Jean Noel Buy1 and Michel Ghossain2
(1)
Service Radiologie, Hopital Hotel-Dieu, Paris, France
(2)
Department of Radiology, Hotel Dieu de France, Beirut, Lebanon
2.2.2 Broad Ligament
2.2.3 Peritoneal Masses
2.2.4 Extraperitoneal Masses
2.2.5 GI Tract Pelvic Masses
2.2.6 Urinary Pelvic Masses
2.2.7 Neurogenic Masses
2.2.8 Perineal Masses
2.2.9 Parietal Masses
Abstract
Diagnosis of the origin of a pelvic mass is one of the most common and difficult problems encountered in pelvic imaging.
Diagnosis of the origin of a pelvic mass is one of the most common and difficult problems encountered in pelvic imaging.
Precise location of the mass is one of the fundamental steps in the radiological diagnosis of a pelvic mass. A precise knowledge of the anatomy of the pelvis (topographic and descriptive) with anatomical sections in the different planes (axial, coronal and sagittal) is essential to localize precisely a pelvic mass and eventually according to the nature of the mass (especially in case of malignant tumor) to precise its extension. Knowledge of the anatomy can only be understood with a precise knowledge of embryology of the genital organs, the genital tract and the external female genitalia [1] but also of the peritoneum, and the urinary tract (mainly the ureters and the bladder), and of the GI tract (small bowel and colon and rectosigmoid) which can be involved in different pathologic processes of the gynecological organs.
The topographic diagnosis is different according to the exclusively or mainly cystic nature of the mass, or its mixed, mainly solid or exclusively solid nature.
2.1 Anatomy and Radioanatomy of the Pelvis and the Perineum
2.1.1 Female Genital Tract Is Situated in the Pelvis and in the Perineum
2.1.1.1 The Pelvis Is Limited By
Upward by the plane passing through the promontory of the sacrum, the arcuate line of the ilium, the iliopectineal line, and the posterior surface of the pubic crest.
Laterally, the pelvic wall formed above the arcus tendineus (which is a thickening of the aponeurosis of the internal obtuatus) by the obturator internus above, and the levator ani below.
Backward the piriformis covered by fascia over piriformis and the sacrum covered by the presacral fasciaDownward the pelvic floor is formed by the levator ani covered by the fascia of the pelvic diaphragm;Levator ani and coccygeus form the pelvic diaphragm and delineate the lower limit of the true pelvis.
2.1.1.2 The Perineum Is Limited By
Anteriorly, the pubic symphysis and its arcuate ligament
Posteriorly, by the coccyx.
Anterolaterally, the ischiopubic rami and the ischial tuberosities
Posterolaterally, the sacrotuberous ligaments
The deep limit of the perineum is the inferior surface of the pelvic diaphragm, its superficial limit the skin.
An arbitrary limit joining the ischial tuberosities divides the perineum into an anterior urogenital triangle and a posterior anal triangle.
Female genital tract is composed of:
1.
The ovary, which is only related by a thin mesovarium to the posterior part of the broad ligament and although entirely not covered by peritoneum, is considered as an intraperitoneal organ, because it lies in the peritoneal cavity.
2.
Derivatives of the Muller duct, which give rise to the tubes, the body of the uterus, the cervix, and the upper vagina (see Chap. 1), which lie under the peritoneum of the bottom of the pelvic cavity, and therefore are subperitoneal.
3.
The lower part of the vagina, which arises from the vaginal plate (see Chap. 1.1.3.1). During embryologic development this part will give rise to two portions:
An upper portion which migrates upward to fuse with the upper part of the vagina (which arises from the Muller duct). These two parts will form the subperitoneal segment of the vagina.
A lower portion under the hymeneal membrane which lies in the perineum and opens into the vestibule. This portion will form the perineal segment of the vagina.
These organs, intraperitoneal, subperitoneal, and perineal, present anatomical relationships with:
The extraperitoneal space lateral to the parietal pelvic peritoneum
The retroperitoneal space, mainly via lymphatic and nervous structures
Moreover, in radiological practice:
Masses of the female genital tract can be difficult:
To differentiate from extra female organs, GI tract, urinary tract, peritoneum, broad ligament, extraperitoneal, retroperitoneal nervous structures, and even in uncommon cases from parietal masses
To precisely locate as ovarian, tubal, uterine in origin, or in case of a double location contiguous or separated to precise the organ of origin
2.1.2 The Different Anatomical Spaces of the Female Genital Tract and Perineum
2.1.2.1 Definitions
Peritoneum [2]: a single layer of flattened mesothelial cells, lying on a layer of loose connective tissue
The mesothelium usually forms a continuous surface, but in some areas may be fenestrated; neighboring cells are joined by junctional complexes but probably permit the passage of macrophages.
The submesothelial connective tissue may contain macrophages, lymphocytes, and adipocytes (in some regions).
Mesothelial cells may transform into fibroblasts, which may play an important role in the formation of peritoneal adhesions after surgery or inflammation of the peritoneum.
Peritoneal cavity: a virtual space lying between the parietal peritoneum and the visceral peritoneum. It may contain physiologically a small amount of peritoneal fluid (<30 cc).
After ovulation, secondary to rupture of the dominant follicle, a little more of fluid is seen in the Douglas.
During menstruation, blood may escape from the uterine tubes into the pelvic peritoneal cavity.
Intraperitoneal organ: although not situated in the peritoneal cavity (between the two layers of peritoneum), an organ entirely (small bowel, appendix, cecum, sigmoid) or almost entirely covered with visceral peritoneum (like in the abdomen, liver, stomach, spleen).
Retroperitoneal organ: an organ situated behind the posterior parietal peritoneum.
Organ lying in the peritoneal cavity: an organ situated in the peritoneal cavity, almost entirely not covered by peritoneum like the ovary (but only connected to the posterior leaf of the broad ligament by the mesovarium).
Meso is composed of the apposition of twofolds of visceral peritoneum (except for the transverse mesocolon which has fourfolds, two from the foregut, two from the midgut).
Root of peritoneum is the area of reflection and attachment of the meso on the posterior parietal peritoneum.
Extraperitoneal tissue (transversalis fascia) separates the parietal peritoneum from the muscle layers of the abdominal wall.
2.1.2.2 The Different Anatomical Spaces
The Intraperitoneal Space
The intraperitoneal space containing the intraperitoneal segments of the GI tract, covered by visceral peritoneum:
1.
Small bowel attached by the mesentery to the posterior parietal peritoneum along its root extending from the duodenojejunal junction to the ileocecal junction
2.
Cecum usually suspended by a short mesentery and appendix with its short mesoappendix connecting it to the lower part of the ileal mesentery
3.
Sigmoid with the mesosigmoid connected to the posterior parietal peritoneum by its two roots:
The primary root from the inferior angle of the aorta bifurcation to the posterior junction of the rectosigmoid junction
The secondary root from the origin of the primary one, descending obliquely along the primitive and external left iliac artery
The Subperitoneal Space
The Roof: The Broad Ligament (Figs. 2.1, 2.2, and 2.3)
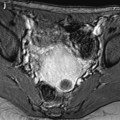
Fig. 2.1
Anterior view of the broad ligament. 1 Uterus, 2 cervix, 3 vagina, 4 left ovary, 5 utero-ovarian ligament, 6 tube with its infundibulum, 7tubo-ovarian ligament, 8 Morgagni hydatid, 9round ligament, 10 broad ligament with its anterior (a), middle (b), and posterior (c) wings; 11 posterior leaf of the broad ligament, and 12 infundibulopelvic ligament
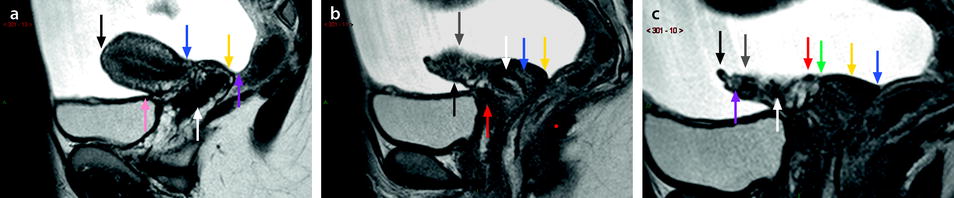
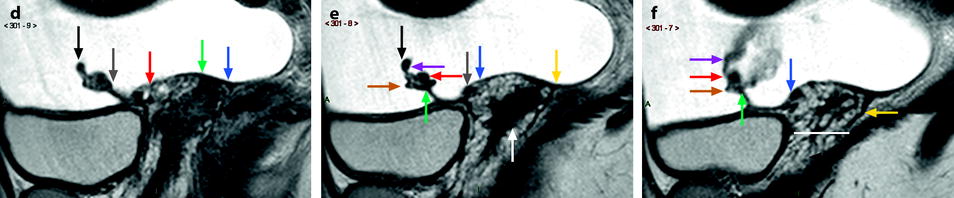
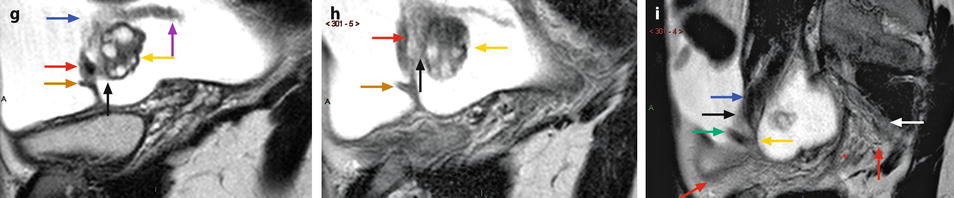
Fig. 2.2
Landmarks: Contiguous sagittal sections of the broad ligament from the midline (black landmark) to the left pelvic wall (purple landmark) (cervix in the middle sagittal plane, uterus body oriented to the right) (last figure with bars). (a) Section through the middle sagittal plane of the uterus body (black landmark). Uterus body (between black arrow and blue arrow), right paracervix (between blue and yellow arrows), right vaginal wall (white arrow), vesicouterine pouch (pink arrow), Douglas (purple arrow). (b) Section at the junction of the left lateral border of the uterus and the mesometrium (red landmark). Myometrium (black arrow), mesometrium (gray arrow), cervix inner stroma (white arrow), external stroma (blue arrow), vesicouterine septum (red arrow), posterior fornix of the vagina (yellow arrow). (c) Section through the inner mesometrium (green landmark). Mesosalpinx (between black and gray arrows) containing the medial branch of the tubal artery (black arrow), the tube (purple arrow). Mesometrium above the Mackenrodt’s ligament (between gray and red arrows) containing vessels particularly the ascending segment of the uterine artery (white arrow). Uterine artery (red arrow) at the junction of Mackenrodt’s ligament and mesometrium. Mackenrodt’s ligament (between red and green arrows). External cervix lateral stroma (yellow arrow), posterior fornix of the vagina (blue arrow). (d) Section through the inner Mackenrodt’s ligament (purple landmark). Mesosalpinx (between black and gray arrows), mesometrium above the Mackenrodt’s ligament (between gray and red arrows), Mackenrodt’s ligament (between red and green arrows), posterior fornix of the vagina (blue arrow). (e) Section just lateral to the previous one (yellow landmark). Mesosalpinx (between black and green arrow), containing medial tubal artery (purple arrow), and uterine artery (red arrow), round ligament containing its artery (brown arrow), mesometrium above the Mackenrodt‘s ligament (between green arrow and blue arrow). Uterine artery in its latero uterine segment (gray arrow), Mackenrodt’s ligament (between blue and yellow arrows), vagina lateral wall (white arrow). (f) Section at the level of the medial face of the ovary (brown landmark). Mesosalpinx with anastomoses between uterine and ovarian arteries (red arrow), tubal artery with a low signal (purple arrow) along the tube. Round ligament (brown arrow) containing its low signal artery. Mesometrium between the green arrow and the blue arrow. White line at the level of the lower part of the cervix. Mackenrodt’s ligament between the blue arrow and the yellow arrow, above the white line. Below the white line, paravaginal subperitoneal tissue (black arrow) Fig. 2.2 (continued) (g) Section through the middle part of the ovary at the level of change in direction of the salpinx (orange landmark). Round ligament (brown arrow), mesosalpinx containing uterine artery (red arrow), mesovarium (black arrow), ovary (yellow arrow), tube with ampullary portion (blue arrow) and infundibulum (purple arrow). (h) Section through the mesovarium (gray landmark). Infundibulopelvic ligament contains ovarian artery (red arrow), mesovarium (black arrow), ovary lateral third (yellow arrow), round ligament (brown arrow). (i) Section through the junction of the lateral part of the broad ligament and the extraperitoneal space (white landmark). Medial part of the extraperitoneal space (blue arrow) containing the left external iliac vein. Anterior (black arrow) and posterior (yellow arrow) peritoneal leaves of the mesometrium close to their attachment to the extraperitoneal space. Round ligament at the beginning of its extraperitoneal segment (green arrow). Anterior and posterior subperitoneal spaces (between red arrows). Retroperitoneal space (white arrow). (j) Section through the extraperitoneal space (Bordeaux red landmark). Anterior subperitoneal space (between green arrow and anterior red arrow), extraperitoneal space (between red arrows), retroperitoneal space (between posterior red arrow and purple arrow), external iliac artery and vein (white arrow), arterial and venous branches of the hypogastric artery and vein (yellow arrow)
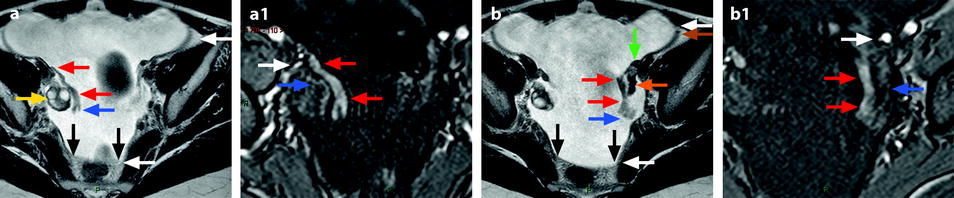
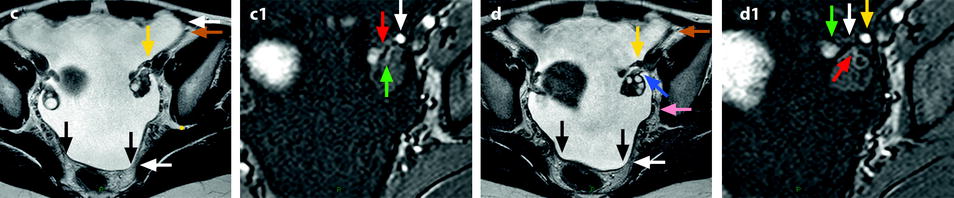
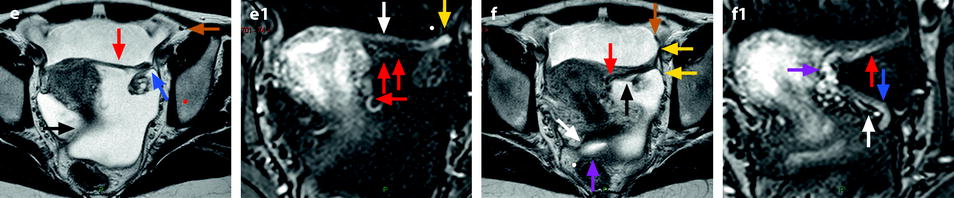
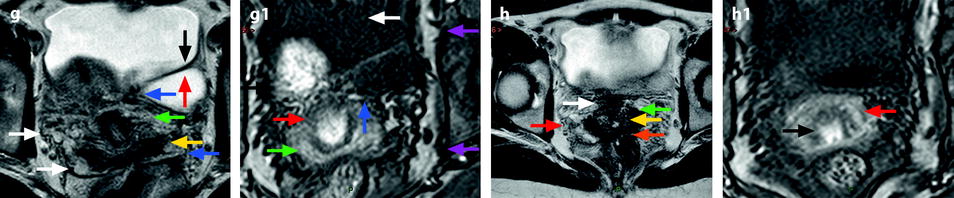
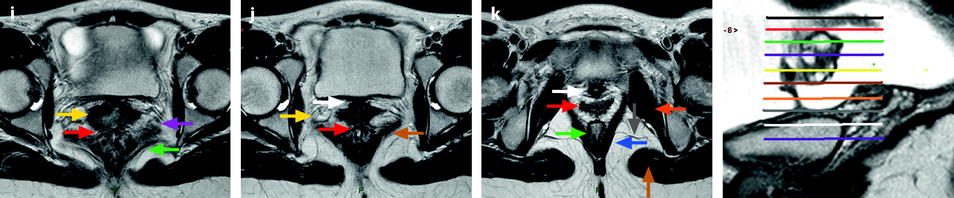
Fig. 2.3
Landmarks: Contiguous axial sections of the broad ligament from the top (black landmark) to the pelvic floor (lower purple landmark) using axial T2 and DMR (at the arterial phase) sequences at the same level (last figure with bars). (a) Section (axial T2), through the right adnexa (black landmark). Right ovary (yellow arrow), right tube ampulla (between red arrows), infundibulum (between the more distal red arrow and blue arrow). Extraperitoneal space (between white arrows), retroperitoneal space (between black arrows). (a1) Same section (DMR, arterial phase): right ovarian artery (white arrow) and intraovarian branches (blue arrow), tubal arteries (red arrows). (b) Section (axial T2) through the left adnexa (red landmark): infundibulo pelvic ligament containing the low signal intensity ovarian artery (green arrow), left superior ovarian cortex (orange arrow), left tube ampulla (between red arrows) infundibulum (between the more distal red arrow and blue arrow). Extraperitoneal space (between white arrows), retroperitoneal space (between black arrows). Round ligament (brown arrow). (b1) Same section (DMR, arterial phase): left ovarian artery (white arrow) and intraovarian branches (blue arrow), tubal arteries (red arrows). (c) Section (axial T2) through both adnexa (green landmark). Left infundibulopelvic ligament containing the ovarian artery (yellow arrow). Extraperitoneal space (between white arrows), retroperitoneal space (between black arrows). Round ligament (brown arrow). (c1) Section (DMR, arterial phase): left ovarian artery (white arrow) and intraovarian branches (green arrow), lateral tubal artery (red arrow). (d) Section (axial T2) (purple landmark) junction between the isthmus and the ampulla. Ovarian artery (yellow arrow) mesovarium with lateral leaf in continuity with the posterior leaf of the parietal pelvic peritoneum (blue arrow) uterine artery in its extraperitoneal segment (pink arrow). Retroperitoneal space (between the two black arrows), junction between the retroperitoneal space and the extraperitoneal space (white arrow), round ligament (brown arrow). (d1) Section (DMR, arterial phase): ovarian artery (yellow arrow) lateral tubal branch of the ovarian artery (white arrow) anastomosis between ovarian artery and tubal artery (green arrow), intraovarian arteries (red arrow) Fig. 2.3 (continued) (e) Section (axial T2) (yellow landmark). Round ligament at the beginning of its extra peritoneal location (brown arrow). Isthmic portion of the tube and mesosalpinx in its superior portion (red arrow), mesovarium (blue arrow), right uterosacral ligament (black arrow). (e1) Section (DMR, arterial phase). Uterine artery: ascending segment in the mesometrium along the lateral border of the uterus body (horizontal red arrow), uterine artery in the mesosalpinx (vertical red arrows), medial tubal branch (branch of division of the uterine artery in the superior portion of the mesosalpinx) (white arrow). Terminal portion of the uterine artery in the mesosalpinx (yellow arrow) anastomosing with the ovarian artery. (f) Section (axial T2) through the ovarian ligament (brown landmark). Ovarian ligament indicating the inferior part of the mesosalpinx (black arrow), uterine artery in the mesosalpinx (red arrow), round ligament in its proximal portion (brown arrow), anterior and posterior leaves of the broad ligament joining the lateral parietal peritoneum (yellow arrows), right uterosacral ligament (white arrow), Douglas (purple arrow). (f1) Section (DMR, arterial phase): uterine artery in its transverse segment (white arrow) at its ascending segment (purple arrow) in the mesosalpinx (red arrow), superior uterine vein lateral and below the transverse segment of the uterine artery (blue arrow), ureter crosses between uterine artery and vein, not visualized on this sequence. (g) Section (axial T2) (orange landmark), anterior (black arrow) and posterior (red arrow) leaves of the mesometrium clearly defined by fluid in the peritoneal cavity containing the low signal intensity of the round ligament, Mackenrodt’s ligament (between blue arrows) with its paracervical portion (green arrow) and paravaginal portion lateral to the fornix (yellow arrow). On the right side lateral limit between Mackenrodt’s ligament and the extraperitoneal space (white arrows). (g1) Section (DMR, arterial phase): fluid in the peritoneal cavity (white arrow); artery of the round ligament just behind white arrow. Transverse segment of the uterine artery (blue arrow), intrauterine arteries (black arrow), cervical arteries (red arrow), vaginal arteries (green arrow), arteries of the extraperitoneal space (between purple arrows). (h) Section (axial T2) (gray landmark) through the lower part of the Mackenrodt’s ligament: uterovesical septum (white arrow), lateral fornix (green arrow), lower part of the cervix (yellow arrow), junction of the Mackenrodt’s ligament and the extraperitoneal space (red arrow), rectovaginal septum (orange arrow). (h1) Section (DMR, arterial phase): cervical arteries (black arrow), vaginal arteries (red arrow). (i) Section (axial T2) (white landmark): uterovesical septum (black arrow), vaginal wall (yellow arrow), rectovaginal septum (red arrow), paravagina (purple arrow), iliococcygeus muscle (green arrow). (j) Section through the top of the rectovaginal septum (lower purple landmark), vesicovaginal septum (white arrow), paravagina (yellow arrow), rectovaginal septum (red arrow), iliococcygeus muscle (brown arrow). (k) Section through the lower part of the subperitoneal space just above the pelvic floor, urethra (white arrow), vagina (red arrow), lower part of the rectum (green arrow) just above the rectoanal junction, iliococcygeus muscle lower part (blue arrow) just above the puborectal muscle, obturator internus (orange arrow), gluteal maximus (brown arrow), posterior perineum:ischiorectal fossa (gray arrow)
Peritoneal Folds
1.
Mesosalpinx (Fig. 2.4a–c)
Fig. 2.4
(a) 1 tube, 2 mesosalpinx, 3 ovary, 4 mesovarium, 5 mesometrium. (b) 1 Ovary, 2 Tuboovarian ligament, 3 Ovarian ligament, 4 Uterus, 5 Rectum, 6 Tube with 6’ isthmus, 6’’ ampulla, 6’’’ infundibulum, 7 Suspensory or Infundibulopelvic ligament containing in its thickness the ovarian artery and vein and lymphatics, 8 Mesometrium, 8’ Mesosalpinx, 9 Uterine artery, 10 Sacral plexus, 11 Ureter, 12 Internal iliac vein Fig. 2.4 (continued) (c) 1 Uterus, 2 Tube intramural segment, 3 Tube with 3’ Isthmic portion, 3’’ Ampulla, 4 Infundibulum, 5 Ovarian fimbria, 6 Ovary, 7 Tuboovarian ligament, 8 Ovarian ligament, 9 Mesometrium with, 10 posterior leaf, 11 Mesosalpinx. (d) 1 Posterior leaf of the mesosalpinx, 2 Ovary with 3 De Graaf’s follicles, 4 Scars, 5 Ampulla, 6 infundibulum with two concentric circles of fimbriae, 7 Ostium abdominale, 8 Ovarian fimbria with 8’ its longitudinal gutter, 9 Tuboovarian ligament in continuity with the longitudinal gutter of the ovarian fimbria, 10 Epoophoron
It covers the tube except the fimbriae of the tubal infundibulum which project from its free lateral end into the peritoneal cavity.
It is attached laterally to the suspensory ligament of the ovary and medially to the ovarian ligament.
It contains vascular anastomoses between the uterine and ovarian vessels, the epoophoron (Fig. 2.4d), the paroophoron, and the proximal part of the Gartner canal.
2.
Mesovarium (Fig. 2.4a–c)
It projects from the lower and lateral part of the posterior fold of the mesosalpinx to the hilum of the ovary. All the rest of the ovary is devoid of peritoneum.
It carries vessels and nerves to the ovary.
The ovarian ligament attaches the inferomedial extremity of the ovary to the lateral angle of the uterus posteroinferior to the uterine tube. The ovarian ligament is continuous with the medial border of the round ligament.
The upper pole of the ovary is connected to the posterior part of the infundibulum of the tube by the tubo-ovarian ligament.
3.
Mesometrium or Parametrium of Virchow (3) (Figs. 2.4a, b and 2.5)
Fig. 2.5
Coronal section through the middle of the broad ligament. 1 Mesometrium, 2 paracervix, 3 paravagina, 4 uterine artery, 5 ureter, 6 levator ani
It is the largest part of the broad ligament.
(a)
It is limited by:
Upward, the lower part of the mesosalpinx.
Downward, the subperitoneal tissue covering the pelvic floor.
Medially, the lateral border of the uterus and the vagina until the introitus.
Laterally, upward the suspensory or infundibulopelvic ligament, which is attached to the upper part of the lateral face of the ovary; below this ligament.
Forward the anterior peritoneal fold:
Medially, descends on the anterior face of the uterus body until the isthmus, reflects onto the bladder forming the uterovesical fold
Laterally, is heightened by the proximal part of the round ligament which inserts on the uterus just below the uterine tube
Backward, the posterior peritoneal fold descends over the posterior face of the uterus body, the upper cervix, the posterior fornix until the lower border of the posterior lip of the exocervix then reflects on to the front of the rectum to form the Douglas pouch.
(b)
It contains:
Loose connective tissue and smooth muscle
The uterine artery
The ureter
1.
Uterovesical fold at the level of the isthmus (Fig. 2.6) The continuum with the anterior parietal peritoneum raised by:
Fig. 2.6
Sagittal view through the middle part of the uterus. 1 Vesicovaginal cul de sac, 2 vesicovaginal septum, 3 Douglas pouch, 4 rectovaginal septum, 5 rectum
On the midline, the median umbilical ligament (obliteration of the lumen of the urachus, derivative of allantois) (see Chap. 1.1.1)
Laterally, the medial umbilical folds over the obliterated umbilical arteries
2.
Douglas pouch:
The top is at the level of the torus (Fig. 2.6:1121 p 353).
The anterior leaf covers the posterior part of the cervix, than reflects over the posterior fornix.
The bottom is at the level of the inferior border of the posterior lip of the cervix.
The posterior leaf reflects over the anterior and lateral borders of the rectum until the rectosigmoid junction.
The lateral parts (called the ring of Waldeyer) are arciform heightened by the subperitoneal uterosacral ligaments.
Ligaments
1.
Round Ligament (Fig. 2.1)
As the ovarian ligament with which it is continuous, the round ligament is issued from the gubernaculum of the embryo (see Chap. 1).
Near the uterus, it contains much smooth muscle, which progressively diminishes until the terminal part which is purely fibrous
1.
In the Mesometrium
It starts from the uterus body just below and anterior to the lateral cornua.
It passes diagonally down and laterally within the mesometrium.
2.
It crosses the obturator nerve and vessels, the obliterated umbilical artery.
Just before the deep inguinal ring, it passes over the epigastric artery.
3.
It traverses the inguinal canal.
4.
It terminates on the mons pubis.
2.
Uterosacral Ligaments (Fig. 2.7)
Fig. 2.7
Frontal view of the posterior part of the broad ligament. 1 Uterus, 2 rectum, 3 external iliac vessels, 4 internal iliac vessels, 5 utero-ovarian vessels, 6 uterine artery, 7 ovary and tube, 8 ureter, 9 uterosacral ligaments, 10 Douglas, 11 obturator artery, 12 vesicovaginal artery, 13 bladder
They arise from the posterior surface of the cervix on both sides of a little transverse protrusion the torus uterinus. The ligaments go backward around the lateral faces of the rectum and are attached to the front of the sacrum. They constitute the roof of the sacrorectovaginal septum. They contain fibrous tissue and smooth muscle.
3.
Ligaments of Mackenrodt (Fig. 2.5)
It is limited by:
The superior part of the cervix with the transverse segment of the uterine artery immediately below Inferiorly: the inferior border of the lateral fornix of the vagina
Medially: lateral wall of the uterine cervix, lateral fornix of the vagina
Laterally: is continuous externally with the fibrous tissue which surrounds the pelvic blood vessels of the pelvic wall.
Forward: the supravaginal part of the cervix is
Backward: the uterosacral ligaments
It contains:
The ureter crossing the inferior part of the transverse segment of the uterine artery, the uterine vein (superior and lateral branch as it passes below the ureter, above the vaginal artery)
Cervicovaginal artery, superficial and deep uterine veins
Lymphatics
4.
Pubocervical Ligament
From the anterior part of the cervix and the upper vagina, diverge around the urethra attach to the posterior aspect of the pubic bones.
The Floor
The Levator Ani (See Figures Chap. 37)
Comprises two parts: a superolateral part, the iliococcygeus muscle; and an inferomedial part, consisting of the puborectalis and the pubovisceralis
1.
Get Clinical Tree app for offline access

A superolateral part: the iliococcygeus muscle
(a)
Origin: the ischiatic spine; the arcus tendineus, which is a thickening of the obturator fascia covering the medial and upper part the obturator internus muscle (a little lower than its superior border) extending from the ischiatic spine behind, running along the inferior border of the obturator canal, to the body of the pubis in front.
The pubis body is 1 cm lateral to the pubic symphysis and 5 mm above its lower border
(b)
Direction: its general direction is inward and downward; its inferior and medial attachment is on the horizontal puborectalis.
(c)




End: The more anterior fibers intersect with those of the opposite side forming sort of a strap around the 3/4 posterior of the rectum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree