The Society for Interventional Radiology, Cardiovascular Interventional Radiological Society of Europe, American College of Phlebology, Canadian Interventional Radiology Association, the Society for Vascular Surgery, and the American Venous Forum have developed quality improvement and clinical practice guidelines which recommend a complete history and a detailed physical examination for patients with varicose veins or chronic venous disease (CVD). 1, 2, 3 The initial clinical evaluation is an essential assessment that helps guide the management of patients with venous insufficiency. As a health care practitioner, it is important to provide a thorough examination keeping in mind that some patients referred for venous insufficiency may also suffer from other medical conditions that share similar clinical manifestations. In these situations, proper recognition of other conditions is necessary to direct the patient toward appropriate medical care. For those with venous insufficiency, the clinical exam will help the practitioner select the type of treatment and manage patient expectations appropriately. The postoperative evaluation is equally as important and used to determine if there has been improvement in symptoms or appearance of the legs, gauge patient satisfaction, and look for procedure-related complications. Both the pre- and postoperative assessments require a methodical, organized examination.
The proper function of the venous system of the lower extremities relies on one-way valves located at intervals along the course of the vessels keeping the direction of blood flow toward the heart. When these valves fail, blood is allowed to flow in a retrograde direction, commonly described as venous reflux. As a consequence, venous hypertension develops in the territory drained by the vessel. CVD is the clinical entity that results from chronic venous hypertension. 4, 5
Chronic venous insufficiency is a heterogeneous medical condition associated with a wide clinical spectrum, ranging from simple cosmetic issues to severe and limiting symptoms including venous ulcerations. The incidence increases with age, is higher in women than men, and worsens with pregnancy. 1, 2, 3, 4, 5, 6, 7, 8 The lower extremity venous system consists of a network of superficial and deep veins interconnected by perforator veins, and the severity of signs and symptoms correlates with the extension of venous insufficiency within the system. 7
The majority of patients presenting with venous insufficiency have idiopathic disease of the vein wall, with subsequent valvular incompetence in the superficial veins leading to venous reflux (superficial venous insufficiency) and development of varicose veins. 1, 2, 3, 4 Most cases of deep venous insufficiency have a nonthrombotic (primary) or postthrombotic (secondary) etiology. 7 It is estimated that 23% of adults have varicose veins in the United States, and 6% present with more advanced CVD with skin changes, edema, or ulcerations. 1 Varicosities can be considered a cosmetic problem with variable impact in the lifestyle of patients. However, varicose veins are a common cause of discomfort, pain, disability, and deterioration of quality of life. 1
Symptoms related to varicose veins can be variable. Some patients may present with no symptoms, only concerned about the cosmetic appearance of the visible veins. Symptoms related to varicose veins include aching, pain, burning sensation, tingling, throbbing, heaviness, tiredness and fatigue, itching skin, muscle cramps, swelling, and restless legs. Although not specific, these symptoms suggest CVD, particularly if they are more significant by the end of the day and are relieved by resting, elevation of the legs, or use of compression stockings. 1
The clinical exam is composed of a thorough medical history, physical examination, photographic documentation of visible findings, classification into the CEAP (clinical, etiology, anatomy, pathophysiology) system, assignment of a venous clinical severity score (VCSS), and determination of treatment options and clinical follow-up. Each part is described in detail in this chapter.
3.2 Medical History
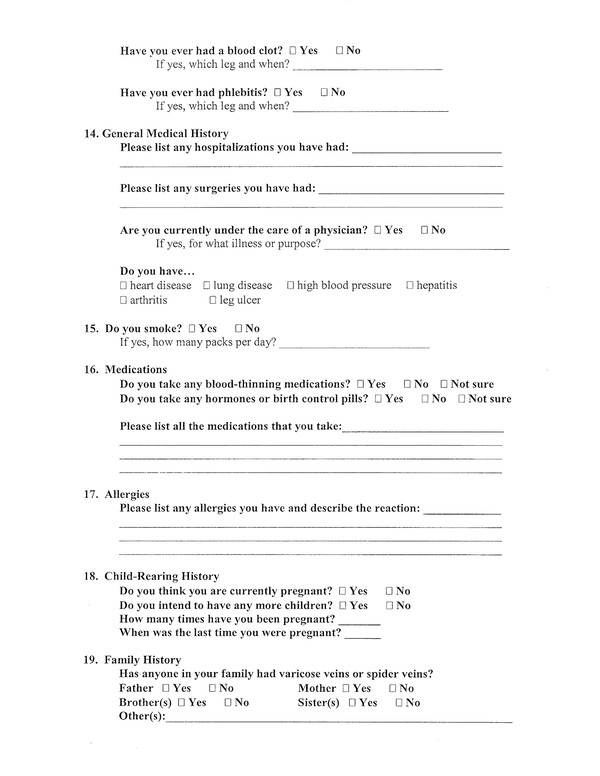
The patient history is necessary to establish the etiology of venous insufficiency, as well as gauge the severity of the disease and the impact on the patient’s quality of life. The latter two will help assess procedure outcomes. The patient history should be thorough and efficient. An efficient way to help obtain thorough histories is to have a clinical questionnaire pertaining to venous insufficiency in the office ( ▶ Fig. 3.1) to be completed by the patient prior to the consult. Alternatively, the questionnaire can be mailed or e-mailed to the patient in advance. The following sections should be present on the questionnaire: chief complaint, history of present illness, past medical and surgical history, allergies, current medications, social history, and family history. Pay particular attention to the risk factors in the history that will make venous disease more likely: older age, female gender, family history of venous insufficiency, obesity, occupation requiring prolonged standing or sitting, pregnancy, and previous deep venous thrombosis (DVT). Also pay attention to risk factors that would make another diagnosis more likely, such as peripheral arterial disease, lymphatic or deep venous obstruction, pelvic congestion syndrome, trauma, vasculitis, or infection.
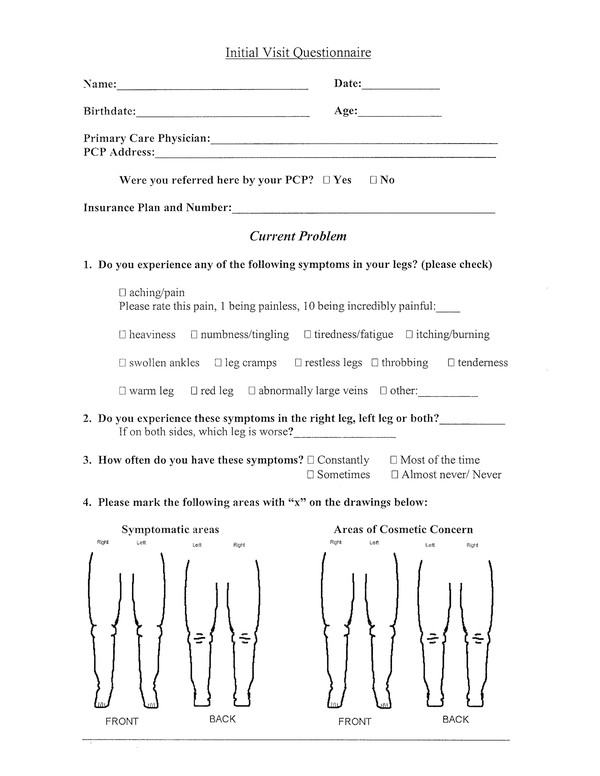
Fig. 3.1 Patient self-assessment questionnaire.
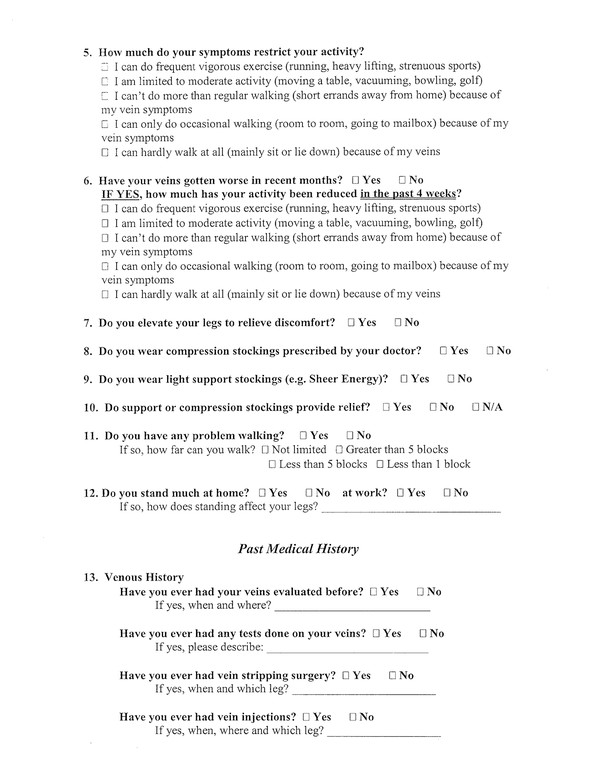
(continued)
(continued)
3.2.1 History of Present Illness
Using the diagram of the legs in the questionnaire ( ▶ Fig. 3.1), have the patient mark the area(s) of concern on the front and back of the legs. The patient should specify the type of discomfort (heaviness, numbness/tingling, itching, burning, cramps, throbbing, tenderness, warmth, restlessness, etc.) and indicate the presence of visible findings such as redness, rash, skin discoloration, bulging veins, spider veins, swelling, or ulceration. The severity of each concern can be provided on a scale of 1 to 10. If it is a cosmetic concern, they should state what type and the location in the lower extremities.
These specific questions regarding the patient’s symptoms are particularly useful:
When does the pain occur? It is expected that pain related to venous insufficiency will occur after standing or sitting for long periods of time, and get worse throughout the day. If the pain is worse in the morning or when lying down, this should draw attention toward other etiologies. For example, rheumatoid arthritis affecting joints in the lower extremity may be painful in the morning, but improve throughout the day. 1 If there is pain or discomfort when lying down or at night, then consider restless leg syndrome, but be aware that there is an association between venous insufficiency and restless leg syndrome. Improvement of symptoms in these patients has been reported after the venous insufficiency has been successfully treated. 9 Whether the symptoms are constant or intermittent may depend on the intensity of physical activity during the day. The pain associated with venous insufficiency is expected to improve when the patient’s legs are elevated and worsen with prolonged standing. 7, 8
Do the patient’s symptoms restrict his or her daily activities? If yes, and to a great extent, then consider that the patient may be experiencing claudication related to arterial insufficiency and peripheral vascular disease. Venous claudication (pain during and after exercise that is relieved with rest and leg elevation) can also be caused by venous outflow obstruction related to DVT or iliac vein stenosis (May–Thurner syndrome). 1
Have the symptoms been getting worse? Venous disease is expected to get worse over a period of months to years. If the symptoms started suddenly or are progressing rapidly, then other etiologies must also be considered.
Has anything been done to improve the pain? Usually, the patient has tried leg elevation and maybe even compression stockings. If the patient has used compression stockings, then identify how often they have been worn and which type (over-the-counter vs. prescription). If prescription, check to see whether the graded compression of the stocking was appropriate for the patient’s symptoms.
3.2.2 Past Medical and Surgical History
A thorough medical history should include past medical problems as well as previous surgical procedures. As part of the clinical assessment, it is particularly important to search for comorbidities that may preclude or increase the risk of venous interventions. Questions should address previous DVT or thrombophlebitis, history of thrombophilia, thrombotic disorders, vascular anomalies, peripheral vascular disease, and diabetes as well as previous surgical operations and procedures. Ask about known medical issues such as malignancy or recent operations or hospitalizations, which can increase the risk of DVT:
Has this patient ever had his/her veins evaluated before and, if so, how long ago?
Did the evaluation include an ultrasound assessment?
Did the patient ever have treatment such as vein stripping, ablation, or sclerotherapy?
Has the patient ever had phlebitis?
If the patient is a female, ask if currently pregnant, if planning on future pregnancies, the number of previous pregnancies, and date of the last pregnancy. Conservative management with compression stockings and leg elevation is traditionally indicated if the patient is currently pregnant or considering pregnancy in the near future. Severe cases should be evaluated individually taking into consideration all risks and benefits of invasive treatment options. 8
3.2.3 Family History
Ask the patient if family members have venous disease given that genetics have strongly been implicated in the development of venous insufficiency. 10 Varicose veins are thought to be autosomal dominant with incomplete penetrance, and when both parents have varicose veins, the offspring have a 90% chance of having them. 8, 10, 11
3.2.4 Social History
Occupations that involve standing or sitting for prolonged periods of time can exacerbate venous disease. 7, 8 Obesity and sedentariness are also risk factors for venous insufficiency. 1 It is reasonable to ask if the patient had any recent travel or has plans to travel, which has implications for when to treat. It is advisable to avoid elective invasive treatments prior to a long flight due to increased risk for DVT. Explain to the patient that physical activity (ambulation) should be encouraged following invasive treatments to reduce chances of DVT. 12 Furthermore, a positive history of tobacco, alcohol, or recreational drug use can suggest the presence of important comorbidities.
3.2.5 Allergies
All known allergies should be revealed. Ask if the patient is allergic to lidocaine, latex, or chemical sclerosants such as Sotradecol or polidocanol given that these may be used during venous interventions. Although rare, allergic reactions and anaphylaxis after injection of sclerosing agents can occur. 1
3.2.6 Medications
Oral contraceptives: They are known risk factors for DVT. 13
Anticoagulation: There is no evidence to support the routine use of anticoagulation for thrombosis prophylaxis prior to or after endovenous thermal ablation (EVTA) procedures. 3 On the other hand, EVTA can be safely performed in patients with chronic venous insufficiency requiring long-term warfarin therapy without discontinuation of anticoagulation. 14
3.3 Physical Examination
The physical examination should start with the patient standing in a warm room with good illumination. The clinical evaluation should focus on visible signs of venous disease, which can be helpful in determining the anatomic pattern of venous insufficiency. Physical examination findings such as size, location, and distribution of enlarged veins should be documented, and may include photographs. The physician should pay particular attention to the patient’s ankle because this is probably the most vulnerable region for skin changes and ulcers. Inspection and palpation are essential parts of the physical examination, and auscultation may be helpful in cases of vascular malformations of arteriovenous fistulae, on which a bruit can be noticed.
There are several findings on physical exam unrelated to venous insufficiency that can mimic venous disease. These findings range from relatively benign such as lipomas and bruising to more concerning findings such as infections, lymphadenopathy, melanoma, or other skin cancers. These should be taken into consideration to promote appropriate medical care.
3.3.1 Physical Manifestations of Venous Disease 1, 7, 15
Inspection
Telangiectasias: a confluence of small dilated intradermal blood vessels of less than 1 mm in caliber. Synonyms include spider veins, hyphen webs, and thread veins.
Corona phlebectatica: fan-shaped pattern of numerous small intradermal veins commonly seen around the medial or lateral aspects of the ankle and foot.
Reticular veins: dilated intradermal veins, usually of blue color, measuring from 1 mm to less than 3 mm in diameter.
Varicose veins: subcutaneous dilated and tortuous veins measuring more than 3 mm in diameter with the patient in standing position. Varicose veins develop as a result of valvular incompetence and may involve saphenous veins, saphenous tributaries, or nonsaphenous veins.
When evaluating varicosities, look for patterns of disease:
Medial thigh and/or calf: great saphenous vein reflux.
Anterior thigh: anterior accessory saphenous vein.
Groin or vulvar varicosities: pelvic congestion syndrome (ovarian vein reflux).
Posterior upper thigh: inferior gluteal vein reflux. 16
Edema: increase in volume of extravascular fluid in the subcutaneous tissue and skin, usually more evident in the ankle region, but may extend to the leg and foot.
Venous stasis dermatitis/venous eczema: erythematous dermatitis (red rash or brown discoloration) that develops as a result of increased pressure in the capillary bed, which the patient may describe as itchy. It can be present anywhere in the lower extremity but is often located in the lower leg, around the ankle, or near varicose veins. 1, 17
Hyperpigmentation: dark brownish discoloration of the skin, which usually occurs in the lower leg and ankle regions.
Lipodermatosclerosis: discolored scarred skin associated with severe CVD. In addition to hyperpigmentation, cutaneous sclerosis or scarring has occurred.
Ulceration: skin defect that usually occurs over the medial malleolus and can be seen in healing or active phases.
Palpation
Palpate for cords, varicosities, pitting edema, tenderness, induration, reflux, thrill, groin, or abdominal masses. Also, examine the arterial pulses in the leg, knee, and foot to evaluate for possible arterial insufficiency.
3.4 Imaging
For a complete assessment, the medical history and physical exam should always be supplemented by ultrasound evaluation of the lower extremities (Chapter ▶ 4). For patients with varicose veins and more advanced CVD, computed tomography venography, magnetic resonance venography, ascending and descending contrast venography, and intravascular ultrasonography should be used selectively for conditions such as postthrombotic syndrome, thrombotic or nonthrombotic iliac vein obstruction (May–Thurner syndrome), pelvic congestion syndrome, nutcracker syndrome, vascular malformations, venous trauma, and tumors, and to plan complex open or endovascular venous interventions. 1
3.5 Classification and Quality-of-Life Assessment
CVD has been classified by various systems, which allow researchers to communicate their diagnosis and assess treatment outcomes. 15, 18, 19, 20, 21, 22, 23, 24, 25 The subjective and objective findings gathered from the history and physical exam can be organized using disease-specific severity scoring models such as the CEAP classification 15 and the VCSS 18, 19, 20 ( ▶ Fig. 3.2). It has also been suggested that a disease-specific quality-of-life questionnaire be used. 1 In this section, we briefly describe the 20-item chronic venous insufficiency quality-of-life questionnaire (CIVIQ-20), 23 a quality-of-life questionnaire that has been validated for use in the United States and in other countries. 24, 25

Fig. 3.2 Examples of patients with chronic venous insufficiency with respective CEAP classifications and venous clinical severity scores (VCSSs). The VCSSs include the following elements: pain or discomfort; varicose veins (VV); edema; skin pigmentation; inflammation; induration; number of active ulcers; active ulcer size; and use of compression therapy (Comp). (a) Pain = 2; VV = 2; edema = 1; pigmentation = 2; inflammation = 0; induration = 0; ulcer number = 0; ulcer size = 0; Comp = 2; CEAP = C4a; VCSS = 9. (b) Pain = 1; VV = 3; edema = 1; pigmentation = 0; inflammation = 0; induration = 0; ulcer number = 0; ulcer size = 0; Comp = 1; CEAP= C3; VCSS= 6. (c) Pain = 1; VV = 1; edema = 0; pigmentation = 1; inflammation = 0; induration = 0; ulcer number = 0; ulcer size = 0; Comp = 2; CEAP= C5; VCSS= 5. (d) Pain = 2; VV = 1; edema = 2; pigmentation = 0; inflammation = 0; induration = 0; ulcer number = 0; ulcer size = 0; Comp = 1; CEAP= C3; VCSS= 6. (e) Pain = 1; VV = 3; edema = 2; pigmentation = 3; inflammation = 2; induration = 1; ulcer number = 0; ulcer size = 0; Comp = 1; CEAP = C4b; VCSS = 13. (f) Pain = 1; VV = 2; edema = 1; pigmentation = 2; inflammation = 0; induration = 0; ulcer number = 0; ulcer size = 0; Comp = 1; CEAP= 3; VCSS= 7. (g) Pain = 3; VV = 2; edema = 2; pigmentation = 3; inflammation = 2; induration = 2; ulcer number = 0; ulcer size = 0; Comp = 2; CEAP= 5; VCSS= 16. (h) Pain = 3; VV = 2; edema = 2; pigmentation = 3; inflammation = 3; induration = 3; ulcer number = 2; ulcer size = 3; Comp = 1; CEAP= 6; VCSS= 22.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree