Heel pain is common and due to a variety of osseous and soft tissue disorders. Causes of heel pain can be classified by the anatomic structure in which they arise and include disorders of the (1) Achilles tendon, (2) plantar fascia, (3) calcaneus, (4) bursae, (5) nerves in the hindfoot, (6) and heel pad. Although careful history taking and physical examination are important, imaging plays a vital role in the diagnosis and management of heel pain. MR imaging is the best imaging test to assess pain in the heel. This review discusses the common causes of heel pain, focusing on MR imaging appearances.
Key points
- •
Knowledge of the anatomic structures that form the heel is important in understanding the various osseous and soft tissue causes of heel pain.
- •
Common causes of heel pain include disorders of the Achilles tendon, plantar fascia, calcaneus, bursae, nerves in the tarsal tunnel, and heel pad.
- •
MR imaging is the best imaging modality to assess heel pain due to its superior soft tissue contrast and ability to localize the site end extent of disease.
Introduction
Heel pain is common and accounts for more than 1 million doctor visits annually in the United States. Several osseous and soft tissue disorders can lead to heel pain and it is important for both radiologists and clinicians to be familiar with the relevant hindfoot anatomy to arrive at a correct diagnosis. Moreover, it is important to understand the relationship of the various structures with one another because this can have implications for treatment. For instance, abnormalities of the Achilles tendon can lead to a higher incidence of plantar fasciitis. Causes of heel pain can be classified based on the structure in which it arises and can be divided into 6 major anatomic categories : (1) Achilles tendon (tendinopathy, tear, and paratenonitis), (2) plantar fascia (fasciitis, fascial tear, and fibromatosis), (3) calcaneus (stress fracture, osteomyelitis, tumors, and Sever disease), (4) bursae (retrocalcaneal and retro-Achilles bursitis, and Haglund syndrome), (5) nerves (tarsal tunnel syndrome and Baxter neuropathy) (6) and heel pad (fat pad syndrome) ( Table 1 ). Other less common causes of heel pain include avascular necrosis, tarsal coalition, arthritic disorders (osteoarthritis, gout, rheumatoid arthritis, and reactive arthritis), and posterior impingement.
| Anatomic Structure | Disorder |
|---|---|
| Achilles tendon | Achilles tendinopathy (midportion or insertional) Achilles partial tear Achilles complete tear Paratendinopathy or paratenonitis of Achilles tendon |
| Plantar fascia | Plantar fasciitis Plantar fascia tear Plantar fibromatosis |
| Calcaneus | Stress fracture Osteomyelitis Sever disease Tumor (intraosseous lipoma, simple bone cyst, aneurysmal bone cyst, etc.) |
| Bursae | Retrocalcaneal bursitis Retro-Achilles bursitis Haglund syndrome |
| Nerve | Tarsal tunnel syndrome Baxter neuropathy |
| Heel pad | Heel pad syndrome |
Diagnosis of heel pain can be challenging based only on clinical history and physical examination. Imaging can be useful, with MR imaging the most useful imaging modality. MR imaging has great soft tissue contrast and excellent anatomic detail, which allow for assessment of the location and extent of the hindfoot disorder, which can also assist with preoperative planning. This article discusses the most common conditions that cause heel pain based on their anatomic location and emphasizes their MR imaging appearances.
Introduction
Heel pain is common and accounts for more than 1 million doctor visits annually in the United States. Several osseous and soft tissue disorders can lead to heel pain and it is important for both radiologists and clinicians to be familiar with the relevant hindfoot anatomy to arrive at a correct diagnosis. Moreover, it is important to understand the relationship of the various structures with one another because this can have implications for treatment. For instance, abnormalities of the Achilles tendon can lead to a higher incidence of plantar fasciitis. Causes of heel pain can be classified based on the structure in which it arises and can be divided into 6 major anatomic categories : (1) Achilles tendon (tendinopathy, tear, and paratenonitis), (2) plantar fascia (fasciitis, fascial tear, and fibromatosis), (3) calcaneus (stress fracture, osteomyelitis, tumors, and Sever disease), (4) bursae (retrocalcaneal and retro-Achilles bursitis, and Haglund syndrome), (5) nerves (tarsal tunnel syndrome and Baxter neuropathy) (6) and heel pad (fat pad syndrome) ( Table 1 ). Other less common causes of heel pain include avascular necrosis, tarsal coalition, arthritic disorders (osteoarthritis, gout, rheumatoid arthritis, and reactive arthritis), and posterior impingement.
| Anatomic Structure | Disorder |
|---|---|
| Achilles tendon | Achilles tendinopathy (midportion or insertional) Achilles partial tear Achilles complete tear Paratendinopathy or paratenonitis of Achilles tendon |
| Plantar fascia | Plantar fasciitis Plantar fascia tear Plantar fibromatosis |
| Calcaneus | Stress fracture Osteomyelitis Sever disease Tumor (intraosseous lipoma, simple bone cyst, aneurysmal bone cyst, etc.) |
| Bursae | Retrocalcaneal bursitis Retro-Achilles bursitis Haglund syndrome |
| Nerve | Tarsal tunnel syndrome Baxter neuropathy |
| Heel pad | Heel pad syndrome |
Diagnosis of heel pain can be challenging based only on clinical history and physical examination. Imaging can be useful, with MR imaging the most useful imaging modality. MR imaging has great soft tissue contrast and excellent anatomic detail, which allow for assessment of the location and extent of the hindfoot disorder, which can also assist with preoperative planning. This article discusses the most common conditions that cause heel pain based on their anatomic location and emphasizes their MR imaging appearances.
Heel anatomy
The heel refers to the posterior aspect of the foot, which includes the posterior calcaneus and adjacent soft tissue structures ( Fig. 1 ). It functions to dissipate the compressive forces that occur during gait especially during the stance phase. Together with the metatarsal heads, the heel supports the full weight of the body; thus, it can be subjected to high repetitive forces leading to certain injuries. The heel is comprised of the Achilles tendon, plantar fascia, calcaneus, bursa, nerves in the tarsal tunnel, and inferior heel pad. The Achilles tendon attaches to the calcaneal tuberosity and is the longest and strongest tendon in the body, formed by the gastrocnemius and soleus muscles. The plantar aponeurosis, or plantar fascia, is a thick band of connective tissue that supports the arch of foot. It consists of 3 bands (medial, lateral, and central) and originates from the medial tuberosity of calcaneus and extends anteriorly to insert on the base of the proximal phalanges. A fascial connection exists between the distal Achilles tendon and the posterior aspect of the plantar fascia; thus, forces exerted on the Achilles can affect the plantar fascia. This fascial connection diminishes with age. The calcaneus is the bony foundation of the heel and serves as the attachment site for several structures. The retrocalcaneal and retro-Achilles bursa are located anterior and posterior to the Achilles tendon, respectively, and can become inflamed by various disorders, leading to bursitis. The tarsal tunnel is a fibro-osseous tunnel located at the medial ankle, which is bounded by the flexor retinaculum (roof) and medial surface of talus and calcaneus (floor). It contains the flexor tendons and a neurovascular bundle (posterior tibial artery, vein and tibial nerve). Compression of the regional neural structures may cause numbness, paresthesia, and heel pain. Lastly, a fat pad is present along the inferior aspect of the posterior calcaneus that helps to cushion the weight of the body. Injury or inflammation to this fat pad can lead to heel pain.
Achilles tendon
Disorders of the Achilles tendon are often due to repetitive microtrauma from overuse in athletes or in patients with abnormal alignment, such as flatfeet. The Achilles tendon represents the union of the gastrocnemius and soleus muscles and attaches onto the posterior calcaneus. It lacks a true tendon sheath but is surrounded by thin connective tissue, paratenon. Moreover, there is a critical zone within the tendon representing a segment of the tendon with decreased vascularity, located 2 cm to 7 cm proximal to the calcaneal insertion. Injuries at this location heal poorly due to poor blood flow and tendon ruptures commonly occur in this location.
Terminology used to describe overuse injuries of the Achilles tendon can be confusing and inconsistent. Because there is often no chronic inflammation, the term, tendinosis , should be used instead of tendinitis ; however, both terms refer to the histopathologic appearance of the tendon. Tendinopathy , on the other hand, includes the clinical syndrome of tendon pain, swelling, and impaired performance; thus, it has been suggested as the ideal term to use when describing Achilles tendon injuries. These injuries can be classified into 4 types: midportion tendinopathy, insertional tendinopathy, paratendinopathy, and tendon tear/rupture.
Midportion tendinopathy is the clinical syndrome of pain, swelling, and impaired performance located 2 cm to 7 cm above the calcaneal insertion and manifests as tendon thickening with loss of the normal anterior concave margin on axial images ( Fig. 2 ) and increased intrasubstance signal on edema-sensitive (T2 and short tau inversion recovery [STIR]) sequences. The normal Achilles tendon should be dark on T1 and T2 MR imaging pulse sequences and should measure 5 mm to 8 mm in thickness, depending on the size of the patient. With tendinopathy, tendon contrast enhancement can be present and is consistent with intratendinous neovascularization from the body’s attempt and failure at tendon repair. Occasionally, normal intratendinous high signal intensity can be seen in the Achilles tendon, which can be attributed to magic angle effect related to rotation of the tendon fibers. This artifact can be avoided by using long echo time sequences, such as T2-weighted sequences.
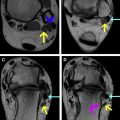
Insertional tendinopathy presents with enthesophyte formation and tendon thickening at the distal calcaneal insertion. Calcifications and ossifications in the distal tendon occur with this condition and can be associated with retrocalcaneal and/or retro-Achilles bursitis. Bone spur and tendon calcifications can be seen on radiographs; and on MR imaging; there is often marrow edema in the calcaneus and distal Achilles tendon substance ( Fig. 3 ). CT aids in surgical planning by detailing the bony anatomy for removal of the posterior spur. Peritendinopathy or peritenonitis of the Achilles tendon refers to acute or chronic inflammation of the thin membrane, peritenon, surrounding the Achilles tendon. It can result from seronegative arthropathy, infection, or overuse injury. On MR imaging, the Achilles tendon can have normal low signal and size; however, there is partially circumferential edema or fluid around the Achilles tendon on fluid-sensitive sequences and enhancement after contrast administration ( Fig. 4 ). Isolated fluid and/or edema in Kager fat pad should be termed, paratendonitis , because the abnormality is adjacent to the tendon and not surrounding it. The potential space between the peritenon and tendon can fill with fluid and exudate, leading to thickening of the peritenon and the patient can present with palpable crepitus.
The Achilles tendon is the most common tendon in the body to rupture and is often seen in middle-aged men engaged in sports activities, such as basketball or tennis. Most tears occur in the avascular zone or midportion of the tendon during an acute traumatic event. Tears can also occur, however, from progression of chronic Achilles tendinopathy, steroid injection, and fluoroquinolone antibiotics. On MR imaging, the presence of fluid within the tendon on fluid-sensitive sequences indicates a tear. There can also be tendon thickening, heterogeneous signal intensity, and disruption of tendon fibers ( Fig. 5 ). When no intact tendon fibers are seen, then a complete tear has occurred. In cases of partial or complete tear, it is crucial to describe the exact location and size of the tendon tear, because treatment options vary depending on the location of the tear. Achilles tendon rupture can occur at the midsubstance (75%), distal insertion (10%–20%), and myotendinous junction (5%–15%). Tears in the tendon midsubstance are typically easier to fix surgically than tears at the myotendinous junction or distal insertion. Moreover, it is important to describe size of the tendon gap and character of the tendon free edge, such as fraying or tapering ( Fig. 6 ). In addition, tears at the myotendinous junction may not been included on the field of view in standard protocols for imaging the ankle; thus, larger sagittal field of view images could be considered in these cases.
Plantar fascia
Plantar Fasciitis
Plantar fasciitis is the most common cause of heel pain and can be due to variety of conditions, including long-distance running, obesity, pes cavus (high arch), pes planus (flat feet), prolonged standing, and arthritidies, such as reactive arthritis (formerly termed Reiter disease) or psoriatic arthritis. Similar to the development of Achilles tendon injury, repetitive trauma can induce microtears in the plantar fascia leading to degeneration and/or inflammatory changes, often in the central cord and at the calcaneal insertion. Patients typically experience pain at the inferior heel that is worse with their initial steps in the morning or after a period of inactivity. The plantar fascia is best seen on coronal and sagittal images MR images and appears as a uniform low signal intensity structure extending from the inferior calcaneal tuberosity to the base of the proximal phalanges measuring 2 mm to 3 mm in thickness. MR imaging findings of plantar fasciitis include thickening of plantar fascia (>4 mm in the craniocaudal dimension), increased intrasubstance signal intensity on T1-weighted and T2-weighted images, and perifascial and bone marrow edema at the calcaneal insertional area ( Fig. 7 ). Occasionally, an inferior calcaneal spur is seen. The association of an inferior calcaneal spur with plantar fasciitis is controversial, however, with some studies indicating no association and other studies indicating a higher association of planter fasciitis with calcaneal spurs. A recent study by Zhou and colleagues finds that there are 2 types of calcaneal spurs. The type A spur extends superior to the plantar fascia insertion whereas a type B spur is enclosed by the plantar fascia and correlates with more severe symptoms. MR imaging can be helpful in these cases by delineating the anatomy of the plantar fascia relative to the spur.
Plantar Fascia Tear
Tear of the plantar fascia can occur from progression of chronic plantar fasciitis or acute sports-related injury in athletes or be related to local corticosteroid injections. Patients are often unable to perform a single-stance heel raise and have plantar ecchymosis. Most plantar fascia tears are located at proximal part of the plantar fascia, near calcaneal insertion, and in the central cord. Similar to tendon rupture, MR imaging can reveal a fluid-filled gap within the disrupted plantar fascia, best seen on fluid-sensitive sequences ( Fig. 8 ). Additional findings include adjacent soft tissue edema, hemorrhage, and injury of the flexor digitorum brevis muscle in acute cases. Fusiform or nodular thickening with low signal intensity on T1-weighted and T2-weighted images can be seen in chronic cases with hypertrophic scar. Delineating the location of the tear and fascial gap on MR imaging is important in surgical planning.
Plantar Fibromatosis
Plantar fibromatosis is a benign but locally aggressive superficial fibroblastic proliferation in the plantar fascia, similar to Dupuytren disease in the hand and desmoid tumors, which involve deeper soft tissue structures. Physical examination often reveals 1 or several palpable nodules along the plantar aspect of foot and can be bilateral in 25% of cases. The nodules can lead to pain, contracture, and even walking disability. Plantar fibromatosis usually involves the central or medial cords of plantar fascia. On MR imaging, plantar fibromatosis typically demonstrates low to intermediate signal intensity on both T1-weighted and T2-weighted images due the dense fibrous content of the nodules ( Fig. 9 ). Occasionally fibromatosis can have high signal intensity on T2-weighted images, if there is a paucity of collagen or fibrous tissue content. Postcontrast MR imaging shows internal, but variable, enhancement in the lesion. Linear regions of enhancement extending from the lesion and along the plantar aponeurosis, called a fascial tail, can be seen and is best seen on postcontrast images. Due to the characteristic appearance of plantar fibromas, MR imaging is helpful in the diagnosis and assessing the anatomic location of the lesions, especially those with deep extension, for surgical removal.