Impingement is a clinical syndrome of chronic pain and restricted range of movement caused by compression of abnormal bone or soft tissue within the ankle joint. It usually occurs following a sprain injury or repetitive microtrauma causing haemorrhage, synovial hyperplasia, and abnormal soft tissue interposition within the joint. MR imaging is particularly valuable in being able to detect not only the soft tissue and osseous abnormalities involved in these syndromes, but also a wide variety of other potential causes of ankle pain and instability that also may need to be addressed clinically.
Key points
- •
Impingement is a clinical syndrome of chronic pain and restricted range of movement caused by compression of abnormal bone or soft tissue within the ankle joint.
- •
Common sites of impingement in the ankle include posterior, posteromedial, anteromedial, anterolateral, and, less commonly, direct anterior; these often coexist and occur in conjunction with other ankle pathologies.
- •
The presence of synovitis, pericapsular oedema and bone marrow oedema on MR imaging support a diagnosis of impingement in the right clinical context.
- •
In most cases ankle impingement is managed conservatively, with arthroscopic or open debridement of the abnormal bone or soft tissue reserved for refractory cases.
Introduction
Impingement syndromes of the ankle are a common cause of chronic pain, instability, and limited range of movement in athletes and the active population. They most commonly occur after a sprain injury or repetitive microtrauma at the extreme ranges of movement. The resultant hemorrhage, reactive synovial hyperplasia, and scarring can lead to abnormal soft tissue interposition within the joint. Developmental or acquired bony spurs or prominences also may impede the normal range of movement. It is painful soft tissue or osseous entrapment within the joint that characterises impingement. The diagnosis is largely clinical but may be supported with a range of imaging techniques. MR imaging is particularly valuable in being able to detect not only the soft tissue and osseous abnormalities involved in these syndromes but also a wide variety of concomitant injuries and other potential causes of ankle pain that also may need to be addressed clinically. It is important to remember that although MR imaging findings help direct surgery and have a high concordance with surgical findings, subclinical asymptomatic disease is often present in athletes, and close correlation with the clinical picture is required.
This heterogenous group of pathologies is categorized according to the anatomic relation to the tibiotalar joint. Broadly speaking there are 3 main types :
- 1.
Anterior impingement, which can be subdivided into anterolateral, anteromedial, and purely anterior impingement.
- 2.
Posterior impingement, subdivided into posterior and posteromedial impingement.
- 3.
Extra-articular lateral hindfoot impingement, which encompasses talocalcaneal and subfibular impingement secondary to a planovalgus foot deformity.
In most cases, ankle impingement is managed conservatively, with arthroscopic or open debridement of the joint reserved for refractory cases. In this review, we describe the anatomy, pathophysiology, clinical presentation, imaging features, and treatment approach of each of ankle impingement syndrome, with a focus on the MR imaging findings.
Introduction
Impingement syndromes of the ankle are a common cause of chronic pain, instability, and limited range of movement in athletes and the active population. They most commonly occur after a sprain injury or repetitive microtrauma at the extreme ranges of movement. The resultant hemorrhage, reactive synovial hyperplasia, and scarring can lead to abnormal soft tissue interposition within the joint. Developmental or acquired bony spurs or prominences also may impede the normal range of movement. It is painful soft tissue or osseous entrapment within the joint that characterises impingement. The diagnosis is largely clinical but may be supported with a range of imaging techniques. MR imaging is particularly valuable in being able to detect not only the soft tissue and osseous abnormalities involved in these syndromes but also a wide variety of concomitant injuries and other potential causes of ankle pain that also may need to be addressed clinically. It is important to remember that although MR imaging findings help direct surgery and have a high concordance with surgical findings, subclinical asymptomatic disease is often present in athletes, and close correlation with the clinical picture is required.
This heterogenous group of pathologies is categorized according to the anatomic relation to the tibiotalar joint. Broadly speaking there are 3 main types :
- 1.
Anterior impingement, which can be subdivided into anterolateral, anteromedial, and purely anterior impingement.
- 2.
Posterior impingement, subdivided into posterior and posteromedial impingement.
- 3.
Extra-articular lateral hindfoot impingement, which encompasses talocalcaneal and subfibular impingement secondary to a planovalgus foot deformity.
In most cases, ankle impingement is managed conservatively, with arthroscopic or open debridement of the joint reserved for refractory cases. In this review, we describe the anatomy, pathophysiology, clinical presentation, imaging features, and treatment approach of each of ankle impingement syndrome, with a focus on the MR imaging findings.
Anterior impingement syndrome
Anterior ankle impingement is a well-established and relatively common cause of chronic ankle pain, particularly in soccer players, runners, and ballet dancers, who sustain repetitive ankle dorsiflexion. Symptoms are generally progressive and relate to impingement of hypertrophied synovial scar tissue and bony spurs within the anterior ankle joint.
Anatomy and Pathophysiology
Ankle instability or repetitive forceful dorsiflexion can result in microtrauma to the anterior joint cartilage and deeper bone layers. Over time, attempted repair, including fibrosis and fibrocartilage proliferation, leads to the formation of bony spurs on the anterior rim of the tibia and sulcus of the talus. These bony spurs or osteophytes can cause anterior joint space narrowing, limiting ankle dorsiflexion ( Fig. 1 ). The term osteophyte does not imply conventional osteoarthritis, rather a proliferative effect of focal premature degeneration. Like any other osteophyte, however, they may break off into the joint, forming a loose body.
Repetitive supination injuries are also known to cause osteophyte formation secondary to damage to the anterior and medial margin of the articular cartilage. Another proposed aetiological factor is direct microtrauma caused by ball striking in soccer with direct impact of the ball typically over the anteromedial tibiotalar joint, where the cartilage is covered only by thin subcutaneous fat. Both mechanisms described occur frequently in soccer players, and it is therefore unsurprising that this population of athletes is so commonly afflicted. Indeed, the condition was first described in European soccer players as “footballer’s ankle.” The theory hypothesised at the time, however, was one of repetitive traction injury of the anterior joint capsule in extreme plantarflexion causing anterior exostoses. This is certainly not the case in the anteromedial ankle, where cadaveric analysis has shown that the bony spurs are intra-articular, consistent with osteophyte formation. The traction hypothesis, however, may still hold true laterally, where growth is sometimes extra-articular and may represent enthesophyte formation.
It is important to remember that the finding of anterior bone spurs does not necessarily mean that the patient is symptomatic. Studies of asymptomatic athletes have found that a significant proportion (45%–59%) have anterior tibiotalar spurs on plain radiograph. It is thought that the associated anterior synovial thickening and scarring, rather than the spurs alone, are responsible for producing the clinical symptoms. Indeed, postexcision recurrence of the bony spurs is not necessarily accompanied by recurrence of symptoms. Recent attention has been given to congenital anatomic variants as predisposing factors for the formation of anterior joint space spurs and soft tissue hypertrophy. A cam-type deformity of the talar dome has been described, whereby contact between a noncircular arc morphology of the dome with the anterior tibial plafond during dorsiflexion causes abnormal loading of the talar dome cartilage. In these patients, a cavo-varus foot type is more commonly observed, and the associated external rotation of the tibia is thought to further reduce the tibiotalar joint space. In addition, the orthopaedic literature describes several cases of soft tissue anterior impingement treated successfully by arthroscopic resection of a congenital intra-articular plicae or fibrous bands.
Clinical Presentation
The typical symptoms are of chronic anterior ankle pain with subjective feeling of blocking on dorsiflexion. On examination, there is restricted and painful dorsiflexion. There may also be a palpable soft tissue swelling or a spur over the anterior joint. The palpable bone spurs are commonly felt over the anteromedial aspect, whereas the symptoms of soft tissue impingement are on the anterolateral aspect of the ankle.
Imaging Features
Diagnosis of anterior impingement is primarily clinical, but conventional, preferably weight-bearing, radiographs are useful for the evaluation of bony spurs and the tibiotalar joint space ( Fig. 2 ). Anteromedial osteophytes are best demonstrated on the oblique anteromedial impingement (AMI) view. The plié view (lateral weight-bearing view with the ankle in maximal dorsiflexion) can demonstrate joint space loss and osseous impingement. Radiographic assessment of the tibiotalar joint for secondary signs of degeneration, particularly joint space loss, has prognostic importance. The Van Dijk radiographic classification system, based on osteophyte appearance and degree of joint space narrowing, demonstrated the importance of osteoarthritis as a postoperative prognostic factor. Several more recent studies have agreed that secondary osteoarthritis confers a poorer postoperative prognosis.
Further imaging is usually unnecessary. Conventional MR imaging can be used, however, to further characterise the location of the spurs within the joint space and to review the degree of synovitis and joint capsule thickening ( Fig. 3 ). It is also useful to check for concomitant pathology, such as osteochondral lesions that may not have been detected on radiography.
Treatment
- •
Most patients recover with conservative measures, including rest, activity modification, and physical therapy. Particularly in ballet dancers this should be performed in conjunction with correction of technique to correct overpronation where appropriate. Ultrasound can be used to direct intra-articular injection of cortisone and local anaesthetic ( Fig. 4 ).
Fig. 4
Sagittal ultrasound of the anterior tibiotalar joint in a rugby player shows hypoechoic synovitis in the anterior joint space ( long arrow ), and an anterior tibial spur ( short arrow ). Ultrasound was used to direct intra-articular injection of corticosteroid and local anaesthetic.
- •
In resistant cases, however, surgery has been shown to have a long-term benefit. In athletes, arthroscopic resection of the osseous spurs and soft tissue abnormality has shown excellent functional and symptomatic results. The overall prognosis after surgery does depend on the degree of degenerative change evident in the rest of the tibiotalar joint at the time of the surgery.
Anterolateral impingement syndrome
Anterolateral impingement is well described in the orthopedic and radiology literature and describes soft tissue hypertrophy and entrapment within the anterolateral recess of the ankle. It is classically described in young athletic patients following an inversion sprain injury with subsequent chronic anterolateral pain and swelling.
Anatomy and Pathophysiology
The anterolateral recess is a triangular structure bordered posteromedially by the anterolateral tibia and talus and posterolaterally by the anterior fibula. Anteriorly it is bordered by the anterolateral joint capsule and capsular ligaments. These include the anterior talofibular, anterior inferior tibiofibular and calcaneofibular ligaments ( Fig. 5 ). Ligamentous and capsular tearing and the resultant microinstability and haemorrhage following an ankle sprain may lead to reactive synovial hyperplasia and scarring in the anterolateral gutter. Compression of the abnormal soft tissue in the anterolateral gutter during dorsiflexion or eversion can cause severe morbidity and pain, particularly amongst athletes and the younger population. It is estimated that the incidence of anterolateral impingement syndrome is 3% following ankle sprains. In advanced cases, the soft tissue can become molded to the triangular shape of the anterolateral gutter. This connective tissue mass was originally described as a “meniscoid lesion” based on its macroscopic meniscuslike appearance.
Anterolateral impingement also has been described in a subset of patients with an accessory fascicle of the anteroinferior tibiofibular ligament. The ligament is invariably multifascicular, but a discreet inferior fascicle separated from the main body by a fibrofatty septum is variably present (identified in 21%–97% of ankles depending on the exact definition) and considered a normal variant. The accessory fascicle of the anteroinferior tibiofibular ligament (Bassett ligament) may normally contact the anterolateral corner of the talus but it is thought that increased contact in dorsiflexion may lead to synovial hypertrophy and impingement within the anterolateral joint space. Ligamentous abrasion of the exposed anterolateral talar cartilage also can sometimes be seen.
Clinical Presentation
The clinical diagnosis of anterolateral impingement is reasonably accurate and based on the anterolateral tenderness, swelling, and pain exacerbated by single-leg squatting, ankle eversion, or dorsiflexion. A provocative physical examination test can be performed in which pressure is applied over the anterolateral ankle while the ankle is brought from the plantar flexed position to full dorsiflexion. A 94.8% sensitivity and 88.0% specificity was reported in a prospective study.
Imaging Features
Anterolateral impingement is predominantly a soft tissue abnormality and therefore radiography and conventional computed tomography (CT) have limited specific utility. Ultrasound and MR imaging can potentially detect abnormal nodular soft tissue extruding anteriorly from the anterolateral gutter. In a retrospective evaluation of ultrasound in a small group of elite soccer players with resistant anterolateral impingement awaiting arthroscopy, synovitic lesions were detected using ultrasound with 100% sensitivity ( Fig. 6 ).
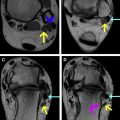
MR imaging has the advantage over ultrasound in being able to assess for whole ankle pathology, including coexisting or alternative causes of prolonged ankle pain, such as marrow contusions, chondral lesions, intra-articular bodies, and sinus tarsi syndrome. MR imaging can show synovial hypertrophy in the anterolateral recess.
The most reliable sign is the obscuration of the anterolateral recess with scar tissue ( Fig. 7 ). It must be remembered that an abnormal nodular or irregular contour of the recess is commonly found in the asymptomatic population and can merely reflect previous anterolateral trauma or surgery. The diagnostic ability of MR imaging in the absence of joint distention with either contrast material or a native effusion remains controversial, with some investigators previously preferring MR arthrography, as it has a reported sensitivity of 97% and specificity of 100%.
However, with advances in MR imaging hardware technology, MR arthrography is now largely redundant and, with sufficient experience, the diagnosis can be made on conventional MR imaging with relative confidence (75%–83% sensitivity and 75%–100% specificity, depending on the experience of the reporter). Axial T1-weighted images were deemed the most useful for detecting the intermediate to low signal hypertrophy and scarring in the anterolateral gutter. Sagittal T1-weighted images are a useful adjunct, demonstrating anterior displacement of the normal hyperintense fat anterior to the fibula by the hypointense scar tissue. Specificity, however, for all these findings on ultrasound or MR imaging is poor, particularly with regard to the detection of thickened nonenhancing scar tissue.
Treatment
- •
The initial treatment is conservative, with immobilization, physiotherapy, and nonsteroidal anti-inflammatory medication. Dry needling of the abnormal soft tissue with an intra-articular injection of cortisone and local anaesthetic may be performed under ultrasound guidance, allowing a return to previous levels of activity, even in elite athletes, but this technique has not been evaluated in the literature.
- •
If these measures fail, arthroscopic evaluation and resection of hypertrophied synovium and scar tissue, including the distal fascicle of the anterior tibiofibular ligament when that is the underlying etiology, has yielded good to excellent symptomatic and functional results.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree