Hippocrates is credited with performing the first phlebotomy to treat a varix circa 400 BC. 1 However, the surgical treatment of varicose veins was first described in detail by Aulus Cornelius Celsus (25 BC to 50 CE) in his medical text entitled De Medicina, which has been available since at least the Roman times. Through modification of technique and refinement of the available surgical tools, Swiss dermatologist Robert Muller reinvented the technique around 1956, and he has been referred to as “the father of modern day ambulatory phlebectomy.” 2 Since the introduction of Muller’s technique, there has been a natural evolution of ambulatory phlebectomy (AP), but the core principles in providing an efficient, minimally invasive, and economical procedure for varicose veins still hold true.
AP is a minor, outpatient surgical technique that removes dilated superficial varicose veins. The procedure is typically conducted on an ambulatory basis in all except the most severe cases. With the aid of local anesthesia, multiple microincisions allow for the complete removal of incompetent veins by hook avulsion, resulting in long-term success rates greater than 90%. 3, 4 The procedure is generally well tolerated and complications are rare. Microsurgical phlebectomy, microphlebectomy, stab avulsion, and microextraction are synonymous with AP.
Exclusively performed with local anesthesia, AP leads to reduced surgical risks compared with traditional surgical venous ligation. The latter of the two leads to relatively high recurrence rates given that the vein is interrupted rather than removed. 5, 6 Venous ligation has therefore fallen out of favor. In comparison, the problematic vein(s) is/are extracted with AP. The small size of the skin incision or puncture usually results in little or no scarring, typically producing good cosmetic results. AP may also be performed in conjunction with endovenous thermal ablation (EVTA) to provide the best available care in appropriately selected patients.
8.2 Indications
The main indication for AP is symptomatic varicose veins not responding to conservative treatment options such as compression therapy. Superficial varicose veins near the skin surface are often too large to treat with sclerotherapy and too tortuous to treat with EVTA, making AP the optimal approach. AP may be used for the cosmetic aspect of treating asymptomatic varicose veins to treating complications of varices, such as recurrent superficial thrombophlebitis and bleeding. 7, 8 AP for the treatment of small segments of superficial thrombophlebitis is readily performed. AP is effective in this setting as the involved vein segment as well as the intravascular coagulum can be extracted through the same incision. With experience, AP need not be exclusive to lower extremity varicose veins and is successfully performed on facial veins such as small periorbital or temporal veins. 9 Alternative indications for AP include vein biopsy and drug implant extraction. 10, 11
AP in the lower extremities permits removal of primary or secondary branch incompetent varicosities of the great saphenous vein (GSV) or small saphenous vein (SSV). The major tributary branch vessels of the GSV or SSV to be removed may include the anterior thigh circumflex vein, the posterior thigh circumflex vein, or anterior accessory GSV, particularly if they exhibit marked tortuosity. Additional varicose veins appropriate for AP include pudendal and labial veins of the groin. Perforators and dilated reticular veins may also be addressed. 12, 13
Dilated reticular veins around and below the knee, lateral thigh and leg, ankle, and venous network about the dorsum of the foot are less common indications for AP. Small reticular veins supplying or associated with telangiectasias, particularly about the foot and ankle, are less frequent indications for AP, but can be performed with success. A retrospective review of 75 patients who underwent AP of the foot demonstrated satisfactory results with few complications 14 ( ▶ Table 8.1).
Indications | Contraindictions | |
Absolute | Relative | |
Asymptomatic varicose and reticular veins | Infectious dermatitis or cellulitis of area to be treated | Deep venous thrombosis |
Symptomatic varicose and reticular veins | Severe peripheral edema | Nonambulatory patient |
Complications of varicose veins | Seriously ill patients | Hypercoagulable state |
Severe allergy to local anesthetic | Anticoagulated patient | |
Liver dysfuncton | ||
Pregnant or nursing | ||
With experience, foam sclerotherapy (Chapter ▶ 7) can satisfactorily treat large tortuous varicosities of the lower extremities, similar to AP. A determining factor in performing AP versus foam sclerotherapy for some practitioners includes assessment of the overall thickness of the venous wall. Thin-walled veins are typically better treated with foam sclerotherapy, whereas thicker-walled veins are generally reserved for AP. 15 Recurrence of varicose veins is significantly lower with AP when compared with sclerotherapy, as evidenced by a randomized controlled trial for the treatment of lateral accessory varicose veins comparing these two techniques. Two-year follow-up demonstrated a 2.1% recurrence rate with AP versus 37.5% for sclerotherapy. 16 Thrombophlebitis is also more common following sclerotherapy than AP.
Veins that may not be appropriate for AP include the GSV and SSV themselves as well as the saphenofemoral and saphenopopliteal junctions. These larger, deeper venous structures are below the superficial fascia and should not be addressed by AP. In such cases, EVTA with either radiofrequency or laser energy is indicated. It is quite commonplace to treat reflux of the saphenous system with EVTA, followed by AP of the remaining varicose branches in the same setting or at a follow-up procedure.
8.3 Contraindications
AP is contraindicated in cases of infectious dermatitis or cellulitis involving the area to be treated, as well as in severe peripheral edema or lymphedema. Patients who are seriously ill (e.g., severe cardiovascular or pulmonary problems), very elderly, or are unable to follow postoperative instructions should not be treated with AP. Patients on anticoagulation, uncorrectable coagulopathy, or hypercoagulable states pose a relative contraindication to AP. Other relative contraindications include patients who rely on the superficial venous system for drainage due to an occlusion of their deep venous system. Patients who are not able to ambulate postprocedure or those with severe peripheral arterial disease, preventing them from wearing compression stockings, are also not ideal candidates. An allergy to local anesthesia or compromised liver function limiting the metabolism of the local anesthetic may pose relative contraindications. As tolerated, pregnant or nursing patients should have care of their varicose veins delayed to a later date ( ▶ Table 8.1).
8.4 Technique
8.4.1 Preprocedure
Procedure facilities, whether in a hospital or clinic setting, should have good lighting, a procedural table permitting Trendelenburg’s position, and resuscitation equipment. Although allergic and toxic reactions are exceedingly rare, appropriate resuscitation capabilities should be available including intravenous fluid, epinephrine, diazepam, antihistamines, injectable steroids, and an automatic external defibrillator. A nurse or assistant should be present but direct intraoperative support is seldom necessary.
With the patient in the standing position, all varicose veins to be treated with AP should be identified, as it may be difficult or near impossible once in the recumbent position. A surgical permanent marker should be used to avoid washing away of the identifying marks during preparation of the site ( ▶ Fig. 8.1). Care should be taken during time of actual incision to avoid the marked areas, as a permanent tattoo may develop if the incisions were placed directly through the markings. Transillumination may also be used to accurately locate the vein(s) to be treated, enabling their removal with an overall reduction in size and number of incisions, as well as a decrease in operating time. 17, 18

Fig. 8.1 All varicose veins are marked with the patient in the standing position given that they may be difficult or impossible to identify during recumbency. A permanent surgical marking is placed adjacent to the varicose vein to prevent washing away during preparation of the surgical site and to avoid accidently making an incision directly over the varicose vein itself. The microincisions should also not be made directly over the markings to avoid tattooing.
Generally, premedication should be avoided and is rarely indicated because the best means of preventing potential vascular complications is postoperative walking. Postoperative walking could be hindered in patients taking sedatives or anxiolytics. 19 Commonly, a large volume of low-concentration lidocaine known as tumescent anesthesia 20 should be instilled around the vein. Mixture concentrations range from 0.01 to 0.1% of lidocaine, at a dose of 4 mg/kg up to 7 mg/kg with the addition of epinephrine. Epinephrine, at a concentration of 1:1,000,000, is frequently added to the solution because it slows down the absorption of lidocaine and it causes vasoconstriction of the superficial skin capillaries, minimizing postoperative bleeding. However, potential risks of adding epinephrine include tachycardia and skin necrosis. The addition of a buffer such as sodium bicarbonate to the acidic tumescent solution may neutralize the pH, making the infiltration less painful. The solution can be infused locally, using a series of large syringes, a pressurized bag, or a peristaltic pump. The use of tumescent anesthesia decreases patient discomfort during and after the procedure, and can contribute to predissection of the vein from the surrounding tissue, thereby elevating it to the skin surface and allowing for easier hook extraction. 21
The procedure requires only a few surgical instruments. An 18-gauge cutting needle, an 11 blade scalpel, or a 15-degree ophthalmic blade may be used for the microincisions. Varying by size and shape, there are several commercially available vein hooks. The commonly used Muller’s hooks of today are in fact an evolution of the broken half of a hemostat. 2 The modern-day Muller’s hook is a blunt-tipped instrument resembling a crochet hook. The Oesch’s hook is designed with a small barb at the tip, and is characterized by a large square handle, available in three sizes. The Ramelet’s hook has a small fine hook with a distinct cylindrical shaft, also available in two sizes. Several other hooks serving a similar purpose include the Dortu, Varady, Vergereau, Martimbeau, and Trauchessec. Multiple clamps are required for AP. These clamps help maintain a firm grip on the extracted vein and should have fine serrated tips. Mosquito forceps can also be used to grasp veins as they are extracted. Surgical scissors and a spatula should readily be available.
8.4.2 Intraoperative
After the patient is placed on the procedural table, with the area to be treated prepped in a sterile fashion, tumescent anesthesia is injected into the perivenous tissue with care in avoiding the preprocedure markings. Cutaneous microincisions or punctures are made near the superficial varicose veins adjacent to the skin markings. The microincisions should be vertically oriented along the thigh, lower leg, and foot, while around the knee or ankle the incision should follow normal Langer’s tension lines for a better cosmetic result. Care should be taken around the popliteal fold, the prepatellar, and pretibial region, as well as about the dorsum of the foot. These regions contain veins that may be more difficult to avulse and are therefore more susceptible to injury, such as a superficial hematoma about the popliteal fold. 22 The incisions themselves vary between 1 and 3 mm in size and can be separated from one another by 2 to 15 cm, dependent on the size and length of the vein, presence of perforators, and experience of the proceduralist.
Once the microincision has been made, the hook is inserted with the intention of undermining the varicose vein along its course via gentle dissection. The hook should then move in a perpendicular direction and rotated against the index vein. If there is difficulty in removing the vein from its perivenous fibroadipose attachments, a blunt dissector or spatula may be used. Once free, the vein can be brought out of the microincision with the hook ( ▶ Fig. 8.2). The liberated vein should then be grasped with either mosquito forceps or clamps outside of the microincision ( ▶ Fig. 8.3). Gentle traction on the vein allows the operator to remove short segments and may permit visualization of its entire course. Periodically, the clamps should be repositioned as the avulsed segments get longer and longer. At any time, the vein may be grasped between two clamps and cut with surgical scissors to facilitate removal. Through repetition, the entire varicose vein or a segment of it is progressively extracted from one microincision to the next. Hemostasis is achieved during the procedure by applying light compression with sterile gauze.
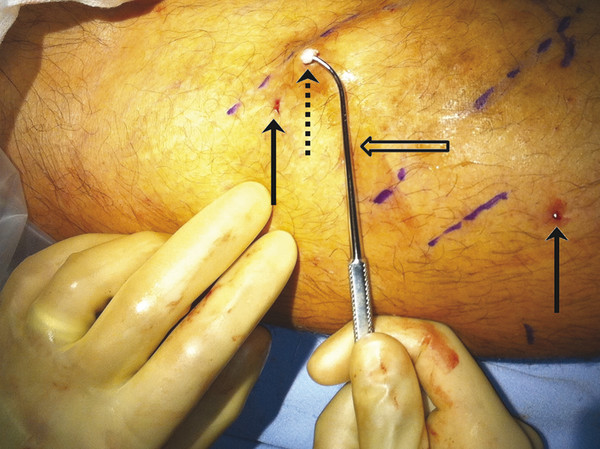
Fig. 8.2 Through the microincision (solid arrow), the phlebectomy hook (open arrow) is inserted along the course of the varicose vein (dashed arrow). After gentle dissection, the hook is rotated in a perpendicular direction. Once free, the vein can be brought out of the microincision with the hook. Note the size of the microincisions, approximately 1 to 3 mm in length, and the distance of the microincisions from the marked areas to avoid tattooing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree