Use: may be used to empty gallbladder about 30 minutes (to 4 hours) before tracer injection in patients on prolonged fasting (gallbladder atony + retained bile and sludge) ← absence of endogenously produced CCK
Dose for hepatobiliary scintigraphy:
package insert: with slow IV injection of 0.01 µg/kg KINEVAC® over 3 minutes (concentration of 1 µg/mL) the response is too variable
preferred: IV infusion of 0.01 µg/kg KINEVAC® over 30–60 minutes
| Useful in: | (a) patient fasting > 24 hours / on total parenteral nutrition |
(b) acalculous cholecystitis | |
(c) chronic GB dysfunction | |
(d) GB ejection fraction |
Side effect: increase in biliary-to-bowel transit time, dizziness, flushing, nausea, abdominal cramps, urge to defecate
Contraindications:
acute pancreatitis, acute cholecystitis, obstruction of cystic duct / CBD, appendicitis, peritonitis, pyloric stenosis, peptic ulcer
Gastrin
= 17 amino acid peptide amide
PENTAGASTRIN = acyl derivative of the biologic active C-terminal tetrapeptide amide
Produced in: antral cells + G cells of pancreas
Released by:
(a) vagal stimulation, gastric distension
(b) short-chain alcohol: ethanol, propanol
(c) amino acids: glycine, β-alanine
(d) caffeine
(e) hypercalcemia
mediated by neuroendocrine cholinergic reflexes
Inhibited by: drop in pH of antral mucosa to < 3.5
Effects:
@ Stomach:
(1) stimulation of gastric HCl secretion from parietal cells, which in turn
(2) increases pepsinogen production by chief cells through local reflex
(3) increase in antral motility
(4) trophic effect on gastric mucosa → parietal cell hyperplasia
@ Pancreas
(1) strong increase in enzyme output
(2) weakly stimulates fluid + bicarbonate output
(3) stimulates insulin release
@ Liver
(1) water + bicarbonate secretion
@ Intestine
(1) stimulates secretion of Brunner glands
(2) increases motility
@ Gallbladder
(1) stimulates contraction
@ Esophagus
(1) increases resting pressure of LES
Glucagon
Produced in: α cells (and β cells) of pancreas
Released by: low blood glucose levels
@ Intestines
(1) lowers pressure of GE sphincter
(2) hypotonic effect on duodenum > jejunum > stomach > colon
@ Hormones
(1) releases catecholamines from adrenal gland → paralysation of intestinal smooth muscle
(2) increases serum insulin + glucose levels → mobilization of hepatic glycogen
@ Biliary tract
(1) increases bile flow
(2) relaxes gallbladder + sphincter of Oddi
Dose for radiologic imaging: 1 mg maximum
◊ IV administration causes a quick response + rapid dissipation of action!
◊ IM administration prolongs onset + increases length of action!
Half-life: 3–6 min
Side effects: nausea + vomiting, weakness, dizziness (delayed onset of 1.5–4.0 hours after IM administration)
Contraindication:
(1) hypersensitivity / allergy to glucagon: urticaria, periorbital edema, respiratory distress, hypotension, coronary artery spasm (?), circulatory arrest
(2) known hypertensive response to glucagon
(3) pheochromocytoma: glucagon stimulates release of catecholamines
(4) insulinoma: insulin-releasing effect may result in hypoglycemia
(5) glucagonoma
(6) poorly controlled diabetes mellitus
Secretin
= 27–amino acid polypeptide hormone
Produced in: duodenal mucosa
Released by: hydrogen ions providing a pH < 4.5 (usually increase in postprandial intraluminal acidity)
The physiologic effects of secretin include secretion of bicarbonate-rich fluid from pancreatic ductal cells and transient increase in the sphincter of Oddi tone, which improves depiction of the pancreatic duct.
Effects:
@ Stomach
(1) inhibits release of gastrin → ↓ in HCl secretion
(2) stimulates pepsinogen secretion by chief cells (potent pepsigogue)
(3) decreases gastric and duodenal motility + contraction of pyloric sphincter
@ Pancreas
(1) increases alkaline bicarbonate-rich pancreatic secretions (NaHCO3 = sodium bicarbonate)
» bicarbonate = 2 x as much carbonate (CO3) per sodium ion in sodium bicarbonate (NaHCO3) as in sodium carbonate (Na2CO3); crucial role in physiological pH buffering
(2) weakly stimulates enzyme secretion
(3) stimulates insulin release
@ Liver
(1) stimulates water + HCO3- secretion (most potent choleretic)
@ Intestine
(1) stimulates secretion of Brunner glands
(2) inhibits motility
@ Esophagus
(1) opens LES
@ Sphincter of Oddi
(1) transient increase in muscle tone used in SOM (sphincter of Oddi manometry)
Secretin Stimulation Test SST
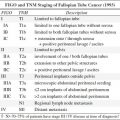
| Indication: | (1) Exocrine pancreas dysfunction |
(2) Gastrinoma versus peptic ulcer disease | |
(3) Identification of ampulla of Vater + accessory papilla during ERCP |
Drug: purified synthetic human secretin ChiRhoStim®, ChiRhoClin®
Dose: 0.2–0.4 µg/kg IV (~ 16 µg for adult) over 1 minute to avoid side effect of abdominal pain
Initial test dose: for possible allergic reaction
Peak effect: usually at 3–5 minutes after injection
√ ↑ main pancreatic duct (MPD) diameter by > 1 mm
√ ↑ visibility of side branches of MPD
√ ↑ T2 SI in duodenum ← excretion of pancreatic fluid
Adverse effects: (in 0.5%) nausea, flushing, abdominal pain, vomiting, mild acute pancreatitis
Dx of gastrinoma:
release of gastrin from gastrinoma cells is increased → increased serum gastrin level of 200 ng/L above baseline (90% sensitive + specific)
N.B.: normally secretin inhibits release of gastrin
Dx of chronic pancreatitis:
aspiration of intestinal secretions via tube passed into duodenum for 1 hour analyzing volume, pH, bicarbonate concentration in 15-minute aliquots (75% sensitive + 90% specific for chronic pancreatitis)
Contraindication: acute pancreatitis
Somatostatin SS
= growth hormone–inhibiting hormone (GHIH); somatotropin release-inhibiting factor (SRIF); somatotropin release-inhibiting hormone (SRIH)
Produced in: many tissues; principally in nervous + digestive systems
Action: inhibits secretion of several other hormones like growth hormone (GH), thyroid stimulating hormone (TSH), cholecystokinin, insulin
Released by: raised levels of other hormones (feed back); ↑ blood glucose + amino acids (food intake)
Inhibited by: reduced levels of other hormones (feed back)
Effects:
@ Hypothalamus
inhibits pituitary gland → ↓ secretion of GH + TSH
Rx: treatment of acromegaly
@ Pancreas
food intake → ↓ secretion of insulin + glucagon
@ GI tract
(a) local reduction of gastric secretion
(b) gastrointestinal motility
(c) inhibits secretion of gastrin + secretin
EMBRYOLOGY OF ALIMENTARY TRACT
Origin: pouchlike extension of the yolk sac
| Division: | (1)foregut supplied by celiac artery for bronchopulmo-nary system, stomach, pancreas, proximal duodenum |
(2)midgut supplied by superior mesenteric artery (SMA) representing axis of gut rotation: mid-duodenum, jejunum, ileum, appendix, ascending colon, mid-transverse colon | |
(3)hindgut supplied by inferior mesenteric artery: mid-transverse colon, rectum |
at 4 weeks: short straight featureless tube
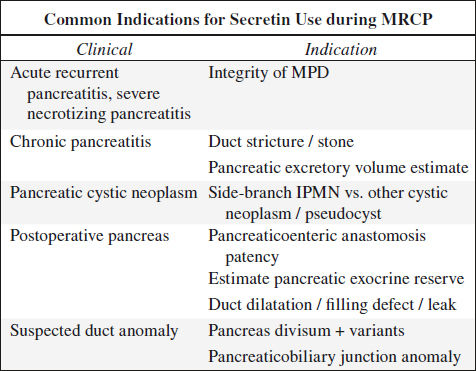
1st rotation:
(a) duodenum rotates cephalocaudal 90° counterclockwise to a position at right of SMA
(b) colon rotates 90° to left of SMA
at 6 weeks: rapid growth of intraabdominal organs (expansion of liver + GI tract) → bowel herniates into umbilical cord = physiologic umbilical herniation
2nd rotation:
(a) duodenum rotates another 90° (completes 180°) counter-clockwise beneath SMA to a position at left of SMA
(b) colon does not rotate
at 10 weeks: bowel returns to abdominal cavity
3rd rotation:
(a) duodenum rotates another 90° (completes 270°) counter-clockwise with duodenojejunal junction resting to left of spine
(b) colon rotates 180° counterclockwise until cecum is located in RLQ by 12th week
Peritoneal fixation of bowel:
› broad-based mesentery extending from ligament of Treitz to ileocecal valve
› colon fuses with retroperitoneum in RLQ with the exception of the most caudal part
› duodenum fixes to retroperitoneum in LUQ
Change in fetal nutrition from yolk sac to placenta:
› during 5th to 7th weeks → regressing omphalomesenteric duct
ARTERIAL SUPPLY OF BOWEL
◊ Bowel receives 20% of resting cardiac output (²/³ for intestinal mucosa) which increases up to 35% in postprandial phase
Influence of food:
carbohydrates → earliest + fast rise
fat + proteins → slower + large rise
Celiac Trunk
Location: at ~ T12 = superior border of pancreatic body
Supplies: from distal esophagus to descending duodenum
Branches: common hepatic a. (CHA), left gastric a. (LGA), splenic artery (SpA) with considerable variations in branching pattern
› CHA branching from SMA (hepatomesenteric type)
› direct branching of CHA / LGA / SpA from aorta
› replaced left hepatic artery
› replaced right hepatic artery
Anastomosis: to SMA via gastroduodenal artery as the 1st branch off the celiac trunk
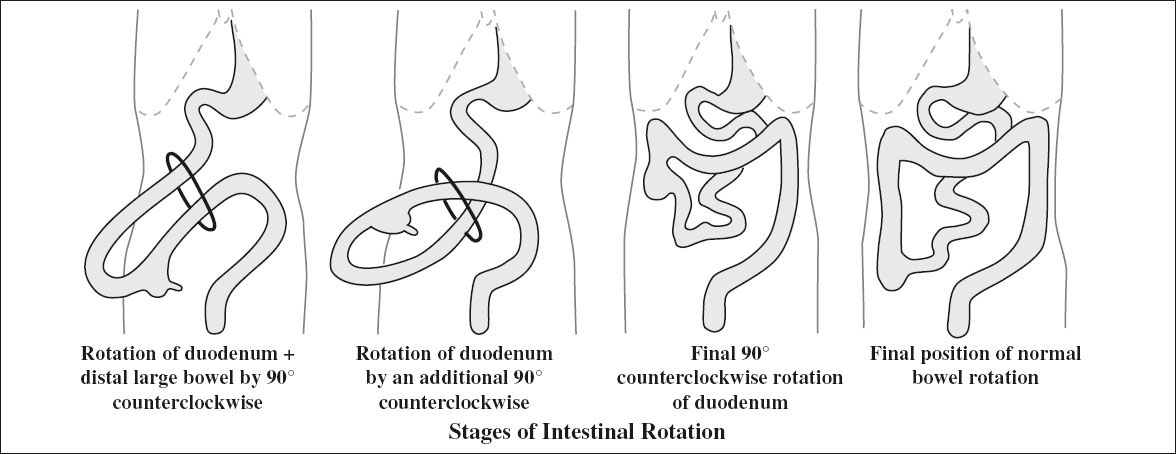
Superior Mesenteric Artery (SMA)
Supplies: transverse + descending duodenum, jejunum, ileum, large bowel to splenic flexure
Anastomosis: with IMA via marginal artery of Drummond, arcade of Riolan
Inferior Mesenteric Artery (IMA)
Supply for: colon from splenic flexure to rectum
Anastomoses: with lumbar branches of abdominal aorta, sacral artery, internal iliac arteries
Arterial Arcades
up to 4 arcades are formed by these arteries which continue toward the periphery as
1. Primary parallel circuits for
a. muscularis propria
b. submucosa
c. mucosa
2. Serial circuits of
a. resistance arterioles
b. precapillary sphincters
c. capillaries
d. postcapillary sphincters
e. venous capacitance vessels
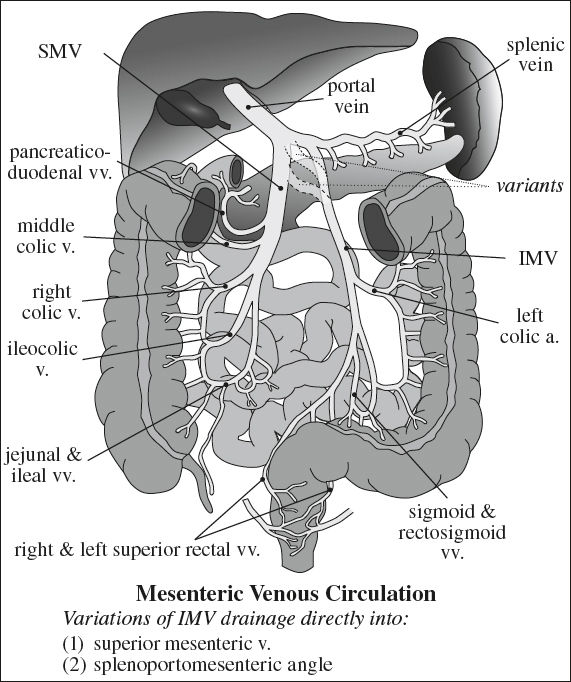
MESENTERIC VENOUS SYSTEM
Venae Rectae
= multiple small veins along bowel wall that join to form venous arcades
Superior Mesenteric Vein
Drainage for: small bowel, proximal colon to splenic angle
Formed by: jejunoileal, ileocolic, right colic, middle colic, pancreaticoduodenal veins
Inferior Mesenteric Vein
Drainage for: splenic flexure, descending colon, sigmoid colon, part of rectum
Formed by: left colic, sigmoid, rectosigmoid, right and left superior rectal veins
Connects to: SMV directly / splenic vein / angle of splenoportomesenteric confluence
ESOPHAGUS
Esophageal Division
1. Upper third
cricopharyngeus to superior margin of aortic arch
2. Middle third
superior margin of aortic arch to inferior pulmonary vein
3. Lower third
inferior pulmonary vein to gastroesophageal junction
Cricopharyngeus Muscle
= main component of upper esophageal sphincter
√ normally closed between swallows
√ relaxes and opens completely for bolus passage to occur in conjunction with elevation of larynx and pharyngeal constrictors
√ prominent posterior indentation on barium column ← incidental / sign of dysphagia
May be associated with:
pharyngeal constrictor muscle weakness, failure of laryngeal elevation, Zenker diverticulum, response esophageal spasm or GERD
Lower Esophageal Anatomy
A. Esophageal Vestibule
= saccular termination of lower esophagus with upper boundary at tubulovestibular junction + lower boundary at esophagogastric junction
√ collapsed during resting state
√ assumes bulbous configuration with swallowing
(a) tubulovestibular junction = A level = junction between tubular and saccular esophagus
(b) phrenic ampulla = bell-shaped part above diaphragm (term should be discarded because of dynamic changes of configuration)
(c) submerged segment = infrahiatal part of esophagus
√ widening / disappearance is indicative of gastroesophageal reflux disease (GERD)
B. Gastroesophageal Junction
Function: regulates flow of food + fluid between esophagus and stomach; key defense against gastroesophageal reflux
| Barrier: | (1) Intrinsic smooth muscle of LES |
(2) Extrinsic striated muscle of crural diaphragm | |
(3) clasp + sling fibers of gastric cardia |
Site: at upper level of gastric sling fibers, straddles cardiac incisura demarcating the left lateral margin of GE junction
C. Z-line = B level = zigzag-shaped squamocolumnar junction line
◊ Not acceptable criterion for locating GE junction
Site: 1–2 cm above gastric sling fibers
D. Lower Esophageal Sphincter
= physiologic 2–4-cm high pressure zone corresponding to esophageal vestibule
√ tightly closed during resting state
√ assumes bulbous configuration with swallowing
Muscular Rings of Esophagus
A Ring
= contracted / hypertrophied muscles in response to incompetent GE sphincter
• rarely symptomatic / dysphagia
Location: at tubulovestibular junction = superior aspect of vestibule
√ usually 2 cm proximal to GE junction at upper end of vestibule
√ varies in caliber during the same examination, may disappear on maximum distension
√ broad smooth narrowing with thick rounded margins
√ visible only if tubular esophagus above + vestibule below are distended
B Ring
= sling fibers representing a U-shaped thickening of inner muscle layers with open arm of U toward lesser curvature = inferior aspect of vestibule
Location: < 2 cm from hiatal margins
√ only visible when esophagogastric junction is above hiatus
√ thin ledge-like ring just below the mucosal junction (Z-line)
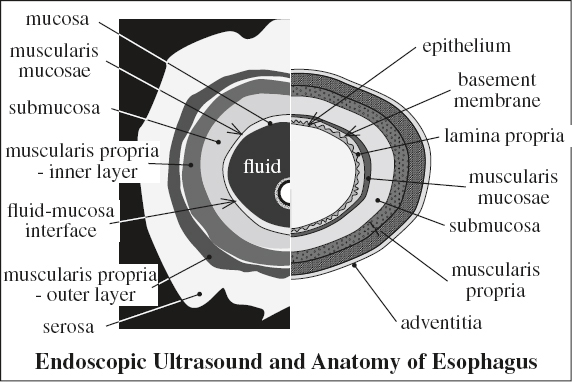
Layers of Intestinal Wall by Ultrasound
= gut signature
1. Mucosa echogenic
√ hyperechoic interface of balloon + mucosa
2. Muscularis mucosae hypoechoic
√ hypoechoic mucosa + muscularis mucosa
3. Submucosa echogenic / hyperechoic
4. Muscularis propria hypoechoic
5. Serosa echogenic / hyperechoic
Most benign conditions preserve the gut signature involving long segments of bowel, while malignant conditions destroy the gut signature involving short segments of bowel.
Aggressive inflammatory processes cause focal disruption of the gut signature.
SWALLOWING FUNCTION
Preparation: refrain from smoking for 12 hours + from eating for > 4 hours before examination
Provide info on baseline anatomy + swallow physiology: for oral cavity, pharynx, larynx, upper esophagus during deglutition
Technique:
Videofluoroscopic Swallow Study (VFSS) = modified barium swallow study to assess handling of bolus; usually performed together with swallowing / speech pathologist
» patient seated upright in lateral + AP positions
» incremental increase in radiopaque bolus volume + texture of various consistencies like nectar liquid, honey liquid, pureed food, soft solid food, hard solid food (commercially available: E-Z Paque liquid, Varibar® thin liquid, nectar, honey, pudding, graham cracker cookie with pudding)
Document patient behavior + reaction:
episode of refusal, cough, silent aspiration, apnea, bradycardia
CNS involved: cranial nerves V, VII, IX, X, XII; 5 cervical nerves; cortical + subcortical pathways; midbrain; brainstem
Muscles involved: 32 groups of muscles
Developmental: swallowing as early as 11 weeks GA;
suckling at 18–24 weeks GA; nonnutritive
sucking at 27–28 weeks GA; single breath
sucking at 35–36 weeks GA
Phases:
1. Oral preparatory phase
√ food chewed + mixed with saliva
2. Oral phase
√ bolus propelled posteriorly to tongue
Path:
(a) spillage from mouth
(b) small bolus formation
(c) tongue tremor
(d) incomplete tongue elevation
(e) early spillage into valleculae prior to initiation of swallow
3. Pharyngeal phase
√ elevation of soft palate + valleculae (to seal nasopharynx)
√ elevation of larynx (to close vestibule)
√ relaxation of cricopharyngeal muscle
√ contraction of lateral pharyngeal wall
At videofluoroscopy carefully evaluate mechanisms to prevent aspiration: superior + anterior elevation of larynx, closure of larynx, and epiglottic tilt.
Path:
(a) nasopharyngeal reflux
(b) laryngeal penetration = contrast material enters laryngeal vestibule
Cause: delayed elevation of larynx
(c) tracheal aspiration = contrast material enters airway below vocal cord level into proximal trachea
Cause: delayed elevation of larynx, delayed pharyngeal transit time, decreased clearance of bolus with residual in vallecula and pyriform sinus spilling into larynx + trachea
4. Esophageal phase
√ contraction of cricopharyngeal muscle
√ bolus transfer into esophagus
Path: cricopharyngeal achalasia (with reflux of bolus into oropharynx / pooling in pyriform sinus)
STOMACH
Segmental Anatomy of Stomach
1. Cardia
2. Fundus
Dependency: most superior portion when upright most dependent portion when supine
√ stomach bubble on CXR
√ accumulation of intraluminal contents on CT
3. Body
(a) lesser curvature: left and posteriorly on CT
(b) greater curvature: right and anteriorly on CT
√ ≤ 5 mm in thickness (in distended state)
» Incisura angularis
= transition to antral-type mucosa
◊ Most common site for gastric ulcers!
4. Antrum
= thickest gastric segment ← most muscular
√ ≤ 12 mm in thickness (in distended state)
√ exhibits the most peristalsis
√ may display mural stratification on CECT
5. Pylorus
Inadequate gastric distention limits diagnostic evaluation and may create a false appearance of thickening or may obscure true disease.
When evaluating abnormal gastric wall thickening in a nondistended stomach, supplementary findings can be helpful in identifying disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree