Introduction
Three-dimensional (3D) printing technologies are now entering their fourth decade of use and many medical applications now are very well established and optimized. Despite this, many in the medical field are surprised to hear that 3D printing is not relatively new. This chapter is not an exhaustive look at every development along the timeline for medical 3D printing but instead meant to point out some major milestones which have led us to the state-of-the-art today.
The basis of much of the work done with 3D printing in medicine is surrounding personalization of surgery. This goes all the way back to the beginning and continues today. Personalization typically relies on use of volumetric medical imaging data, allowing the therapy to truly be personalized to the individual patient. Flexibility, complexity of design, and lot sizes of one make 3D printing a good fit for support of the tools, guides, models, and implants which make up the world of personalized surgery. If we consider the medical 3D printing technologies and applications as the toolbox, many pioneering engineers, surgeons, and others contributed to the creation of the tools in the toolbox. Over time the toolbox has continuously expanded by way of software tools, hardware tools, material tools, and workflows which combine these tools in specific ways to solve specific clinical problems. 3D printing has significantly altered several key areas of medicine including craniomaxillofacial surgery, orthopedic surgery, and beyond.
1980s—3D Printing Pioneering Work and Earliest 3D Printing in Medicine
The majority of the work for personalized surgery starts with a volumetric medical imaging study such as computed tomography (CT) or magnetic resonance imaging (MRI). With the advent of the CT scanner in 1967, volumes of data could be acquired, giving for the first time a sense of scale and position of different elements by density. Traditional X-rays did not capture scale and compressed what was 3D data (the patient) into one very two-dimensional (2D) planar image. MRI was commercialized in the 1980s and led to the ability to image soft tissues with much more discretion than was allowed by CT. (Please refer to Chapter 2 for more information on medical imaging.)
In the early 1980s, inventors Hideo Kodama (Japan) and Chuck Hull (US) started independent work on the first 3D printing process which was later coined stereolithography. Hull’s first US Patent was issued in 1987 and the first 3D printing company (3D Systems, Rock Hill, SC) was founded which focused on selling 3D printers, then referred to as the field of rapid prototyping. One might think that 1987 could be the start for 3D printing in medicine, but several very important building blocks, key to this field coming to fruition, actually stretch back to 1981.
In 1981, Dr. Jeffrey Marsh, a craniofacial surgeon, and Dr. Michael Vannier, a radiologist, both physicians at the Washington University School of Medicine (St. Louis, MO), worked with an engineer named James Warren (McDonnell Douglas, St. Louis, MO) on the concept of anatomic modeling. The goal was to take slice data from a CT scan and use it to replicate individual slices of materials that would form a 3D object when assembled. McDonnell Douglas was in the aerospace field and working with many high-performance materials including titanium. An image postprocessing technique called thresholding (Described in Chapter 3) was used to delineate the Hounsfield units (measure of grayscale intensity) for bone in the CT scan, creating individual slices of data just for the bone structure. This was first used to model a young boy with a large frontonasal encephalocele. The digital files from the segmented CT slices were transferred to a milling machine which traced these slices, which were of the same thickness as the CT scan slices, into titanium. When assembled and stacked up these slices formed, to scale, a model of the boy’s bone structure which clearly illustrated the large bony perforation above his left orbit. This work continued into 1982 with less exotic materials, moving to acrylic sheets instead of titanium. , Due to lack of funding, the work ceased in 1982, but several of the models remain intact. Marsh and Vannier published a paper and a book on their pioneering efforts in 3D imaging in the early 1980s, but there was only a passing comment made in the paper regarding their physical modeling efforts ( Fig. 1.1 and 1.2 ). ,


Also in 1981, a physicist named F. Brix in Kiel, Germany, started work that used the external shape of the body, derived from a CT scan, milled from different materials, as radiation therapy compensators. This work led to others in Kiel, including Ulrich Kliegis, to start milling 3D shapes from solid blocks of foam, beginning with anatomic models. Kliegis started a company called MEK/Endoplan (Kiel, Germany) to offer the service of anatomic modeling and later commercialized an anatomic modeling system that was even brought to the annual meeting of the Radiological Society of North America (RSNA) in the mid-1980s. This concept was way ahead of its time and commercialization was slow, but work progressed in the 1980s and beyond for Kliegis and the group at Kiel. Many influential maxillofacial surgeons who in the 1980s trained at Kiel later took the concepts for anatomic modeling with them to Switzerland (Professor Dr. J. Thomas Lambrecht) and Austria (Professor Dr. Rolf Ewers) where the applications and technology continued to evolve and mature. , Lambrecht’s book, published in 1996, contains clinical cases from the late 1980s to the early 1990s and is considered by many to be the authoritative work on early oral and maxillofacial surgery applications ( Fig. 1.3 ).

In the Department of Radiology at the University of California, Los Angeles (UCLA), in 1984, a physicist named Dr. Nicholas Mankovich was hard at work solving some of the same issues for anatomic modeling. He and his team used a similar approach to the St. Louis group for milling of individual slices of a CT scan from acrylic and stacking them to create life-sized 3D models of anatomy. The first clinical needs were for modeling the bone structure of patients with defects in their skull requiring cranial reconstruction. The team created models that would allow for design and construction of patient-matched implants for the skull, called cranioplasties, working with legendary maxillofacial prosthodontist Dr. John Beumer. This work at UCLA continued until 1988 when Mankovich collaborated with Chuck Hull and Scott Turner at 3D Systems to create what was the very first 3D printed anatomic model, created with stereolithography. Once the concept of stereolithography had been proven to work and showed the needed accuracy, the UCLA team abandoned the earlier stacked layer methods in favor of the more robust and accurate stereolithography process.
A US patent was issued to David White in 1982 for a technique surrounding anatomic modeling primarily for custom implant creation using subtractive, milling techniques. CEMAX (Fremont, CA) licensed this patent in 1985 and used it to create a service business for anatomic modeling, servicing surgeons and medical device companies in need of these models to plan surgery or design patient-matched implants. One such user of these anatomic models was Dr. William Binder and the company Implantech Associates (Ventura, CA). Implantech has pioneered patient-matched silicone facial and body prostheses made using CT imaging.
Another competing method to the White method was being used at another California-based orthopedic implant company called Techmedica (Camarillo, CA) in the 1980s and into the early 1990s. The model quality seems crude by today’s standards, but the accuracy of the anatomic models met the clinical needs at that time. The models were created by tracing 1:1 CT scan images by a tracer into acrylic sheets which were then stacked together, smoothed along the outside contours with clay, and then used to cast sequential copies of the anatomy. The primary clinical focus for Techmedica was on large orthopedic tumor reconstruction cases, limb salvage cases, and complex joint revision cases. Techmedica was later sold to Intermedics Orthopedics (Austin, TX), but at least one product still exists from the Techmedica days, a patient-matched total joint replacement for the temporomandibular joint, now sold by TMJ Concepts (Ventura, CA).
1990s—3D Printed Anatomic Models and Personalized Implants
Fried Vancraen and his firm Materialise (Leuven, Belgium) play an important role in this industry starting in 1990, the same year that Materialise was founded. Vancraen was interested in the 3D printing of anatomic models with a newly acquired SLA-250, with serial number 32 (3D Systems, Rock Hill, SC), and his first anatomic model made by stereolithography was produced in November 1990. Vancraen quickly learned that the software workflow for converting what were then proprietary file formats for each CT scanner was very difficult to utilize. In 1991, to help this workflow, the Materialise Interactive Medical Image Control System (Mimics) software was created; and it was commercialized in 1992. This software paved the way in creating a service business for Materialise and for others to follow in their footsteps. Vancraen was instrumental in launching and leading the Phidias project in Europe to specifically study the clinical benefits of 3D printed anatomic models in comparison to static 3D virtual images. The Phidias Project, run by European radiologists, lasted from 1992 to 1995 with trailing data reports following. This project was way ahead of its time in gathering data to support reimbursement for 3D printed anatomic models. One of the lasting and important contributions of the Phidias project was the creation of a first-of-its-kind material for stereolithography which allowed selective coloration by overcuring select regions of interest and biocompatibility. The material was developed by Materialise and Zeneca Specialties (London, United Kingdom) and allowed a second, red coloration to be used to highlight select anatomic structures within the otherwise clear anatomic model. This material was commercialized by Zeneca and later sold to Huntsman (The Woodlands, TX). Huntsman was acquired by 3D Systems in 2011 and folded into their stereolithography materials portfolio. This material is still in active, worldwide use today.
3C Design (Founded by RW Christensen, DC Chase, and D Crook) was started in Dallas, TX, in 1992, to focus on aerospace, industrial, and medical uses for stereolithography. In 1995, the company folded and what would become Medical Modeling (Golden, CO) got its start with the same technology in Golden, Colorado. At first, the applications focused solely on preoperative anatomic models to assist with total joint replacement of the temporomandibular joint, but they quickly expanded to serve many surgical specialties and clinical needs. In 2000, Andy Christensen, employed with Medical Modeling since 1996, purchased the company and kept adding to its armamentarium of services and workflow development to support the medical applications of 3D printing. This included anatomic modeling, design of personalized implants, virtual surgical planning, and eventually additive metals for implant production.
In 1994, on the other side of the globe, building on the work of Mankovich, Beumer, and others, the company Anatomics (Melbourne, Australia), led by neurosurgeon Dr. Paul D’Urso, was created with a focus on anatomic modeling and patient-matched cranioplasty implants. D’Urso and group later published a seminal paper on a prospective clinical trial for 3D printed anatomic models in 1999 which showed benefits to surgeon, patient, and hospital.
Companies who sold 3D printers started to take notice of this emerging market; and, in 1996, there was major movement from Stratasys (Eden Prairie, MN), another major player in the 3D printer and material space. Scott Crump invented the technology called Fused Deposition Modeling (FDM) and cofounded Stratasys with his wife Lisa in 1989. Lisa became quite interested in the anatomic modeling area and in 1996 led the effort for Stratasys to obtain the first (and possibly still the only) Food and Drug Administration (FDA) clearance of a 3D printer, the FDM MedModeller. Stratasys commercialized the product and even exhibited at the RSNA annual meeting in Chicago in the late 1990s to try and market 3D printers to hospitals. The Materialise Mimics software was also FDA cleared at the same time to provide more of an end-to-end solution from CT scan to model. A company was eventually spun-out of Stratasys to commercialize this idea, but eventually it was discontinued due to lack of traction. This concept was 20 years ahead of its time and the industry owes Lisa Crump a debt of gratitude for pushing point of care 3D printing first.
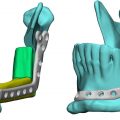
The very beginnings of virtual surgery also date back to the mid-1990s, with Dr. James Xia’s work in Hong Kong. Xia’s work dealt with manipulating, cutting, and moving objects in space related to oral and maxillofacial surgical procedures. He relocated to Houston around 2000 and so began a long career with oral and maxillofacial surgeon Dr. Jaime Gateno first at University of Texas (Houston, TX) and later at Methodist Hospital (Houston, TX). The group’s focus was on orthognathic surgery involving osteotomies of the mandible and maxilla. In the 2000s, this dynamic team had a singular focus on tackling each step of the virtual surgery and clinical transfer process step by step. Publishing each subsequent step along the way they established workflows and accuracy standards for this work in collaboration with clinical and industry collaborators. Through work funded by several NIH grants, the team flushed out many of the key steps of the process along with collaborator Medical Modeling, who commercialized some of the workflow steps in its services for orthognathic surgical planning and guidance. At the core of these technologies was the ability to osteotomize bony segments in a virtual environment and then move these segments to desired, new, positions. Once the desired outcome was expressed digitally, a series of 3D printed templates or splints would be output to transfer the clinical plan from the computer to the operating room. This group went on to publish some of the most influential manuscripts in this space. ,
2000s—Digital Design, Additive Metals, and Foundations for Future Virtual Work
The first meaningful use of templates came with the launch of SurgiCase by Materialise in 2000. Building on previous software development and workflows, the SurgiCase software was initially targeted for dental implant simulation, translating the implant’s position from the simulation to the patient, and it also included the creation of patient-specific, 3D printed dental drill guides. In 2001, Materialise purchased Columbia Scientific (Columbia, MD), an industry leader for dental implant planning software (SimPlant), thereby combining their SurgiCase software product line with SimPlant. Another technological advance that helped push this application forward was the commercialization of Cone-Beam CT (CBCT), which allows for volumetric imaging studies to be performed in the oral surgeon’s office and led to much wider use of CT in the craniomaxillofacial area.
Around 2000, computer-aided design (CAD) software programs started to become more advanced and products such as Freeform Modeling Systems 3D touch enabled haptic device systems for medical and dental modeling, product design, and digital content creation became available (Sensable Technologies, Woburn, MA). Dr. Richard Bibb in Cardiff, Wales, did pioneering work with these haptic devices and design software. Using the more artistic interface allowed for creation of patient-matched craniomaxillofacial implants; and for the first time these implants could be designed net shape, something very difficult previously with traditional CAD software. This work had an immense impact on the specific clinical application for patient-matched cranioplasty and changed how this work would be done in the future around the world.
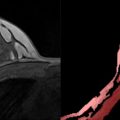
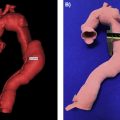
Meanwhile in Dallas, TX, in 2001, a craniofacial surgeon named Dr. Kenneth Salyer embarked on what would be a multiyear project to separate two twin boys born joined at the head (craniopagus twins). Using the latest anatomic modeling provided by Medical Modeling (Golden, CO), he and his team created 3D printed models of bone, skin, brains, venous and arterial systems, ventricles, and more that were integral to the successful separation which took place in 2003. While not the first case where anatomic models were used by surgeons separating twins, this case garnered national attention and lead to a seminal paper on 3D printing for craniopagus cases and a 2004 3D Systems User Group SLA Excellence Award Grand Prize. Earlier anatomic models for conjoined twins separation surgeries go back as far as 1995 with the Rainey twins who were separated at Wilford Hall Medical Center, Lackland Air Force Base in San Antonio, TX. Medical Modeling’s work for conjoined twins included modeling for 15 sets of twins by 2006. Salyer is now retired from clinical practice but had used anatomic models to plan for more than 500 craniofacial surgeries during the 2000s ( Fig. 1.4 ).