7 Anatomy and Development of the Facial Nerve
The facial nerve is worthy of considerable attention because of its very complex derivation, anatomy, and pathology. It is composed of special visceral efferent, special visceral afferent, and general somatic afferent fibers traveling a circuitous course from three central brainstem nuclei to terminations in the functional end plates of the muscles of facial expression; taste buds of the anterior tongue; lacrimal, nasal seromucus, and minor salivary glands; and ear canal skin (Fig. 7.1). The lengthy course of the facial nerve can be divided into three parts: intracranial, intratemporal, and extracranial. The intratemporal portion constitutes the anatomically most complex portion of this course and is the central focus of this chapter. However, because the imaging issues of the facial nerve require familiarity with the entire course of the facial nerve, we review the relevant anatomy and pathology of the facial nerve from its brainstem origins to its peripheral insertions.
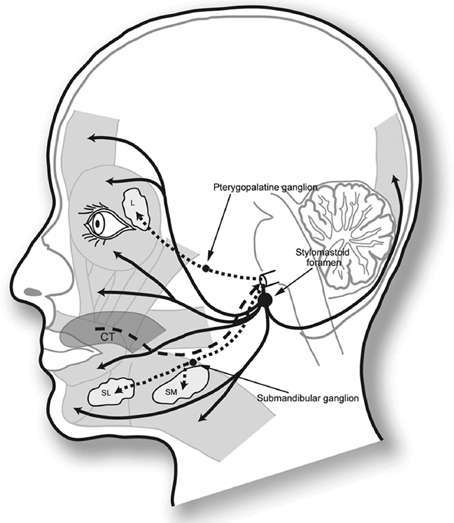
Fig. 7.1 Main functions of the facial nerve. The solid black line corresponds to the somatic motor output to the facial musculature anteriorly and the occipital muscle posteriorly, exiting through the stylomastoid foramen. The upper hatched lines illustrate the course of the parasympathetic fibers that end in the lacrimal glands (L), as well as the nasal and palatal mucosa via the pterygopalatine ganglion. The inferior hatched lines correspond to the parasympathetic fibers that innervate the submandibular and sublingual glands (SL and SM) via the submandibular ganglion. Taste information is projected via the chorda tympani (CT), represented by the dashed line from the tongue to the facial nerve trunk.
For background, we will begin with a discussion of the embryologic development of the facial nerve and proceed to the normal anatomy of the entire facial nerve, using computed tomography (CT) and magnetic resonance imaging (MRI) to illustrate. A practical imaging approach to the facial nerve, including imaging techniques and preimaging topographic localization, is presented. Next, pathological conditions affecting the facial nerve are briefly reviewed. Because many of the lesions that cause facial nerve injury are discussed in depth in other chapters of this book, only the lesions not covered elsewhere (facial schwannoma, Bell’s palsy, hemifacial spasm, hemangioma) are covered here.
Embryology
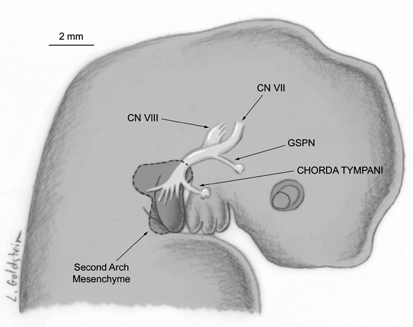
The embryological derivation of the facial nerve and fallopian canal involves a complex interaction of the facial nerve, otic capsule, and second branchial arch mesenchyme. Development of the fallopian canal can be divided into three phases—blastemal, cartilaginous, and osseous periods. The intricate path of the facial nerve is largely determined during the blastemal phase, days 20 to 48, before the surrounding otic capsule and mesenchyme embed the facial nerve in cartilage and, subsequently, bone.1 The neural crest cell progenitors of the facial nerve can be identified as a facioacoustic primordium in a 3 mm fetus (day 20) in the epipharyngeal placode of the second branchial arch, adjacent to the otic vesicle and attached to the rhombencephalon.2 By day 32, the geniculate ganglion has developed, and the motor trunk and chorda tympani nerve are distinct (Fig. 7.2). By day 33, the chorda tympani nerve enters into the mesenchyme of the first branchial arch, and the facial motor trunk inclines caudally and ventrally in the second branchial arch mesenchyme. The greater superficial petrosal nerve appears in the 8 to 11 mm fetus (day 37) and the nervus intermedius is present in the 16 to 18 mm fetus (day 47.5). The horizontal or tympanic segment of the facial nerve elongates from day 44 to 47.5, and the motor trunk in the vertical segment lengthens with the growing second arch derivatives. With growth of the branchial arch derivatives and the fetal head, the motor trunk elongates in a sinuous extratemporal course (Fig. 7.3).
The intramedullary portion of the facial nerve can be recognized near the end of the fifth week of gestation as a collection of neuroblasts in the metencephalic portion of the rhombencephalon. The motor nucleus of cranial nerve VI (CN VI) lies in close proximity. As the metencephalon elongates, the abducens motor nuclei ascend and move dorsally, displacing the facial nerve fibers and creating the internal genu of the facial nerve.
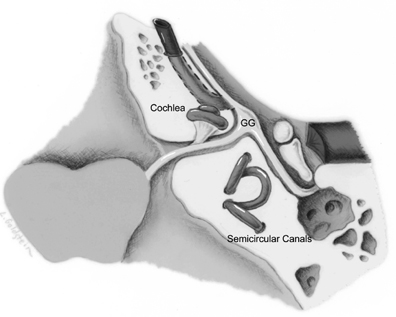
With development of the otic vesicle into the otic capsule and labyrinth during weeks 4 to 8, the facial nerve medial to the geniculate ganglion becomes distinct from, but in close proximity to, the acoustic nerve in the region of the future internal auditory canal and labyrinthine segments. The semicircular canals (SCCs) and vestibule develop caudal to the geniculate ganglion, placing the labyrinthine segment of the facial nerve between the cochlea and the vestibular organs. During week 8, the rudimentary fallopian canal begins as a sulcus containing the facial nerve, blood vessels, and stapedius muscle, on the posterior aspect of the otic capsule.3 The portions of the facial nerve in close approximation to the otic capsule become enveloped by cartilage and subsequently bone. With formation of the periosteal portions of the temporal bone, the remaining intratemporal portions of the facial nerve become encased in bone. The vertical segment of the facial nerve and fallopian canal continue to elongate after birth as the mastoid tip grows inferiorly.
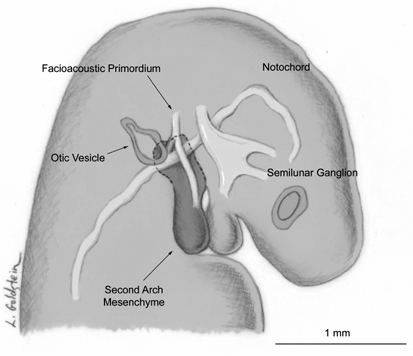
Fig. 7.2 Illustration of a 6-week embryo. The cells of the facioacoustic primordium lie in close proximity to the developing otic vesicle. This cell tract extends into the mesenchyme of the second branchial arch. (From Gasser RF, May M. Embryonic development. In: May M, Schaitkin BM, eds. The Facial Nerve. 2nd ed. New York, NY: Thieme Medical Publishing; 2000. Reprinted with permission.)
Because of this complicated derivation, localized areas of bony dehiscences in the facial canal are common, in as many as 55% of temporal bones.4,5 More recent work, utilizing light microscopy rather than visual inspection, demonstrated focal dehiscence in 74% of specimens.6 The failure of periosteal bone to develop has been suggested to be responsible.4 Arterial and venous structures course through the facial nerve canal along with the nerve itself; one theory is that unusually prominent vascular structures may cause delay in development of the periosteal bone with subsequent dehiscences.4,6 An alternative theory is based on the observation that most of the dehiscences are in areas where the canal is completed by Reichert’s cartilage and that discontinuity of the cartilage may result in canal wall defects.6 These normal defects are small, from 0.4 to 3.0 mm, generally less frequent in well-pneumatized temporal bones, and often bilateral and relatively symmetric.6,7
Gaps in the continuity of the osseous wall may be observed in any segment.4,8–10 Most commonly, dehiscences are located in the tympanic segment superior and posterior to the oval window, especially along its medial wall. Focal defects in the anterior epitympanic sinus and in the jugular bulb are somewhat less common. Gaps more anteriorly in the tympanic facial nerve canal, near the cochleariform process, and in the mastoid segment are rare.7
Dehiscent areas along the tympanic aspect of the facial nerve canal may result in inferior protrusion of the tympanic segment through these defects.11 Such a protrusion may vary from a slight bulge to a complete prolapse of the nerve, allowing the nerve to abut the stapes superstructure. A profound protrusion may result in conductive hearing loss, although this is very uncommon.4 A prolapsed nerve may conceal all or some of the oval window; preoperative knowledge of this anomaly is of considerable importance, particularly prior to stapes surgery.12
With CT, the appearance of the protruding nerve is that of a smooth soft tissue density with inferior convexity emanating from the undersurface of the lateral SCC at the level of the oval window on coronal sections.11,12 The CT diagnosis of this entity is only possible in the absence of middle ear debris. If the inferior margin of the nerve is not outlined by air because of middle ear inflammatory debris, it is difficult to distinguish the nerve with CT. When such an inferior protrusion is encountered, the surgeon should be cautious of the possibility of dehiscence.11,12 Because the tympanic segment most commonly produces a groove on the undersurface of the lateral SCC on coronal CT sections, absence of this groove should be viewed with suspicion, particularly in those individuals in whom middle ear opacity precludes identification of the undersurface of the nerve itself.
Numerous anomalies have been described in the course of the facial nerve canal. Commonly, they are associated with congenital dysplasias of the temporal bone.13
Normal Anatomy
The seventh cranial nerve supplies three principal functions. In addition to its motor function, various branches serve the sensory functions of transmitting taste from the anterior two thirds of the tongue and superficial sensation from the cutaneous regions around the auricle of the ear. Additional branches provide autonomic innervation to the lacrimal, sublingual, submandibular, oral cavity minor salivary, and nasal seromucus glands (Fig. 7.1). The facial nerve may be thought of (true enough) as a simple neural trunk exiting the pontomedullary junction to course through the temporal bone (Fig. 7.4), in proximity to the organs of balance and hearing, but this disguises the true complexity of its origin and destinations.
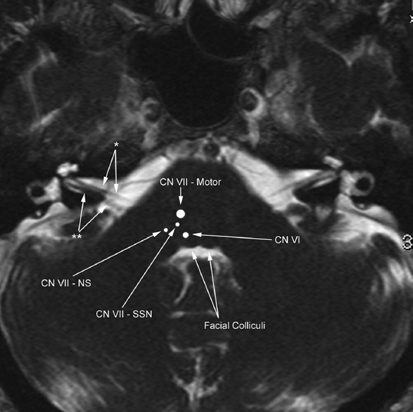
The facial nerve, the nerve of the second branchial arch, arises from three brainstem nuclei. The largest, or motor nucleus (Fig. 7.5 and Fig. 7.6), is a nuclear column in the ventrolateral pontine tegmentum.14–17 This motor nucleus is the origin for efferent motor fibers to the muscles of facial expression and supplies motor fibers to the stapedius, stylohyoid, and posterior belly of the digastric muscles. Cortical input to the facial nucleus is from the motor face area in the precentral and postcentral gyri, with connections through the corticobulbar tract to the internal capsule, midbrain, and pons. The corticobulbar tract fibers serving the motor area of the forehead/upper face are bilaterally innervated, whereas the tracts to the remainder of the face are crossed only, resulting in unilateral innervation. This is the anatomic basis for the classical distinction between central facial nerve palsy, sparing the forehead, and peripheral facial nerve palsy, involving both the upper and lower face. This century-old interpretation of supranuclear innervation has been challenged by more recent data. One study of macaque monkeys found scant bilateral direct cortical innervation to the upper facial motor subnucleus, but robust bilateral cortical innervation to the lower facial motor subnucleus with a contralateral predominance. The upper facial motor subnucleus was presumed to receive additional indirect cortical inputs. A central or supranuclear facial palsy would result in contralateral lower facial muscle weakness because those lower facial motor neurons are much more dependent on direct cortical innervation. The ipsilateral lower facial motor neurons continue to receive their contralateral dominant direct cortical innervation, and the upper facial motor neurons function from indirect cortical innervation.18
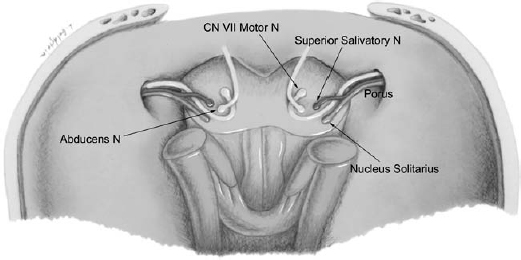
Fig. 7.5 Diagram of the individual nuclei of the facial nerve and their relative positions in the pons. The motor nucleus of the facial nerve (CN VII Motor N) gives rise to fibers that course slightly medially and dorsally to loop around the abducens nucleus, then moves ventrally and laterally toward the root exit. Along the way, the nerve picks up fibers from the superior salivatory nucleus and nucleus solitarius. The fibers from the superior salivatory nucleus and the nucleus solitarius travel distinctly as the nervus intermedius. The facial nerve trunk moves through the cerebellopontine angle cistern to the porus.
The superior salivatory nucleus is located just dorsal to the motor nucleus (Fig. 7.5) and contributes preganglionic parasympathetic secretomotor fibers. These fibers terminate in and stimulate the lacrimal gland and nasal seromucus glands via the greater superficial petrosal nerve and the submandibular, sublingual, and oral cavity minor salivary glands via the chorda tympani nerve.
A third nuclear column found in the upper medulla, the solitary tract nucleus (nucleus solitarius) (Fig. 7.5 and Fig. 7.6), receives the afferent information of the special sensory fibers of taste via the chorda tympani, and general sensory fibers of proprioception and sensation from the external auditory canal (Table 7.1).19–21
| Facial Nerve Nuclei | Function |
| Motor | Motor innervation to the muscles of facial expression, stylohyoid, stapedius, posterior belly of digastric muscles |
| Superior salivatory | Preganglionic parasympathetic secretomotor stimulation to the lacrimal (via greater superficial petrosal nerve), submandibular, and sublingual glands (via chorda tympani nerve) |
| Solitary tract | Receives afferent information (nucleus solitarius) of the special sensory fibers of taste (via chorda tympani nerve), and general sensory fibers of proprioception and sensation (external auditory canal) |
Within the lower pontine brainstem, the motor fibers of the facial nerve loop dorsally around the abducens nerve nucleus (CN VI). The bulge in the floor of the fourth ventricle formed by these looping fibers is referred to as the facial colliculus (Fig. 7.5).22 These fibers then course ventrolaterally to exit the anterolateral pons and enter the cerebellopontine angle (CPA) cistern (Fig. 7.7, Fig. 7.8, and Fig. 7.9).
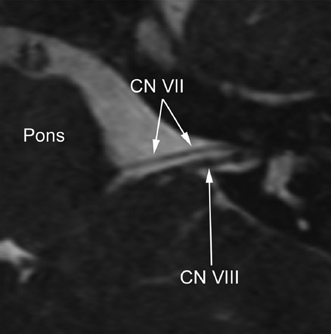
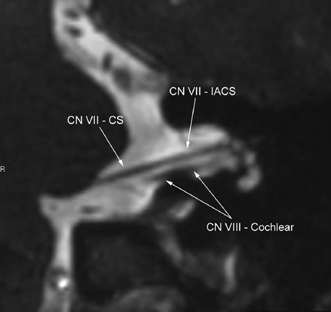
Fig. 7.8 Oblique coronal reconstruction of a three-dimensional T2-weighted sequence through the internal auditory canal (IAC) demonstrates the cisternal segment of the facial nerve (CN VII – CS) directed slightly superiorly and laterally to the IAC, and running horizontal to the fundus (CN VII – IACS). The facial nerve is immediately superior to the cochlear division of the vestibulocochlear nerve (CN VIII – Cochlear) in this section. The T2-weighted sequences are particularly useful in patients with capacious cerebrospinal fluid spaces in the IAC.
The parasympathetic secretomotor fibers from the superior salivatory nucleus (bound for the lacrimal, submandibular, and sublingual glands) combine with the special sensory fibers of the solitary tract nucleus (conveying taste from the anterior two-thirds of the tongue) to form the nervus intermedius (of Wrisburg) or sensory root. The nervus intermedius fibers may join the motor root of the facial nerve just as they exit the brainstem, or may initially attach to the vestibulocochlear (VIII) nerve, joining the facial nerve near the meatus of the internal auditory canal (IAC).23,24 The two remain as a combined nerve trunk through the IAC to their diverging points within the temporal bone (Fig. 7.5 and Fig. 7.10).20
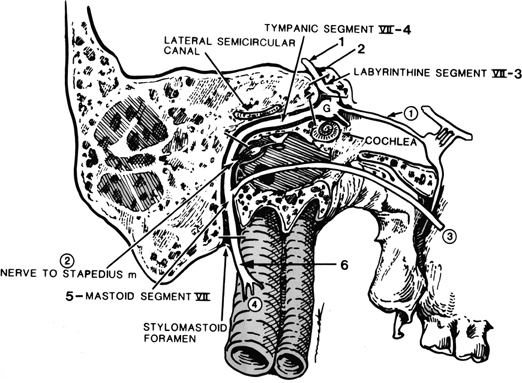
The facial nerve departs the brainstem at the lower border of the pons at the pontomedullary junction. (Fig. 7.5, Fig. 7.7, Fig. 7.8, and Fig. 7.9) Within the CPA cistern, the facial nerve is the most anterior, the vestibulocochlear nerve most posterior, with the nervus intermedius, as its name suggests, between the two. The facial nerve from the pontomedullary junction to parotid may be described as having six segments: cisternal, intracanalicular (internal auditory canal), labyrinthine, tympanic, mastoid, and extracranial (intraparotid) (Fig. 7.11 and Table 7.2).20,25,26
The cisternal segment of the facial nerve, the portion of the nerve that stretches across the CPA cistern from the brainstem to its entry into the porus acusticus of the IAC (Fig. 7.7, Fig. 7.8, and Fig. 7.9), is 24 mm in length. With MRI, it is identified anterior to the vestibulocochlear nerve (CN VIII) within the CPA cistern (Fig. 7.6, Fig. 7.7, and Fig. 7.8).20,27,28 The nervus intermedius cannot be separately resolved from the main motor trunk of the facial nerve.
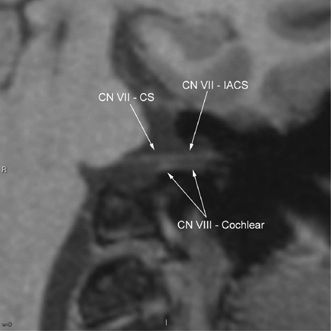
Fig. 7.9 Oblique coronal fast spin echo T1-weighted magnetic resonance image through the internal auditory canal (IAC) demonstrates the cisternal segment of the facial nerve (CN VII – CS) directed laterally to the IAC, and running horizontal to the fundus (CN VII – IACS). The facial nerve is immediately superior to the cochlear division of the vestibulocochlear nerve (CN VIII – Cochlear) in this section. This image is the corollary of Fig. 7.8.
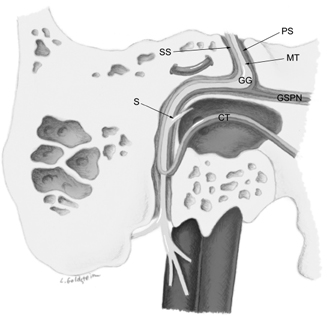
Fig. 7.10 Diagrammatic representation of the facial nerve functional distinction by segment. At the fallopian canal, the facial nerve is comprised of the motor trunk (MT), the parasympathetic secretomotor (PS) fibers, and the special sensory (SS) fibers. The parasympathetic and special sensory fibers comprise the nervus intermedius. At the level of the geniculate ganglion (GG), the greater superficial petrosal nerve (GSPN) exits via the facial hiatus. A single motor branch to the stapedius muscle (S) exits just distal to the posterior genu. Along the course of the mastoid segment, the special sensory fibers and remaining parasympathetic fibers exit as the chorda tympani (CT) to course through the middle ear.
The facial nerve then enters the porus acusticus of the IAC to become the intracanalicular segment, 8 mm in length, following a shallow gutter in the anterosuperior aspect of the IAC. In the lateral aspect of the IAC, a transverse bony crest, the crista falciformis, separates the facial nerve above from the cochlear nerve below. This superior compartment is further divided by a vertical crest of variably ossified arachnoid tissue (Bill’s bar), which separates the facial nerve from the superior vestibular nerve.29 MR sequences demonstrate the facial nerve and superior vestibular nerve in the IAC as discrete structures positioned superior to the cochlear and inferior vestibular nerves (Fig. 7.8, Fig. 7.9, and Fig. 7.12). The mnemonic “seven up, coke down” refers to the relative positions of these cranial nerves in the IAC.
The facial nerve canal or fallopian canal begins as the facial nerve exits the anterosuperior portion of the IAC fundus. Within the facial nerve canal, the facial nerve is subdivided into three segments: labyrinthine, tympanic, and mastoid. The anterior (first) genu (Fig. 7.13 and Fig. 7.14) where the geniculate ganglion can be found, separates the labyrinthine segment from the tympanic segment, and the posterior (second) genu separates the tympanic segment from the mastoid segment. The motor component of the facial nerve and its associated nervus intermedius both enter the labyrinthine segment through a narrow aperture at the IAC fundus, the narrowest portion of the fallopian canal.21,30–32 Throughout its course in the fallopian canal, the facial nerve is surrounded by a sheath consisting of periosteum, epineurium, and perineurium.33 The dura may extend as far peripherally as the geniculate ganglion.
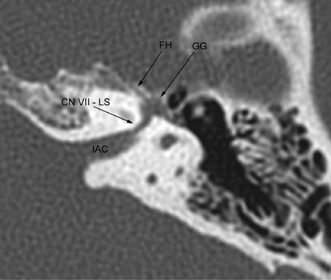
The labyrinthine segment of the facial nerve, so named because of its intimate relationship to the cochlea and SCCs, courses anterolaterally from the IAC fundus at an angle of ∼125 degrees relative to the long axis of the IAC.33
This segment of the facial nerve canal is the narrowest (< 0.7 mm) and shortest (3 to 5 mm). It follows a gentle and medially concave curve (Fig. 7.13 and Fig. 7.14A), lying in a sulcus between the cochlear and vestibular labyrinth, the intervestibulocochlear groove. The facial nerve is particularly vulnerable in this location and is subject to compromise or complete transection by temporal bone fractures, particularly those in the transverse plane. Further, this segment is in close relationship to the vestibule and ampulla of the superior SCC and may be compromised during translabyrinthine surgery.
The bony margins of this short labyrinthine segment are complex. Medially, the labyrinthine segment is adjacent to the superior portions of the spiral turns of the cochlea. Superiorly, the labyrinthine segment is bordered by the petrous cortex, which may or may not be pneumatized by supralabyrinthine air cells. Laterally and posteriorly lie the ampullae of the horizontal and superior SCCs.13,20,31,33
The labyrinthine segment of the facial canal terminates in the geniculate fossa, a bulbous enlargement of the canal containing the geniculate ganglion (Fig. 7.13 and Fig. 7.14A). The ganglion is usually enveloped by bone, but in up to 15% of patients it may be incomplete or absent, making it vulnerable during middle cranial fossa surgery.33 The geniculate ganglion contains the cell bodies of the special sensory neurons subserving the taste function of the anterior two thirds of the tongue. These taste fibers ascend to the geniculate ganglion by coursing centrally with the lingual branch of the mandibular division of the trigeminal nerve,34 then departing the lingual nerve to form the chorda tympani nerve as it enters the temporal bone via the canal of Huguier (chordae iter anterius) in the petrotympanic fissure. At the geniculate fossa, the facial canal turns posterior and lateral at an angle of 75 degrees or less, referred to as the anterior genu, to become the tympanic segment (Fig. 7.13 and Fig. 7.14A).11
The first major branch of the facial nerve exits the geniculate fossa anteromedially as the greater superficial petrosal nerve, courses through the facial hiatus, a small groove on the anterior surface of the petrous temporal bone, eventually to supply the lacrimal and nasal seromucus glands via the pterygopalatine ganglion.7 It additionally provides taste fibers to the palatal mucosa.24 The facial hiatus can occasionally be seen on axial high-resolution CT (HRCT) imaging as a small anteromedially oriented channel on the anterior surface of the superior temporal bone, arising in the region of the geniculate fossa (Fig. 7.13).35 Injury to this facial nerve branch may be manifested as an impairment of ipsilateral lacrimation.
|
A large air cell referred to as the anterior epitympanic (geniculate) sinus is related to the geniculate fossa and proximal tympanic facial nerve segment laterally. The lateral bony wall of the fallopian canal may be dehiscent in this location and must be surgically avoided. The relationships of the geniculate fossa are otherwise similar to those of the labyrinthine facial nerve segment, being separated from the vestibule and ampullae of the superior and lateral SCCs posteriorly by 3 mm of compact otic capsule bone. This location is a crossroad of four nerve canals: the labyrinthine segment of the facial nerve canal, the tympanic segment of the facial nerve canal, the facial hiatus containing the greater superficial petrosal nerve, and the accessory facial hiatus transmitting the lesser petrosal nerve.11,19,20,24,31
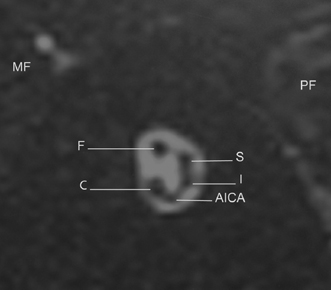
Fig. 7.12 This sagittal reconstruction of a three-dimensional T2-weighted sequence within the proximal internal auditory canal (IAC) demonstrates the vascular and neural structures of the normal cistern. The facial nerve is anterior and superior (F), the cochlear division of the vestibulocochlear nerve is anterior and inferior (C), and the vestibular nerve is posterior, just at the division of the superior (S) and inferior (I) branches. There is also an inconstant loop of the anterior inferior cerebellar artery (AICA) inferior in the IAC on this image. Proximity of the middle (MF) and posterior (PF) fossa are apparent.
The tympanic segment of the facial nerve is usually straight and measures ∼10 mm in length from its emergence from the geniculate fossa anteriorly to the posterior genu posteriorly.20 This segment of the facial canal courses along the superior portion of the medial wall of the mesotympanum. Anteriorly, the facial nerve lies lateral to the ampulla of the horizontal SCC. As it courses posteriorly the nerve assumes a position that is inferior to the plane of the horizontal SCC. The tympanic segment of the facial canal is readily visualized with either axial or coronal CT (Fig. 7.13, Fig. 7.14, Fig. 7.15, Fig. 7.16, Fig. 7.17, and Fig. 7.18). The cochleariform process from which the tensor tympani tendon emanates lies immediately inferior to the proximal tympanic segment. In the coronal plane, the cochleariform process, the proximal tympanic segment, and the distal labyrinthine segment may be visualized in close proximity on a single image. The normal nonprotruding middle portion of the facial canal runs superior to the oval window and inferior to the lateral SCC. Only 1 mm of bone separates the tympanic segment of the facial nerve canal from the vestibule and lumen of the horizontal SCC medially. The impression that the superior aspect of the tympanic segment makes on the lateral SCC is variable.
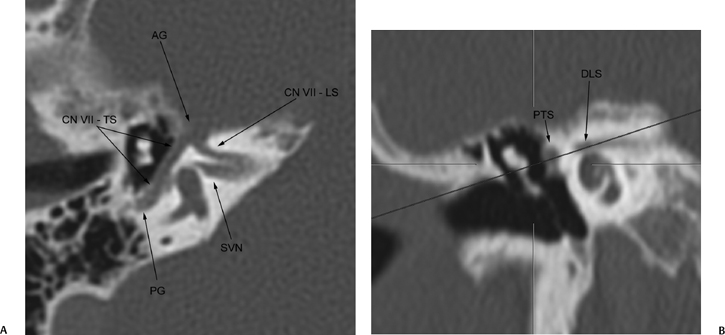
Fig. 7.14 (A) This slight oblique axial computed tomography reconstruction demonstrates continuity of the facial nerve from the fallopian canal to the posterior genu (PG). Continuity of the labyrinthine segment (CN VII – LS) and the tympanic segment (CN VII – TS) of the facial nerve is noted. The plane of section also depicts the superior vestibular nerve (SVN) adjacent to the vestibule. (B) Red line illustrates the plane of orientation to demonstrate the entire course of the labyrinthine and tympanic segment of the facial nerve. A coronal reconstruction at the level of the cochlea shows the distal labyrinthine segment of cranial nerve VII (DLS) and the proximal (PTS) in the “snake eyes” orientation.
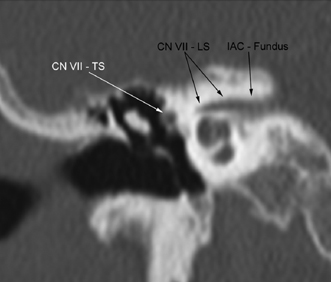
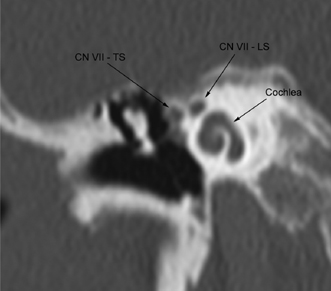
Fig. 7.16 Reconstructed coronal computed tomography image in the plane of the cochlea demonstrates the distal labyrinthine segment of the facial nerve (CN VII – LS) and the proximal tympanic segment of the facial nerve (CN VII – TS) as the “snake eyes” above the turns of the cochlea.
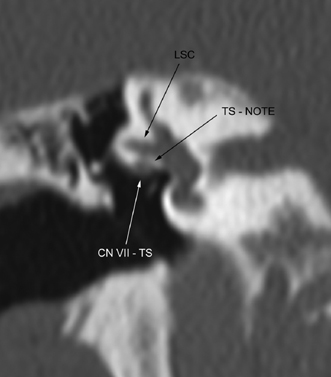
Fig. 7.17 Reconstructed coronal computed tomography image at the level of the oval window, depicting the lateral semicircular canal (LSC) and the tympanic segment of the facial nerve (CN VII – TS) immediately inferior to it. The tympanic segment is inconstantly encased in bone, and in this case, appears to have a deficient bony inferior covering. However, the depression of the nerve into the temporal bone is quite obvious (TS – NOTE).
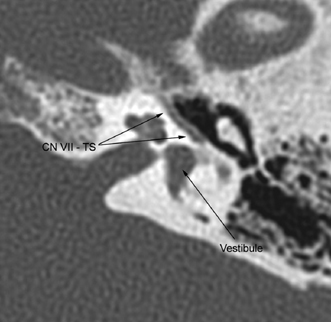
Fig. 7.18 Axial computed tomography image in the plane of the cochlea and vestibule demonstrates the continuous tympanic segment (CN VII – TS) of the facial nerve.
The tympanic segment of the facial nerve is densely concealed by bone only at its most anterior and posterior ends. In the middle two thirds, the bony wall adjacent to the middle ear is very thin and often cannot be resolved even with HRCT (Fig. 7.17).11 Focal areas of dehiscence may be present in up to 74% of temporal bones and are most common in the region of the oval window.6 Cholesteatoma and other complications of chronic otitis media may cause erosion of the canal in this location and thereby cause facial palsy. Also, the inferior surface of the tympanic segment may partially conceal the oval window.
As it extends posteriorly, the facial nerve is inclined slightly inferiorly, generally in the plane of the petrous pyramid, and courses obliquely from medial to lateral toward the posterior mesotympanum. The posterior tympanic segment courses immediately beneath the short process of the incus at the fossa incudis, where it begins its second turn inferiorly into the posterior tympanic wall to become the mastoid segment. The facial recess is immediately lateral to the facial canal in this location, and the stapedius muscle within the pyramidal eminence is immediately medial to it. The short process of the incus, sinus tympani, and pyramidal eminence all serve as useful landmarks of the posterior genu in the axial CT plane.
The posterior genu of the facial nerve canal between the tympanic and mastoid segments forms an angle of between 95 and 125 degrees (Fig. 7.19).20 The concavity of this turn lies in the posterosuperior aspect of the tympanic cavity in direct apposition to the ponticulus, a smooth bony ridge on the medial wall of the middle ear that defines the superior boundary of the sinus tympani and separates the oval window niche from the round window niche. Medially, the sinus tympani separates the facial nerve canal from the bony labyrinth overlying the posterior SCC.
The mastoid segment of the facial nerve extends 13 mm from the posterior genu to the stylomastoid foramen (Fig. 7.19 and Fig. 7.20). The jugular bulb lies medial to the mastoid segment of the facial canal. The medial aspect of the mastoid facial canal may be dehiscent within the jugular fossa or may be separated from it by 7 mm of bone or more. The distance between the mastoid segment and the jugular bulb is related not so much to the degree of mastoid pneumatization as to the size of the jugular bulb itself.12,20 It is in this location that the facial nerve may be compromised by erosive jugulotympanic paraganglioma involving the jugular fossa. Three millimeters or less may separate the proximal mastoid segment from the posterior tympanic annulus. Distally, or more inferiorly, there is more separation from the tympanic annulus. The mastoid segment can be readily identified on axial CT or MR section, again depending on the degree of mastoid pneumatization (Fig. 7.19, Fig. 7.20, and Fig. 7.21).11 Excessive pneumatization can make CT evaluation more difficult; however, following the course of the nerve on contiguous sections will usually identify its location. Identification is usually straightforward in the sclerotic or diploic mastoid.
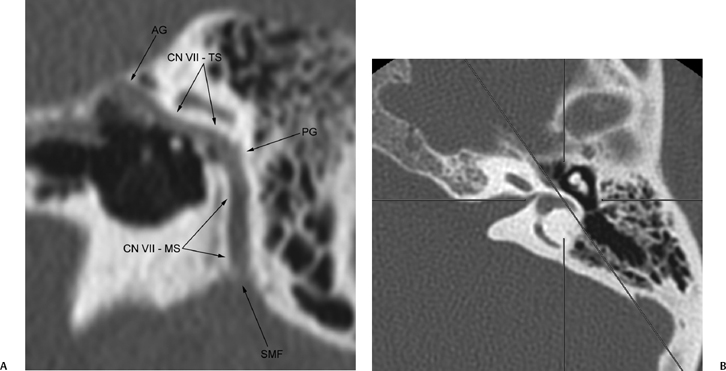
Fig. 7.19 (A) The reconstructions performed from the projection in (B) demonstrate the posterior genu of the facial nerve (PG) to advantage. On this oblique reconstruction, the facial nerve is depicted from the anterior genu (AG) to the stylomastoid foramen (SMF). The tympanic segment (CN VII – TS) and mastoid segment (CN VII – MS) are depicted in continuity. (B) Line illustrates the plane of orientation to demonstrate the entire course of the mastoid segment of the seventh cranial nerve (Fig. 7.15). The axis closely approximates the Stenvers’ projection along the long axis of the petrous temporal bone.
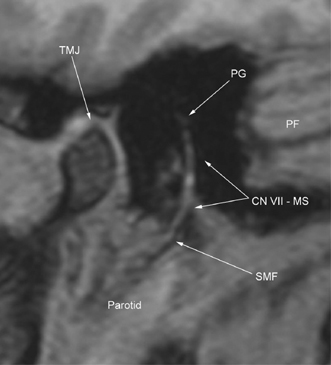

Fig. 7.21 Axial computed tomography image in the plane of the cochlea demonstrates the pyramidal eminence (PE) over the stapedius origin, with the sinus tympani (ST) anterior and the facial recess (FR) posterior in relation. The mastoid segment of the facial nerve (CN VII – MS) is depicted just inferior to the posterior genu. The cochlea and vestibule are evident in the otic capsule anterior and medial.
Two major branches emerge from the facial nerve along its mastoid segment, the stapedius nerve and the chorda tympani nerve (Fig. 7.10, Fig. 7.11). The stapedius nerve diverges from the facial nerve in the proximal mastoid segment to provide motor innervation to the stapedius muscle. Injury to this branch may result in hyperacusis. The chorda tympani nerve is the terminal branch of the nervus intermedius. It arises from the distal third of the mastoid segment and follows a redundant course upward and anteriorly through the canaliculus chordae tympani (iter chordae posterius) into the middle ear, where it crosses the middle ear cavity lateral to the long process of the incus and medial to the malleus, finally exiting the temporal bone at the petrotympanic fissure in the canal of Huguier.24,33,36 The origin of the nerve is usually 5 mm or so proximal to the stylomastoid foramen, although it can rarely arise from an extratemporal location.7,20 It carries afferent fibers for taste sensation from the anterior two thirds of the tongue and efferent parasympathetic secretomotor fibers to the submandibular, sublingual, and minor salivary glands in the floor of the mouth. Injury to this facial nerve branch causes loss of taste from the anterior two thirds of the tongue and atrophy of the ipsilateral submandibular and sublingual salivary glands.16
The stylomastoid foramen opens inferiorly between the mastoid process posterolaterally and the styloid process anterolaterally. Often, the facial nerve exiting the stylomastoid foramen into adjacent fat can be identified on axial CT or MR sections obtained a few millimeters inferior to the stylomastoid foramen.11,37,38 The extracranial facial nerve then delivers branches to the posterior belly of the digastric and the stylohyoid muscles as it courses anteriorly, inferiorly, and laterally to pierce the substance of the parotid gland to form the parotid plexus. Terminal branches to the numerous muscles of facial expression diverge from the parotid.39,40
The arterial supply to the facial nerve is provided by three vessels.33,41 The best known is the stylomastoid artery, a branch of the occipital or posterior auricular artery, which enters the facial canal via the stylomastoid foramen. This vessel primarily supplies the mastoid segment. A second vessel, the superficial petrosal artery, a branch of the middle meningeal artery coursing in the facial hiatus with the greater superficial petrosal nerve, supplies the tympanic segment. The internal auditory artery, a branch of the anteroinferior cerebellar artery from the basilar, supplies the intracanalicular and labyrinthine segments of this nerve. Rich anastomoses exist at the sites of overlap of these territories, which may play a role in the tendency of certain lesions, hemangiomas as an example, to occur at the junctions of these distributions.
Imaging of the Facial Nerve
All segments of the facial nerve canal within the temporal bone can be imaged with HRCT or MRI using proper technique.11,19,42–44 The intracranial segment of the facial nerve within the CPA cistern and IAC is now routinely noninvasively imaged with MRI.43 This evaluation has supplanted the use of intrathecally administered air or water-soluble contrast as a contrast agent in CT cisternography, rendering them as historical interest alone, although cisternography may rarely be used for the patient with MRI contraindications who requires imaging of the cisternal segment of the nerve.
Computed Tomography Delineation of the Normal Facial Nerve
Within the temporal bone, CT displays the facial nerve bony canal, whereas MRI shows the facial nerve itself. With CT, the long axis of the labyrinthine segment, the proximal tympanic segment, and the intervening geniculate fossa are best seen with contiguous axial sections (Fig. 7.13, Fig. 7.18, and Fig. 7.21), although occasional utilization of slight off-axis axial images may depict longer contiguous segments of the nerve (Fig. 7.14 and Fig. 7.19). The “snake eyes” of the paired distal labyrinthine segment and proximal tympanic segment may be visualized in cross section on coronal sections obtained at the level of the cochleariform process (Fig. 7.16). Coronal CT sections are also required for visualization of the tympanic segment in cross section and in identifying its relationship to the oval window. The posterior genu is equally well seen on both routine axial and coronal sections; however, oblique sagittal CT reformations reveal this genu to best advantage (Fig. 7.19). The mastoid segment of the facial nerve canal and stylomastoid foramen may be seen on axial CT, direct coronal CT sections, and oblique sagittal reformatted CT images (Fig. 7.19 and Fig. 7.21). With axial sections, one can identify this segment in cross section and discern its relationship to the external auditory canal and the jugular foramen.11,37,45
The extracranial facial nerve is first seen outlined by surrounding fat on sections just inferior to the stylomastoid foramen, unless this area is obliterated by inflammatory or neoplastic tissue.37,38,42 If perineural tumor from a parotid malignancy along the facial nerve is suspected, identifying a normal nerve trunk in the fat of the stylomastoid foramen clears the mastoid segment of involvement. The extracranial facial nerve within the parotid gland has never been satisfactorily demonstrated by CT or MRI.41
Magnetic Resonance Imaging Delineation of the Normal Facial Nerve
With MRI the normal facial nerve is readily visualized in the CPA cistern and the IAC using T1- or T2-weighted sequences, and with proper sequences (see below), can be separated from the other nerves with which it traverses these regions. The intratympanic segment can be visualized in either the axial or coronal plane, but it is more apparent following gadolinium administration (Fig. 7.22). The normal facial nerve, particularly the geniculate ganglion and the anterior tympanic segment, will often enhance to a mild to moderate degree due to the presence of a rich perivenous plexus surrounding the nerve in the fallopian canal and in the region of the geniculate ganglion. The CPA cisternal and intracanalicular segments and the extracranial facial nerve do not normally enhance.46 The posterior genu may be seen to best advantage with oblique sagittal images angled along the course of the tympanic segment of the facial nerve. The mastoid segment and stylomastoid foramen may also be seen on direct sagittal or coronal imaging. Axial nonenhanced T1-weighted magnetic resonance images (T1WIs) at the level of the stylomastoid foramen may display the main trunk of the facial nerve as a black dot surrounded by high signal fat. This image is very useful in excluding perineural tumor spread into the temporal bone along the mastoid segment of the facial nerve in cases where parotid malignancy is found. Beyond the stylomastoid foramen the facial nerve has not been convincingly and reproducibly visualized. Although MRI frequently demonstrates a low intensity linear structure on T1WIs on the axial plane within the parotid gland, this has been shown to represent the main intraglandular duct of the parotid gland rather than the intraparotid facial nerve.42,47
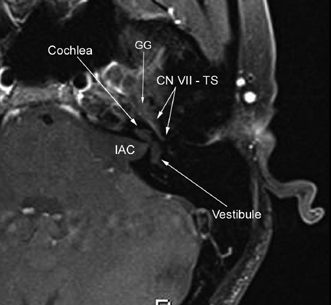
Fig. 7.22
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree