, and the injured ligament is either attenuated or thickened, findings that are seen with subacute and chronic injuries. However, the reparative process may fail to reconstitute the ligament, in which case it will not be visualized on MR imaging. Bony proliferative changes can occur at attachment sites or within the substance of the ligament with chronic injuries. Although MR imaging is excellent to assess the integrity and stage of healing of ligamentous injuries, false-positive results do occur. In one prospective study, approximately 30% of patients with asymptomatic lateral ankles had an abnormal-appearing ATFL on MR imaging, which should be considered when evaluating lateral ankle ligaments. Correlation with physical examination and clinical history are important components of accurate image interpretation.
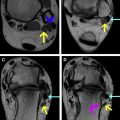
As seen in other anatomic sites, MR imaging findings of acute ankle ligamentous injury include fiber discontinuity, thickening or attenuation of ligament, contour abnormalities, and intrasubstance signal changes. MR imaging grading of ligamentous injuries of the ankle follows the usual schema suggested for other ligaments based on T2-weighted MR imaging findings: grade 1, intrasubstance stretching without visible tears; grade 2, partial thickness tear; and grade 3, complete disruption of the ligament. As an important aside, MR imaging grading must be used with caution and in agreement with referring specialists, because it does not always reliably correlate with surgical findings. Extra-articular joint fluid arising from a fluid-filled ligamentous defect, particularly with injury to the ATFL, can be helpful to identify high-grade tears ( Figs. 1 and 2 ). Other findings may include bone marrow edema/contusion, adjacent soft tissue edema, or associated avulsion fracture ( Fig. 3 ). A common finding in chronic high-grade lateral ligament injuries is nonvisualization of a given ligament, with resulting prominent articular recess ( Figs. 4 and 5 ). Acute CFL injury can result in thickening or discontinuity of fibers with surrounding soft tissue edema ( Fig. 6 ). Associated thickening caused by sprain of the superior peroneal retinaculum and fluid in the peroneal tendon sheath are common secondary findings seen in lateral ankle ligament injuries. The PTFL is rarely ruptured because of its intrinsic load capacity, therefore injury often results in intrasubstance loss of its normal fascicular appearance.


Injury to lateral ankle ligaments is linked to lateral ankle instability and functional ankle instability can result from unbalanced loading to the ankle joint. Studies evaluating cartilage T2 mapping and other advanced imaging techniques have shown peak cartilage strain as well as increased T2 relaxation time after lateral ligamentous injury, suggesting that lateral ankle ligament injury can lead to acceleration of tibiotalar osteoarthritis in combination with chronic ankle instability.
Regarding evaluation of chronic lateral ankle ligament injuries, MR imaging has been proposed as an important component of patient work-up; however, a study by Park and colleagues showed that the sensitivity of MR imaging to detect CFL chronic injuries was higher than for ATFL (44%–75% for ATFL, 50%–83% for CFL). In contrast, Kumar and colleagues reported higher MR imaging sensitivity for detection of ATFL tears compared with CFL tears (87% for ATFL, 47% for CFL). Nonetheless, there is a high specificity and positive predictive value compared with arthroscopic findings in the diagnosis of chronic ankle pain and/or instability, showing up to 100% specificity for the diagnosis of ATFL and CFL tears and osteochondral lesions. For these reasons, symptomatic patients with negative MR imaging findings may still require an arthroscopy for a definitive diagnosis.
Tibiofibular syndesmosis
Injury to the distal tibiofibular syndesmosis, or high ankle sprain, is a well-recognized but often overlooked cause of chronic lateral ankle pain and instability. The incidence of tibiofibular syndesmosis injury ranges from 1% to 20%, commonly with a protracted recovery time. Injury can be associated with other ligaments or ankle fractures ; however, isolated syndesmotic injury in acute scenarios can occur in approximately 16% of athletes, with the most common injury patterns being dorsiflexion and external rotation. Functionally, the syndesmotic ligament complex serves as a stabilizer of the distal tibia and fibula, resisting axial, rotational, and translational forces.
The distal tibiofibular syndesmosis is a complex structure composed of 4 syndesmotic ligaments: anterior inferior tibiofibular ligament (AITFL), posterior inferior tibiofibular ligament (PITFL), interosseous tibiofibular ligament (IOTFL), and inferior transverse tibiofibular ligament. Although syndesmotic injury has traditionally been associated with high fibular fractures and certain types of Weber B fibular fractures, pure ligamentous injury without fracture is possible. In the acute traumatic setting, MR imaging has been shown to reliably identify syndesmotic injuries that were otherwise occult on radiographs and clinically. MR imaging findings of acute syndesmotic injury consist of rupture or abnormal intrasubstance signal within the ligaments, occasionally with bony avulsion from either the tibial or fibular attachment sites, which often result in widening of the syndesmosis. The reported sensitivity of MR imaging for syndesmotic injury ranges from 93% to 100%.
The AITFL is the most commonly injured syndesmotic ligament and is almost always injured before other syndesmotic ligaments. Because of its oblique trajectory from the tibia to the fibula, it usually is seen in multiple consecutive axial images and requires careful assessment, because this off-axial orientation has been reported to affect diagnostic accuracy. The origin of the AITFL is the anterolateral tibial tubercle and it extends laterally and distally to insert in the anterior margin of the fibula, coursing in an oblique fashion. The MR imaging features of an acute injury to the AITFL include discontinuity, laxity, or irregular configuration ( Fig. 7 ). Although a small amount of fluid can be seen in a normal recess of distal tibiofibular syndesmosis, a recess height greater than 1 cm might prompt consideration of prior syndesmotic injury. Chronic injury patterns span from complete disruption to a diminutive or thickened appearance, frequently with adjacent small areas of mineralization ( Fig. 8 ). Synovial hypertrophy is a commonly reported finding both at arthroscopy and MR imaging as a secondary finding. Thickening of an accessory AITFL can abut the talar dome and cause pain, resulting in anterolateral impingement. This accessory ligament resides inferior to the AITFL and is also known as the Basset ligament. Because of the high incidence of this variant (70%–92% incidence on MR imaging), many investigators believe it to be a normal anatomic structure and may refer to it as the distal fascicle of the AITFL ( Fig. 9 ).