Jean Noel Buy1 and Michel Ghossain2
(1)
Service Radiologie, Hopital Hotel-Dieu, Paris, France
(2)
Department of Radiology, Hotel Dieu de France, Beirut, Lebanon
30.1 Cysts
30.1.1 Clinical Findings
30.1.2 Frequency and Location
30.1.3 Pathology
30.1.4 Imaging Findings
30.2 Benign Neoplasms
30.2.1 Papilloma
30.2.2 Condylomata Acuminata
30.2.4 Leiomyoma
30.2.5 Benign Mixed Tumors
30.3 Malignant Neoplasms
30.3.1 Epidemiology
30.3.2 The Risk Factors
30.3.3 Histopathology
30.3.4 Symptoms of Vaginal Cancer
30.3.5 Classical Examination
30.3.6 Site and Staging
30.4 Other Pathologies
30.4.1 Vaginal Endometriosis
30.4.2 Vaginal Fistulas
30.4.3 Hematocolpos
30.4.4 Urethral Diverticula
Abstract
They are often incidental findings on MRI or ultrasound. They are usually asymptomatic but can grow to reach large size, protrude into the vagina, and cause symptoms.
30.1 Cysts
30.1.1 Clinical Findings
They are often incidental findings on MRI or ultrasound. They are usually asymptomatic but can grow to reach large size, protrude into the vagina, and cause symptoms.
30.1.2 Frequency and Location
Vaginal cysts can be congenital (Müllerian cysts or Gartner’s cyst) or acquired (squamous inclusion cysts). The most frequent are Müllerian and squamous inclusion cysts followed by Gartner’s cysts [1–3].
Congenital cysts are of paramesonephric origin (Müllerian cysts) or mesonephric origin (Gartner’s cyst). Both are located in the anterior-lateral wall of the vagina along the corresponding ducts. When higher situated, they are in the lateral wall of the vagina; at lower level, they are closer to the midline. The same cyst can be seen extending from the anterior midline inferiorly to the lateral wall posteriorly [4]. When large, they can protrude posteriorly in the ischiorectal fossa [5].
Acquired cysts are squamous inclusion cysts (also known as epithelial inclusion cyst, epidermal inclusion cysts). They are secondary to trauma and thus are mostly located at the site of episiotomy posterolaterally.
30.1.3 Pathology
30.1.3.1 Müllerian Cysts (Paramesonephric Cysts)
Some may be derived from islands of adenosis. They are usually less than 2 cm. They may be lined by any of the epithelia of the Müllerian duct, including endocervical type (most commonly), endometrial, and ciliated tubal type. Squamous metaplasia may be present.
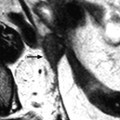
30.1.3.2 Gartner’s Duct Cysts (Mesonephric Cysts) (Figs. 30.1, 30.2, and 30.3)
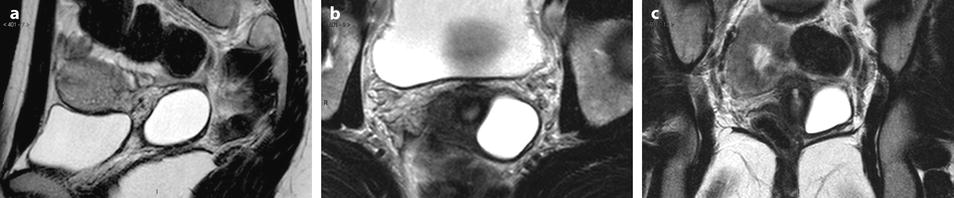
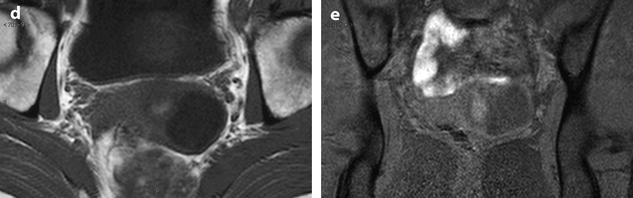
Fig. 30.1
Gartner‘s cyst. Twenty-three-year-old woman with slight dyspareunia. At speculum examination: swelling on the lateral wall of the vagina. MR sagittal T2 (a), coronal T2 (b), axial T2 (c), axial T1 (d), and coronal T1 with fat suppression (e). Four centimeter subperitoneal cyst on the left lateral wall of the cervix with a low signal on T1 and T1 with suppression, and a high signal on T2 related to a serous content. Prospective diagnosis based on location: Mullerian or Gartner’s cyst. At operation: the cyst is in the wall of the left vaginal cul de sac. At pathology the cyst lies in the stroma. Its lining is a flat or cuboidal non-mucinous epithelium (Gartner’s cyst)

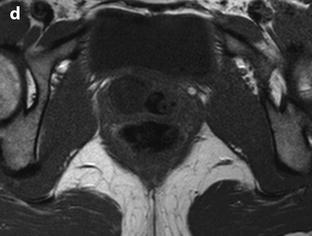
Fig. 30.2
Gartner’s cyst. Axial (a), sagittal (b), and coronal (c) T2W images, and axial T1W image (d), without vaginal opacification, show a unilocular cyst in the right lateral wall of the midportion of the vagina. Signal intensity is identical to urine on T1 and T2W images (arrows)
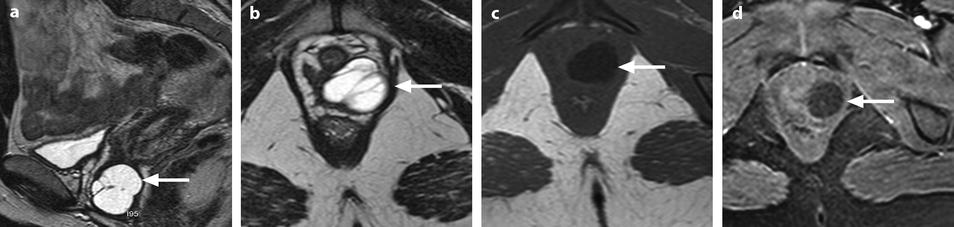
Fig. 30.3
Multilocular Gartner’s cyst. (a, b) Sagittal (a) and axial (b) T2W images show a hyperintense multilocular cystic mass (arrows) with thin regular septa located along the anterolateral wall of the middle third of the vagina. (c, d) Axial T1W image (c) and axial T1W-FS image after gadolinium injection do not show nodular contrast enhancement inside the cyst (arrows)
They are lined by low cuboidal non–mucin–secreting cells
30.1.3.3 Squamous Inclusion Cysts (Also Known as Epithelial Inclusion Cyst, Epidermal Inclusion Cysts)
These cysts arise from entrapment of vaginal mucosa as a result of surgery (episiotomy, obstetrical trauma, or vaginoplasty) or injury.
They are often asymptomatic.
The central content is keratin from desquamated cells. Size ranges from a few millimeters to several centimeters.
30.1.4 Imaging Findings
All these cysts are thin walled with no internal contrast enhancement or internal color Doppler flow. Differentiation between different types could be suggested by their location but not by their internal patterns (see Sect. 30.1.2) (Figs. 30.1, 30.2, and 30.3). As these cysts are usually asymptomatic and not operated, definite histological diagnosis is often missing (Figs. 30.4, 30.5, and 30.6).
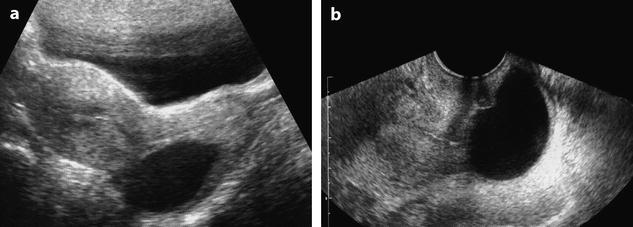
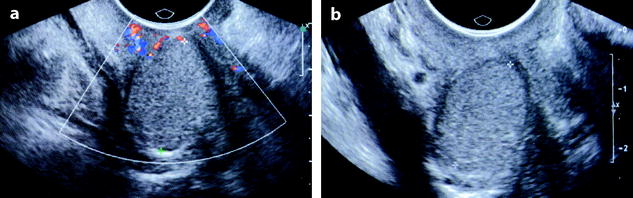
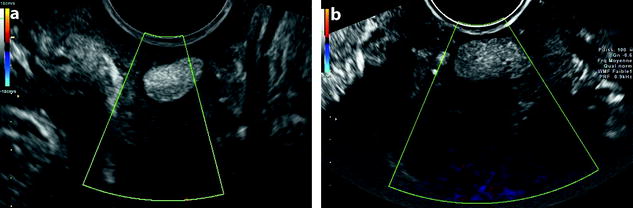
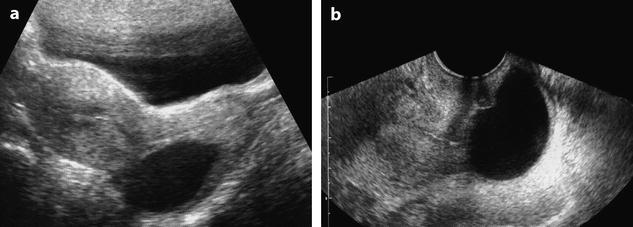
Fig. 30.4
Posterior vaginal cyst in an asymptomatic woman. (a, b) Transabdominal (a) and transvaginal (b) ultrasound disclose a posterior vaginal cyst with some internal echos. The cyst was stable on follow-up. As surgery was not performed definite histological diagnosis could not be made but the posterior location of the cyst favors a squamous inclusion cyst
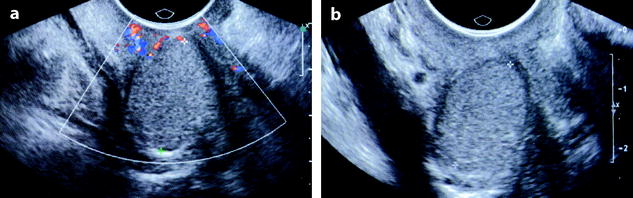
Fig. 30.5
Vaginal cyst. Posterior vaginal mass at clinical examination in an asymptomatic woman. Transvaginal ultrasound (a, b) discloses a hyperechogenic homogeneous mass of the vagina, avascular on color Doppler study. The mass was stable on follow-up. As surgery was not performed definite histological diagnosis could not be made but the posterior location of the mass and the absence of vascularization on color Doppler favors an inclusion cyst
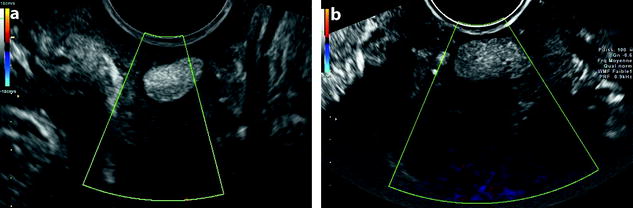
Fig. 30.6
Vaginal cyst. Anterior vaginal cyst in a 42-year-old asymptomatic woman. (a, b) Transvaginal transverse ultrasound with color Doppler discloses a hyperechogenic homogeneous cystic mass of the anterior wall of the vagina at the junction of the upper third and the middle third of the vagina, measuring 20 mm in diameter. The cyst was stable on follow-up. As surgery was not performed definite histological diagnosis could not be made but the anterior location of the cyst favors a congenital cyst (Mullerian or Gartner’s by order of frequency)
30.2 Benign Neoplasms
Benign solid tumors of vagina arise from vaginal connective tissue such as fibrous muscle, smooth muscle, and skeletal muscle tissues.
30.2.1 Papilloma
Definition: A papillary frond with a central fibrovascular core
Location: Near the hymeneal ring
Aspect: Most commonly clusters
Size: Only a few milliliters
They arise in the wall of the vagina, and the majority occurs early in childhood, before 10 years of age with vaginal bleeding. The clinical findings can mimic those of malignant lesions such as sarcoma botryoides and adenocarcinoma.
30.2.2 Condylomata Acuminata
In order of frequency, they arise in the vulva then the vagina then the cervix, and can be exophytic or less commonly maculopapular almost flat (See Chap. 27, Sect. 27.1.2 and Chap. 35, Sect. 35.2.3).
30.2.3 Fibroepithelial Polyp or Mesodermal Stromal Polyp
Definition: An edematous stroma covered by a stratified squamous epithelium
Mean age: 40 years, 25 % are pregnant at the time of diagnosis
Location: Lateral wall of the lower third of the vagina
Size: 0.5–4 cm
Aspect: A polyp or a cerebriform mass
The most common symptoms are postcoital vaginal spotting or bleeding or a vaginal lump. They most typically present as mobile, rounded submucosal, or polypoid masses.
The distinction from sarcoma is made primarily on the basis of superficial location and small size.
30.2.4 Leiomyoma
The most common mesenchymal neoplasm in the vagina
Location: Anywhere usually submucosal
Size: Most are small
Vaginal leiomyoma usually arises in the midline anterior vaginal wall. But it can be located anywhere within the submucosa of the vaginal wall. Their size ranges from 0.5 to 15 cm. Clinical symptoms include vaginal discomfort, vaginal bleeding, and dyspareunia.
On ultrasound the mass is round or oval, of an echogenicity close to that of myometrium, with characteristic acoustic shadowing (Fig. 30.7).
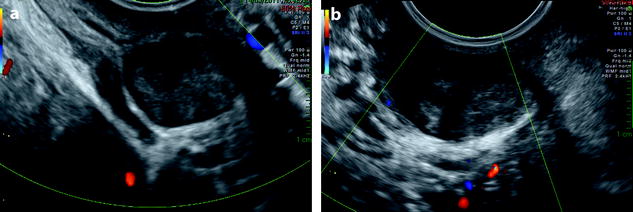
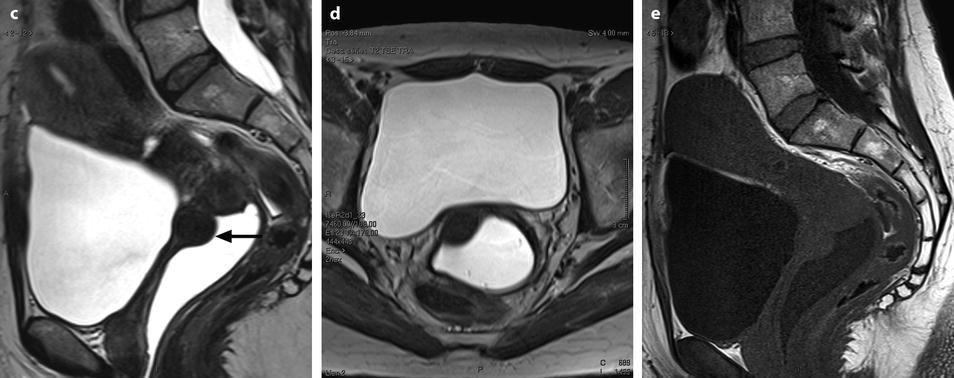
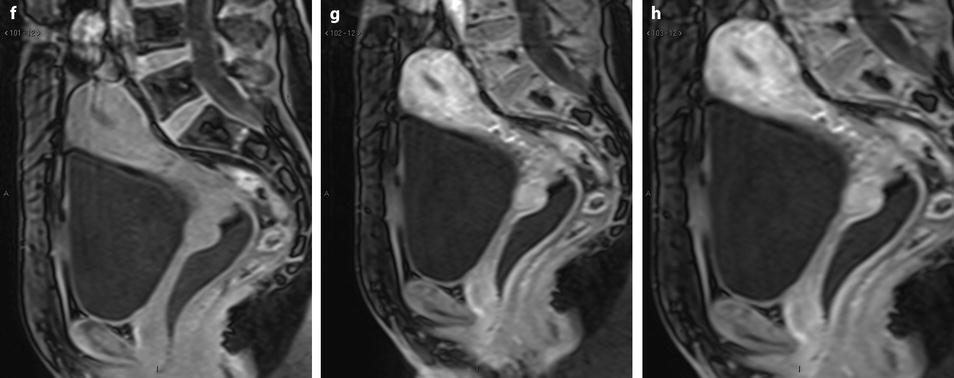
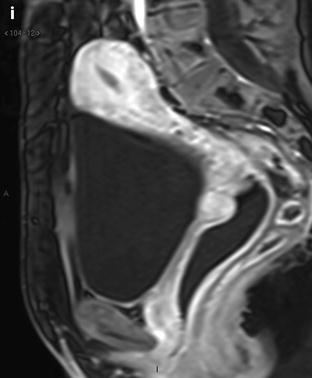
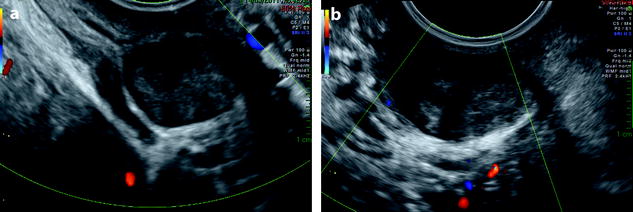
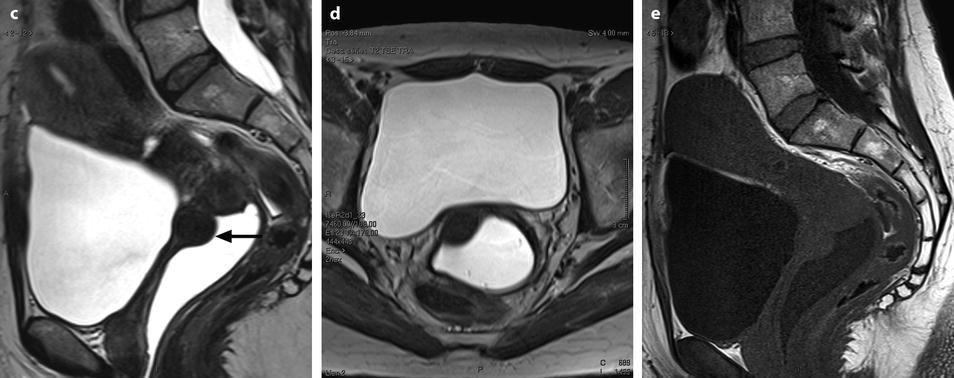
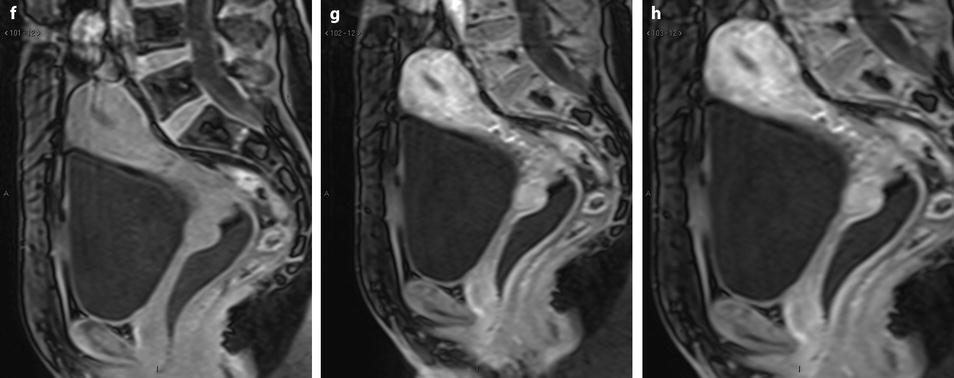
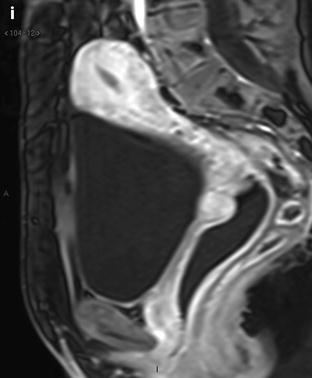
Fig. 30.7
Leiomyoma of the vagina. US Sagittal (a) and axial (b) view display in the anterior and right upper third of the wall of the vagina a round echogenic mass with foci of ultrasound attenuation very suggestive of a leiomyoma. A hypoechoic rim surrounds the mass. Color Doppler does not display any vessel in the mass. MR sagittal T2 (c), axial T2 (d), and sagittal T1 (e) after vaginal opacification depict that the mass (arrow in c) arises in the muscular layer of the wall. Signal of the mass is identical to pelvic muscles on T1 and T2. These two findings are very suggestive of a leiomyoma. Sagittal DMR without injection (f), at the arterial phase (g) and at the venous phase (h) demonstrates regular arterial vessels at the periphery of the mass Fig. 30.7 (continued) On the delayed phase (i), the contrast uptake is identical to myometrium. These features reinforce the diagnosis of leiomyoma that was confirmed at pathology
On MR, they appear as homogeneous low signal intensity on T1 and T2, similar to myometrium. On DMR, on the arterial phase, peripheral arterial vessels are visualized. At the venous phase, there is high and homogeneous contrast uptake identical to myometrium (Fig. 30.7).
While the location to the vagina is clearly established in most cases, in case of low and anterior location, differentiation from urethral leiomyoma may be difficult (Fig. 30.8).
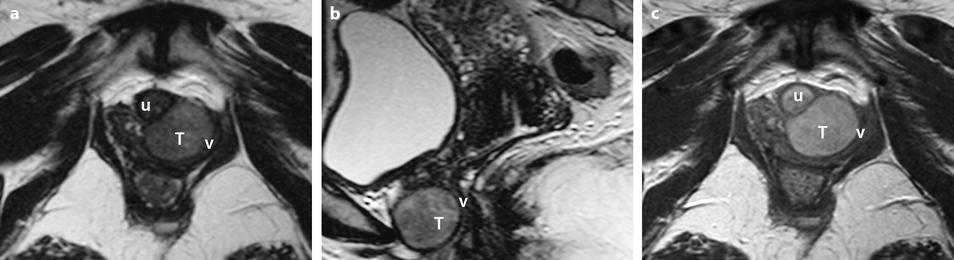
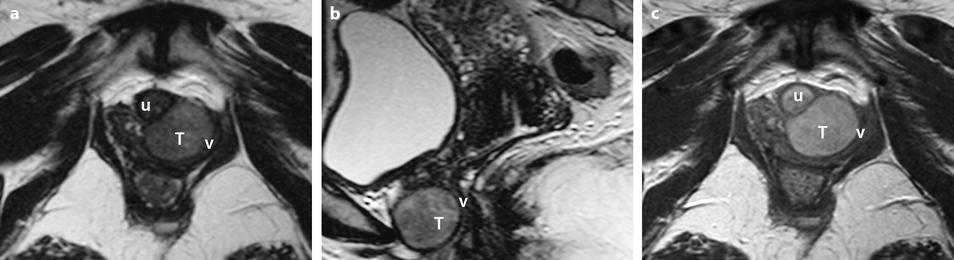
Fig. 30.8
Urethral leiomyoma. Dysuria, dyspareunia, and anterior vaginal wall mass at clinical examination. Axial (a) and sagittal (b) T2W images display a well-defined mass (letter T) of intermediate signal, lying between the urethra and the anterior vaginal wall. The urethral or vaginal origin is impossible to define. On axial T1W image after gadolinium injection (c) the mass enhances homogeneously. Urethra u, Vagina v. The diagnosis of leiomyoma is suggested. Surgery: Leiomyoma of the urethra
30.2.5 Benign Mixed Tumors
Benign mixed tumors histologically bear some resemblance to salivary gland neoplasm. These tumors occur anywhere in the vagina, but most frequently near the hymenal ring. The mean age at diagnosis is 30 years. They range in size from 1.5 to 5 cm. Microscopically, the neoplasm is characterized by a proliferation of stromal and epithelial cells.
Clinically, they are finger-like protruded polypoid structures, well circumscribed, not encapsulated within the mucosa, and unconnected to the surface of epithelium.
30.3 Malignant Neoplasms
30.3.1 Epidemiology
Primary or secondary malignancies can involve the vaginal walls.
Primary vaginal cancer is relatively rare, accounting for 1–3 % of gynecologic malignant tumors and only approximately 0.1–0.2 % of all cancers [1]. To be considered as primary tumor of the vagina, the neoplasm must be located in the vagina without clinical or histological evidence of involvement of the cervix or vulva.
Bulky tumors located in the upper vagina that have extended on to the portio vaginalis of the cervix are considered as primary cervical carcinoma.
It is predominantly a tumor of elderly women (60–65 years).
Secondary vaginal cancer may represent an extension from a cervical cancer or metastatic disease from a uterine, ovarian, vulvar, bladder, or colon primary tumor.
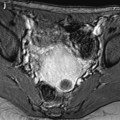
Squamous cell carcinoma occurring in the vagina within 5 years of therapy for cervical carcinoma is considered to be recurrent cervical carcinoma rather than a new primary carcinoma of the vagina (Fig. 30.9).
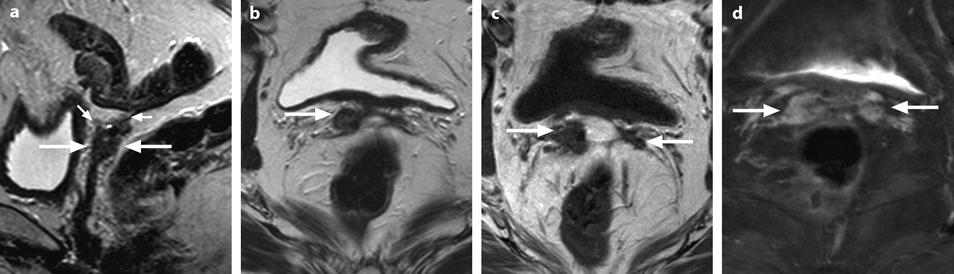
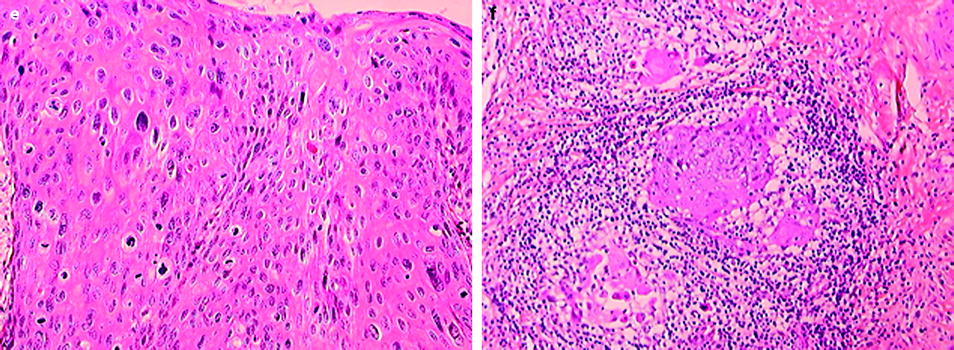
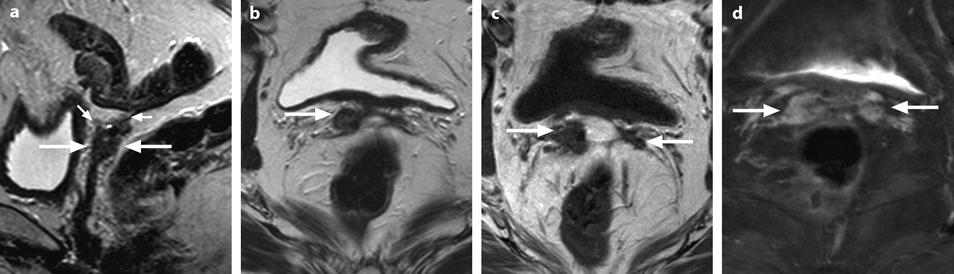
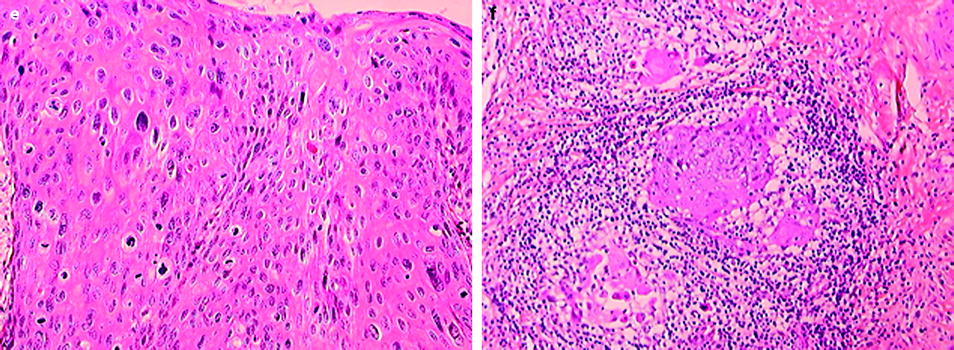
Fig. 30.9
Vaginal squamous cell carcinoma (stage II) after hysterectomy for cervical cancer. A 51-year-old woman with previous hysterectomy for cervical cancer 4 years ago. (a–d) Sagittal (a) and axial (b) T2W images, axial T1W image (c), and axial T1W-FS image after gadolinium injection (d) show a tumor of the upper vagina and vaginal vault (arrows) with subperitoneal nodules (small arrows in a). Fig. 30.9 (continued) (e, f) Microscopic view of the surgical specimen
30.3.2 The Risk Factors
HPV infections (human papillomavirus)
Exposure to diethylstilbestrol (DES) as a fetus (involve young women)
History of cervical cancer
History of cervical precancerous conditions
Vaginal irritation, vaginal adenosis
Uterine prolapse
Smoking
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree