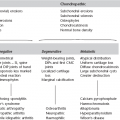
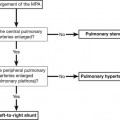
Achondroplasia 1. Decreasing interpedicular distance caudally in the lumbar spine. 2. Short pedicles with a narrow sagittal diameter of the lumbar spinal canal. 4. Anterior vertebral body beak at T12/L1/L2 associated with gibbous deformity once sitting. Gibbous may reverse and develop into hyperlordosis of lumbar spine once walking. Acquired immune deficiency syndrome CXR and CT changes rarely provide definitive diagnosis. 1. Pneumocystis jiroveci – most common opportunistic (fungal) infection. Associated with CD4+ count < 200 cells/µl. With effective chemoprophylaxis and antiretroviral treatment, incidence has fallen. Chest radiographs may be normal at presentation but typically progresses to show bilateral perihilar or diffuse ground-glass opacification and reticulation. Without treatment, there is rapid progression to air-space opacification. Diffuse ground-glass opacification, thickened interlobular septa and consolidation are the key findings on HRCT. Thin-walled cysts are present in ~30%. Less common imaging features include: (a) Asymmetrical upper lobe disease – in patients on prophylactic therapy; may be confused with tuberculosis. (b) Miliary nodules or solitary nodule (may cavitate). 2. Mycobacterium tuberculosis – an important infection in HIV-positive patients, and diagnosis is difficult. Imaging features depend on severity of immune compromise: depressed but near-normal CD4+ levels are associated with similar radiological features to non-immunocompromised patients (upper lobe nodules ± cavitation). With more severe depression, more atypical patterns (non-upper lobe predilection; lower propensity for cavitation) and disseminated infection are likely. 1. Kaposi’s sarcoma – decreasing incidence with advent of HAART. Lung involvement is less common than cutaneous and/or visceral disease. Perihilar bronchocentric nodules/masses are the typical radiological findings – ‘flame-shaped’ opacities may be seen on CT. 2. Pulmonary lymphoma – increasingly common: non-Hodgkin’s more common than Hodgkin’s. 1. Non-specific interstitial pneumonia – variable prevalence. Clinical presentation and radiological features may mirror those seen in patients with Pneumocystis carinii pneumonia (PCP) but CD4+ counts tend to be higher in patients with NSIP. 2. Lymphoid interstitial pneumonia – most common in children and associated with EBV infection. Non-specific radiological appearances (ground-glass opacities, small nodules, bronchiectasis. 3. Obliterative bronchiolitis – in adolescents with vertically transmitted infection. 1. Primary HIV – oesophageal ulceration. 2. Candida – usually oropharynx and oesophagus. AIDS defining. Mucosal plaques, fold thickening, ‘shaggy’ oesophagus on barium swallow. 3. Herpes – small discrete ulcers on barium swallow. 4. CMV – most common gastrointestinal infection. Can occur anywhere but usually lower gastrointestinal tract. Oesophagus – large mid-oesophageal ulcer; CMV gastritis, enteritis and colitis – superficial progressing to deep ulceration (mimic Crohn’s), extensive bowel wall thickening on CT, US; segmental or diffuse, lymphadenopathy not prominent. 5. TB – ileocaecal jejunoileum most common sites (upper gastrointestinal tract less common). Segmental ulcers, wall thickening, strictures, and mass-like lesions of the caecum and terminal ileum. Regional low-attenuation necrotic lymphadenopathy. Hepatosplenomegaly (occasional focal lesions). 6. Chlamydia trachomatis – causes lymphogranuloma venereum. Generally in men who have sex with men as a HIV coinfection. Introduced anally and causes a proctocolitis. May have inguinal lymphadenopathy and collections. 7. Mycobacterium avium complex – usually small bowel. Mimics Whipple’s (irregular fold thickening and mild dilatation). Prominent lymphadenopathy. Hepatosplenomegaly (occasional focal lesions). 8. Cryptosporidium – diffuse fold thickening, flocculation of barium (mimics sprue). No lymphadenopathy. 9. Rochalimaea henselae (peliosis hepatis) – fever, sweats, right upper quadrant pain. Sonographically liver inhomogeneous, with hyperechoic and hypoechoic regions. Cavities may be visible on CT (if large). 10. PCP – liver/spleen/kidneys – hypoechoic/hypoattenuating masses or multiple tiny echogenic/hyperattenuating foci (calcified). 1. Kaposi’s sarcoma – CD4 count typically < 200 (a) Liver/spleen – multifocal hyperechoic nodules (5–12 mm) adjacent to portal veins on US scan. CT – hypoattenuating nodules, with delayed enhancement (mimic haemangiomas). (b) Gastrointestinal tract – usually with cutaneous involvement. Anywhere in gastrointestinal tract but duodenum most common. Submucosal masses (0.5–3 cm) ± ulceration at CT/barium. Hyperattenuating lymphadenopathy. 2. Lymphoma – usually aggressive form of non-Hodgkin’s lymphoma. Peripheral nodes are present in 50% and extranodal involvement is common, particularly bowel, viscera and marrow. 1. Dysphagia – common. Usually due to candidiasis, but occasionally caused by viral oesophagitis or Kaposi’s sarcoma. 2. Hepatosplenomegaly – non-specific. Seen in many infections (CMV, TB, MAI) and lymphoma. 3. Diarrhoea – common. Usually CMV colitis if mild, or Cryptosporidium (protozoa) if severe. Giardia, Clostridium difficile and Mycobacterium may also occur. 4. Retroperitoneal/mesenteric lymphadenopathy (a) Progressive generalized lymphadenopathy syndrome – i.e. two or more extrainguinal nodes persisting for > 3 months with no obvious cause. Biopsy reveals benign hyperplasia, and CT shows clusters of small nodes < 1 cm in diameter in the mesentery and retroperitoneum. 5. AIDS cholangiopathy – right upper quadrant pain, nausea, vomiting and fever. Due to infection by CMV or Cryptosporidium. Gallbladder wall thickening, pericholecystic fluid, intrahepatic and extrahepatic bile duct strictures, diverticula, intraluminal filling defects and strictures of the juxta-ampullary pancreatic duct. 6. HIV nephropathy – proteinuria and rapidly progressive renal failure. Usually, globally enlarged kidneys. Boiselle, P. M., Crans, S. A., Jr., Kaplan, M. A. The changing face of Pneumocystis carinii pneumonia in AIDS patients. AJR Am J Roentgenol. 1999; 172:1301–1309. Burns, J., Shaknovich, R., Lau, J., et al. Oncogenic viruses in AIDS: mechanisms of disease and intrathoracic manifestations. AJR Am J Roentgenol. 2007; 189:1082–1087. Ferrand, R. A., Desai, S. R., Hopkins, C., et al. Chronic lung disease in adolescents with delayed diagnosis of vertically-acquired HIV infection. Clin Infect Dis. 2012; 55:145–152. Guihot, A., Couderc, L. J., Rivaud, E., et al. Thoracic radiographic and CT findings of multicentric Castleman disease in HIV-infected patients. J Thorac Imaging. 2007; 22:207–211. Kuhlman, J. E. Imaging pulmonary disease in AIDS: state of the art. Eur Radiol. 1999; 9:395–408. Logan, P. M., Finnegan, M. M. Pictorial review: pulmonary complications in AIDS: CT appearances. Clin Radiol. 1998; 53:567–573. Major, N. M., Tehranzadeh, J. Musculoskeletal manifestations of AIDS. Radiol Clin North Am. 1997; 35:1167–1190. Provenzale, J. M., Jinkins, J. R. Brain and spine imaging findings in AIDS patients. Radiol Clin North Am. 1997; 35:1127–1166. Redvanly, R. D., Silverstein, J. E. Intra-abdominal manifestations of AIDS. Radiol Clin North Am. 1997; 35:1083–1126. Reeders, J. W., Goodman, P. C., 2001. Radiology of AIDS. Springer, Heidelberg. Reeders, J. W., Yee, J., Gore, R. M., et al. Gastrointestinal infection in the immunocompromised (AIDS) patient. Eur Radiol. 2004; 14(Suppl 3):E84–E102. Restrepo, C., Lemos, D., Gordillo, H. Imaging findings in musculoskeletal complications of AIDS. Radiographics. 2004; 24:1029–1049. Restrepo, C. S., Ocazionez, D. Kaposi’s sarcoma: imaging overview. Semin Ultrasound CT MR. 2011; 32(5):456–469. Richards, P. J., Armstrong, P., Parkin, J. M., et al. Chest imaging in AIDS. Clin Radiol. 1998; 53:554–566. Spencer, S. P., Power, N., Reznek, R. H. Multidetector computed tomography of the acute abdomen in the immunocompromised host: a pictorial review. Curr Probl Diagn Radiol. 2009; 38(4):145–155. Acquired immune deficiency syndrome (AIDS) in children AIDS in children differs from AIDS in adults in the following ways: 2. Children are more likely to have serious bacterial infections or CMV. 3. They develop pulmonary lymphoid hyperplasia (PLH)/lymphocytic interstitial pneumonia (LIP), which is rare in adults. 4. They almost never develop Kaposi’s sarcoma. 5. They are less likely to be infected with Toxoplasma, Mycobacterium tuberculosis, Cryptococcus and Histoplasma. 6. Two patterns of presentation and progression can be recognized: (a) In the first year of life with serious infections and encephalopathy. Poor prognosis. (b) Preschool and school age with bacterial infections and lymphoid tissue hyperplasia. Survival is longer, to adolescence. Prognostic factors are severity of disease in the mother, age of onset and severity at onset. 1. PCP – may be localized initially but typically there is rapid progression to generalized lung shadowing, which is a mixed alveolar and interstitial infiltrate. 50% of infections occur at age 3–6 months. Two-thirds of infections are the first and only infective episode. 3. LIP/PLH – in 50% of patients. Insidious onset of clinical symptoms. CXR shows a diffuse, symmetrical reticulonodular or nodular pattern (2–3 mm in diameter) which is most easily seen at the bases and periphery of the lungs ± hilar or mediastinal lymphadenopathy. The nodules consist of collections of lymphocytes and plasma cells without any organisms. Children with LIP are more likely to have generalized lymphadenopathy, salivary gland enlargement (particularly parotid) and finger clubbing than those with CXR changes due to opportunistic infection, and the prognosis for LIP is better. Long-standing LIP may be complicated by lower lobe bronchiectasis or cystic lung disease (resembling that seen in histiocytosis). 4. Mediastinal or hilar adenopathy may be secondary to PLH, M. tuberculosis, MAI, CMV, lymphoma or fungal infection. 5. Cardiomyopathy, dysrhythmias and unexpected cardiac arrest. 1. Hepatosplenomegaly – due to chronic active hepatitis, hepatitis A or B, CMV, EBV and M. tuberculosis, generalized sepsis, tumour (fibrosarcoma of the liver) or congestive cardiac failure. 2. Oesophagitis – Candida, CMV or herpes simplex. 3. Chronic diarrhoea – in 40–60% of children. Infectious agents are only infrequently found but include Candida, CMV and Cryptosporidium. Radiological findings are non-specific and include a malabsorption-type pattern with thickening of bowel wall and mucosal folds and dilatation. Fine ulceration may be seen. 5. Mesenteric, para-aortic and retroperitoneal lymphadenopathy – due to MAI, lymphocytic proliferation (lymph-node syndrome), non-Hodgkin’s lymphoma or Kaposi’s sarcoma (rare in childhood). 6. HIV nephropathy – children may present with proteinuria, fluid and electrolyte imbalances and/or acute or chronic renal failure. US shows enlarged echogenic kidneys and CT shows enlarged pyramids. Simple cysts may be present. 7. UTI – in up to 50% of AIDS patients. May be due to common organisms or unusual agents, e.g. CMV, Cryptococcus, Candida, Aspergillus, Mycobacterium and Pneumocystis. 1. HIV encephalopathy is divided into two types: (a) Progressive encephalopathy comparable to adult AIDS dementia complex. There is step-wise deterioration of mental status and higher functions. It is associated with severe immune deficiency. (b) Static encephalopathy, associated with better higher functions but failure to reach appropriate milestones. (a) Cerebral atrophy – worse with progressive encephalopathy. (b) Non-enhancing white matter of ↓ attenuation (CT) or ↑ T2W signal (MRI) in the frontal lobes, periventricular regions and centrum semiovale. 2. Intracranial calcifications – in up to 33% of HIV-infected children. Usually bilateral and symmetrical and most commonly seen in the globus pallidus and putamen; less commonly in the subcortical frontal white matter and cerebellum. Usually not seen before 10 months of age; early calcifications are more likely because of congenital infections. 3. Malignancy – most commonly high-grade B-cell lymphoma associated with EBV infection. (a) Progressive multifocal leucoencephalopathy – difficult to distinguish from HIV encephalopathy, but tends to be more focal, asymmetrical and commoner in the posterior parietal lobe. (b) Toxoplasmosis – enhancing mass lesions with surrounding oedema in the basal ganglia and corticomedullary junction of the periventricular white matter. (c) Meningitis – due to fungi, Mycobacteria spp. and Nocardia, in addition to the more usual causes of meningitis. Haller, J. O. AIDS-related malignancies in pediatrics. Radiol Clin North Am. 1997; 35(6):1517–1538. Haller, J. O., Cohen, H. L. Pediatric HIV infection: an imaging update. Pediatr Radiol. 1994; 24:224–230. Martinoli, C., Pretolesi, F., Del Bono, V., et al. Benign lymphoepithelial parotid lesions in HIV-positive patients: spectrum of findings at gray-scale and Doppler sonography. AJR Am J Roentgenol. 1995; 165(4):975–979. Miller, C. R. Pediatric aspects of AIDS. Radiol Clin North Am. 1997; 35:1191–1222. Safriel, Y. I., Haller, J. O., Lefton, D. R., et al. Imaging of the brain in the HIV-positive child. Pediatr Radiol. 2000; 30:725–732. Stoane, J. M., Haller, J. O., Orentlicher, R. J. The gastrointestinal manifestations of pediatric AIDS. Radiol Clin North Am. 1996; 34(4):779–790. Zinn, H. L., Haller, J. O. Renal manifestations of AIDS in children. Pediatr Radiol. 1999; 29:558–561. Acromegaly The effect of excessive growth hormone on the mature skeleton. 1. Increased width of bones but unaltered cortical thickness. 2. Tufting of the terminal phalanges, giving an ‘arrowhead’ appearance. 3. Prominent muscle attachments. 4. Widened joint spaces – especially the metacarpophalangeal joints: due to cartilage hypertrophy. 6. Increased heel pad thickness (> 21.5 mm in female; > 23 mm in male). Alkaptonuria Aneurysmal bone cyst 1. Age – 10–30 years (75% occur before epiphyseal closure). 2. Sites – ends of long bones (70–80%), especially in the lower limbs. Also flat bones and vertebral appendages. (a) Arises in unfused metaphysis or in metaphysis and epiphysis after fusion. (b) Well-defined lucency with thin but intact cortex. (c) Marked expansion (ballooning). (d) Thin internal strands of bone/trabeculation. (e) ± New bone in the angle between original cortex and the expanded part. (f) Fluid–fluid level(s) on CT and MRI. (g) In the spine they involve the posterior elements. (h) May rarely arise from the surface of bone in a subperiosteal location. Ankylosing spondylitis 1. Involved initially in 70–80%. Initial changes in the sacroiliac joints followed by the thoracolumbar and lumbosacral regions. The entire spine may be involved eventually. 2. The radiological changes in the sacroiliac joints (see 3.12) are present at the time of the earliest spinal changes. MRI most sensitive technique for early disease and all changes except syndesmophytes. 3. Spondylitis – anterior and posterior erosion of vertebral end-plates (Romanus). Enthesitis of annulus fibrosis. Then sclerosis causing ‘shiny corner’ (osteitis). 4. Discovertebral – inflammatory involvement of intervertebral disc (Andersson). 5. Syndesmophytes – bony outgrowths from vertebral margins. 6. Squaring of vertebrae – due to bone proliferation. 7. Arthritis – facet, costovertebral and costotransverse joints (synovitis, erosion, ankylosis). 8. Enthesitis – interspinous ligaments with osteitis. 9. Ankylosis – fusion of spine from 5–7 plus bony extension through 4. Leads to ‘bamboo spine’. 10. Fracture – insufficiency in ankylosed spine (especially cervicothoracic and thoracolumbar junctions). 11. Osteoporosis – with long-standing disease. 13. Arachnoiditis – rare and late. Arachnoid diverticulae, laminar erosions, dural calcification. 1. Hip – axial migration, concentric joint-space narrowing, cuff-like femoral osteophytes, acetabular protrusion. Symptoms may be dominant, leading to flexion contracture and ankylosis. 2. Shoulder – narrowing of glenohumeral and acromioclavicular joints. Hatchet erosion at greater tuberosity. 3. Knee – tricompartment narrowing and erosion. 4. Hand and foot – asymmetric involvement; small erosion and osseous proliferation. Jang, J. H., Ward, M. M., Rucker, A. N., et al. Ankylosing spondylitis: patterns of radiographic involvement – a re-examination of accepted principles in a cohort of 769 patients. Radiology. 2011; 258(1):192–198. Lambert, R. G., Dhillon, S. S., Jaremko, J. L. Advanced imaging of the axial skeleton in spondyloarthropathy: techniques, interpretation, and utility. Semin Musculoskelet Radiol. 2012; 16(5):389–400. Asbestos inhalation 1. Pleural plaques – commonest manifestation of asbestos exposure developing 20–30 years after exposure. Typically seen on parietal pleural on undersurface of ribs, diaphragmatic pleura and adjacent to spine; virtually pathognomonic. Sharply angulated, ‘holly-leaf’ opacities on chest radiography and sharply demarcated. Discrete ‘punched-out’ appearance at CT. 2. Benign pleural effusion – most common ‘early’ (< 10 years) manifestation; occurs in < 10%. Exudative fluid. May be unilateral or bilateral and may be followed by residual benign diffuse pleural thickening in around 50% or regions of rounded atelectasis (‘folded lung’). 3. Diffuse pleural thickening – less specific for asbestos exposure than plaques. 4. Rounded atelectasis – (folded lung, Blesovsky syndrome). Rounded mass, adjacent pleural thickening and parenchymal bands/distortion (‘comet tail’ appearance). Can be seen with other exudative effusions. 5. Malignant pleural mesothelioma – long latency (30–40 years). Lobulated pleural thickening involving mediastinal pleura ± large pleural effusion but minimal mediastinal shift. (NB. Can occur in peritoneum.) 1. Asbestosis – long latency (30–40 years). Crocidolite most fibrogenic, chrysotile least. Histological and radiological appearances almost identical to those seen in patients with cryptogenic fibrosing alveolitis/idiopathic pulmonary fibrosis. 2. Lung cancer – increased incidence even in the absence of a smoking history or asbestosis. Calcium pyrophosphate dihydrate deposition disease 1. Three manifestations which occur singly or in combination: (a) Cartilage calcification (chondrocalcinosis). (b) Crystal-induced acute synovitis (pseudogout) (c) Structural joint abnormalities (pyrophosphate arthropathy). 2. Associated conditions are hyperparathyroidism and haemochromatosis (definite) and gout, Wilson’s disease and alkaptonuria (less definite). 3. Chondrocalcinosis involves:
Alphabetical list of conditions
Axial skeleton
A Chest
Opportunistic infections
Neoplasms
Other parenchymal lung diseases
B Abdomen
Infections
Malignancy
Common symptoms/signs
Chest
Abdomen
Head
Appendicular skeleton

Axial skeleton
Appendicular skeleton
Extraskeletal
Pleura
Lung parenchyma
Alphabetical list of conditions