Fig. 23.1
Schematic diagrams of the cross-sectional anatomy, compartments, and recommended needle paths at various levels in the upper extremity. (a) Humeral head and proximal metaphysis. (b) Proximal humeral diaphysis. (c) Mid-humeral diaphysis. (d) Distal humeral metaphysis. (e) Distal humeral epiphysis and elbow joint. (f) Proximal radius and ulna. (g) Mid-radial and ulnar diaphyses. (h) Distal radial and ulnar diaphyses. (i) Distal radial and ulnar metaphyses and epiphyses
The anterior and posterior compartments of the arm are separated by the medial and lateral intermuscular septa [7, 9]. The anterior compartment contains the biceps, brachialis, brachioradialis, and coracobrachialis muscles, and the posterior compartment contains the triceps muscle. The brachial artery and vein and the median nerve are extracompartmental in the upper arm; however, these neurovascular structures enter the anterior compartment in the distal arm. Likewise, the radial nerve is located in the posterior compartment in the upper arm but crosses over into the anterior compartment in the distal arm. The ulnar nerve remains in an extracompartmental location throughout the arm.
The anatomy of the forearm has been sorted into multiple compartmental classifications [7, 9, 10]. In a commonly used classification, the forearm is divided into three compartments. The dorsal compartment contains the extensor muscles: the supinator, anconeus, extensor digitorum, extensor digiti minimi, extensor carpi ulnaris, extensor pollicis longus, and abductor pollicis longus. The lateral compartment (also known as the “mobile wad of Henry”) contains the brachioradialis and two wrist extensors (i.e., the extensor carpi radialis longus and extensor carpi radialis brevis). The volar compartment contains the flexor muscles: the pronator teres, flexor carpi radialis, palmaris longus, flexor digitorum superficialis, flexor carpi ulnaris, flexor pollicis longus, flexor digitorum profundus, and pronator quadratus. The radius, ulna, and interosseous membrane separate the volar and dorsal compartments, which can be subcategorized as superficial or deep. In the proximal forearm, the radial nerve is located between the lateral and volar compartments. The radial and ulnar arteries and median and ulnar nerves are located in the volar compartment. The anterior and posterior interosseous nerves and vessels are located in the volar and dorsal compartments, respectively.
Lower Extremity Compartments
The cross-sectional anatomy of the lower extremity at different levels is shown in Fig. 23.2. The thigh is divided into anterior, posterior, and medial compartments [7, 8, 11]. The anterior compartment contains the iliotibial tract, tensor fascia lata, quadriceps (i.e., the rectus femoris, vastus lateralis, vastus intermedius, and vastus medialis), and sartorius muscles. The posterior compartment contains the hamstring muscles (i.e., the biceps femoris, semitendinosus, and semimembranosus), popliteal artery, and sciatic nerve. The femoral artery and vein enter the thigh medially, are contained within the femoral sheath, and are considered extracompartmental, as they are located between the anterior and medial compartments. Distal to the adductor canal, the superficial femoral artery becomes the popliteal artery, which is located in the posterior thigh. A portion of the gluteus maximus resides in the posterior proximal thigh but is not technically within the posterior compartment. The medial compartment contains the gracilis and the adductor muscles. The sciatic nerve is located in the posterior thigh, between the adductor magnus and gluteus maximus in the upper thigh and between the adductor magnus and the biceps femoris in the lower thigh. The fascia lata forms the superficial boundary of all three compartments. The medial and lateral intermuscular septa, which attach to the femur, separate the anterior compartment from the medial and posterior compartments. A thin fascial plane separates the medial and posterior compartments.
Fig. 23.2
Schematic diagrams of the cross-sectional anatomy, compartments, and recommended needle paths at various levels in the lower extremity. (a) Femoral head and neck. (b) Proximal femoral diaphysis. (c) Mid-femoral diaphysis. (d) Distal femoral diaphysis. (e) Distal femoral metaphysis. (f) Distal femoral epiphysis and knee joint. (g) Proximal tibial and fibular epiphyses and metaphyses. (h) Proximal tibial and fibular diaphyses. (i) Mid-tibial and fibular diaphyses. (j). Distal tibial and fibular diaphyses. (k) Distal tibial and fibular epiphyses
The leg has four compartments: anterior, deep posterior, superficial posterior, and lateral [7, 8, 11]. The anterior compartment contains the extensor muscles (i.e., the tibialis anterior, extensor digitorum longus, and extensor hallucis longus), the deep peroneal nerve, and the anterior tibial artery and vein. The deep posterior compartment contains the tibialis posterior, popliteus, flexor digitorum longus, and flexor hallucis longus muscles; the peroneal artery and vein in the lateral part of the compartment; and the posterior tibial artery and vein and the tibial nerve in the medial part of the compartment. The superficial posterior compartment contains the soleus, gastrocnemius, and plantaris muscles and the sural nerve. The lateral compartment contains the peroneus longus and peroneus brevis muscles and the common peroneal nerve, which becomes the superficial peroneal nerve after giving off the deep peroneal nerve. All four compartments are encased superficially by the deep crural fascia. The anterior, posterior, and transverse intermuscular septa and the interosseous membrane form the borders between the various compartments.
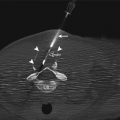
Biopsy Approach
The main considerations in planning the biopsy needle path are positioning the tract along the intended surgical incision site and avoiding disease-free compartments, structures that are needed for maintaining function or for reconstructive surgery, and major neurovascular structures. Some general guidelines should be followed [1, 6–8, 12, 13]. For example, the shortest distance possible from the skin surface to the tumor should be selected. It is important to discuss the anticipated needle path with the surgeon who will be performing the definitive surgery.
The key point to consider when selecting a biopsy path is the risk of tumor seeding along the needle tract, specifically when primary musculoskeletal sarcoma is suspected [1, 5, 6]. For this reason, the biopsy tract is resected en bloc during definitive surgery [1, 5, 6]. The needle path must be close to the intended surgical incision site so that the needle path will be amenable to resection during definitive surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree