Jean Noel Buy1 and Michel Ghossain2
(1)
Service Radiologie, Hopital Hotel-Dieu, Paris, France
(2)
Department of Radiology, Hotel Dieu de France, Beirut, Lebanon
8.1.1 Work-Up for Infertility
8.1.2 Biological Findings
8.2.1 Ovulation Disorders
8.2.3 Endometriosis
8.2.4 Periovarian Adhesions
Abstract
Infertility is defined as 12 months or more of unprotected intercourse without pregnancy. It is primary when there is no previous pregnancy. It is secondary when fertility problems occur in a couple that has conceived on their own and had a child in the past. A standard infertility evaluation is made with a series of test [1] which are reported in Table 8.1.
Infertility is defined as 12 months or more of unprotected intercourse without pregnancy. It is primary when there is no previous pregnancy. It is secondary when fertility problems occur in a couple that has conceived on their own and had a child in the past. A standard infertility evaluation is made with a series of test [1] which are reported in Table 8.1.
Table 8.1
Diagnostic evaluation of infertility
1. Male factor (semen analysis) |
2. Ovulatory and luteal function (serum progesterone) |
3. Cervical factor (postcoital test (PCT)) |
4. Uterine factor (HSG and/or hysteroscopy, ultrasound) |
5. Tubal factor (HSG and coelioscopy) |
6. Endometriosis or other pelvic pathology (coelioscopy) |
Female infertility after 35 years old increases with age. The most common causes are ovulation problem, followed by tubal problems (previous PID, previous tubal pregnancy). More uncommonly it may be related to abnormal function of the hypothalamic-hypophyseal axis, to adrenal dysfunction, to metabolic disease, and to multiple pelvic disorders which can involve the different compounds of the Muller duct and the secondary Mullerian system. Moreover, in some of these entities like in PCOD, different factors can be associated. In some cases, the cause of infertility is unexplained.
Etiological diagnosis of infertility is mainly based on clinical and biological findings. However, imaging modalities, particularly ultrasound, occupy an important place in the detection and characterization of a pathologic process of the pelvic organs. This modality is also particularly appropriate to evaluate the ovarian function. MR can provide additional informations in the evaluation of infertility.
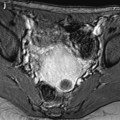
Ovarian infertility is related to three different causes: ovulation disorders which may be related to ovarian or to hypothalamic and hypophyseal dysfunction or endocrine disorders, endometriosis in which the factors responsible for sterility are multiple, and periovarian adhesions. When ovarian infertility is suspected, the first step in the work-up is to evaluate the ovarian reserve.
8.1 Evaluation of Ovarian Reserve
8.1.1 Work-Up for Infertility
Evaluation of ovarian reserve is part of every work-up for infertility. It is made at day 3 of the menstrual cycle and comprises day-three blood test and an antral follicle count with endovaginal sonography (Table 8.2).
Table 8.2
Ovarian reserve screening tests
Biological findings at day 3 |
FSH (normal <10 mIU/ml) |
Estradiol (E2) (normal 25–75 pg/ml) |
AMHa (normal between 1 and 3 ng/ml) |
US findings at day 3: antral follicle count (AFC) (between 2 and 8 mm) |
8.1.2 Biological Findings
FSH >10 mIU/ml or normal FSH associated with an elevated estradiol level indicates a reduced ovarian reserve. A level >20 is usually correlated with a very poor response to stimulation. However, a significant number of woman with normal FSH have a reduced egg supply.
AMH blood level is thought to reflect the size of the remaining egg supply or ovarian reserve. A low level <1 ng/ml expresses a decrease of this reserve. With increasing female age, the size of their pool of remaining microscopic follicle decreases. Likewise their blood AMH levels and the number of ovarian antral follicles visible on ultrasound decrease. Women with many small follicles such as PCOD have high AMH, and women who have few remaining follicles have low levels of AMH. However, AMH levels do not reflect egg quality.
8.1.3 Basal Antral Follicle Count
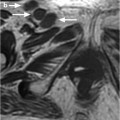
The basal antral follicle count test is a transvaginal ultrasound test that measures a woman’s ovarian reserve, or her remaining egg supply. The ovarian reserve reflects her fertility potential.
The basal antral follicle count, along with the woman’s age and cycle day 3 blood work levels, is considered one of the best indicators for estimating ovarian reserve and the woman’s chance for pregnancy with in vitro fertilization. The antral follicles are a good predictor of the number of mature (dominant) follicles in woman’s ovaries that can be stimulated by medications leading up to IVF.
The results of basal antral follicle count and correlation with response to stimulation are reported in Table 8.3.
Table 8.3
Antral follicle count
<4 | Extremely low count | Very poor response to stimulation |
4–6 | Low count | Poor response to stimulation drug |
7–10 | Reduced count | Higher than average rate of IVF cancelation |
11–15 | Intermediate count | Response to stimulation usually adequate |
Good count | ||
16–30 | Normal antral count | Excellent response to stimulate |
>30 | High count | Risk of overstimulation |
8.2 Causes of Ovarian Infertility
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree