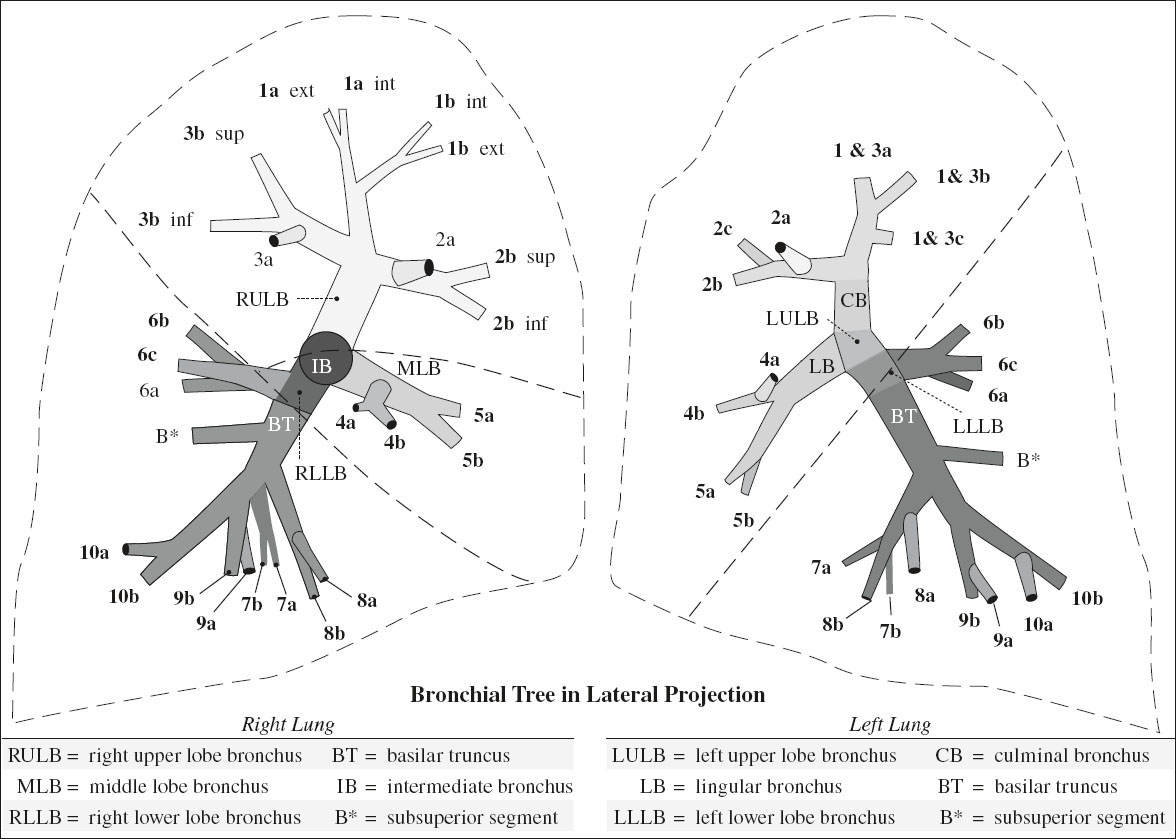
ORDER OF BRONCHOPULMONARY SEGMENTS OF RIGHT LUNG:
AIRWAYS
The carina is normally at the level of T4/T5.
Embryology of Airways & Maldevelopment
| first 5 weeks GA | lung buds grow from ventral aspect of primitive foregut (from caudal end of laryngotracheal groove of primitive pharyngeal floor) |
| abnormal: | pulmonary agenesis |
| 5th week GA | separation of trachea + esophagus |
| 5–16 weeks | formation of tracheobronchial tree with bronchi, bronchioles, alveolar ducts, alveoli |
| abnormal: | bronchogenic cyst ← abnormal budding; |
| pulmonary hypoplasia ← fewer than expected bronchi | |
| 16–24 weeks | dramatic increase in number + complexity of airspaces and blood vessels |
| abnormal: | small airways ← reduction in number and size of acini |
Anomalous Bronchial Division
Branching anomalies:
(a) displaced (replaced) bronchus
√ bronchus with abnormal origin while normal bronchus ventilating corresponding parenchyma is absent
(b) supernumerary (accessory) bronchus
√ may end blindly in parenchyma of corresponding normal bronchus = congenital bronchial diverticulum
√ may ventilate additional lung parenchyma, possibly delineated by an accessory fissure
Tracheal Bronchus (0.1–2.0%)
= bronchus of variable length arising from lower trachea
Frequency: 0.1–1.3% in adults; 1.5–2% in childhood
In 78% associated with:
Down syndrome; malformation of thoracic cage / foregut / lung; tracheal stenosis; other tracheobronchial branching anomalies
Type: displaced in 75%; supernumerary in 25% → ventilating intra- / extralobar tracheal lobe (NOT related to azygos lobe)
Location: almost invariably on right; bilateral (rare)
Site: distal trachea < 2 cm from carina
• recurrent pneumonia, respiratory distress in childhood
• almost invariably asymptomatic in adults
√ blind-ending pouch (= congenital right tracheal diverticulum) / aeration of a portion or all of RUL
√ early origin of apicoposterior LUL bronchus (less common)
√ “pig bronchus” = entire RULB displaced on trachea
Right Preeparterial Bronchus
= any bronchus directed toward RUL that arises abnormally from RMB above level of right eparterial ULB
Frequency: 0.9%
Type: 82% displaced
• mostly asymptomatic
DDx: accessory cardiac bronchus
Right Posteparterial Bronchus
= any bronchus directed toward RUL that arises abnormally from right bronchial tree below level of right eparterial ULB
Left Eparterial Bronchus
= any bronchus directed toward LUL that arises from posterolateral / lateral wall of LMB above level where left pulmonary artery crosses LMB
Left Prehyparterial Bronchus
= anomalous bronchus directed toward LUL that arises from LMB between level of left pulmonary artery crossing and hyparterial LULB
Accessory Cardiac Bronchus (ACB)
= true supernumerary anomalous bronchus
The only bronchus originating from medial wall of either RMB or IMB (occasionally on left side)
M÷F = 2.8÷1
√ arises from medial wall of bronchus intermedius prior to origin of apical segmental RLL bronchus
√ caudal course toward pericardium
√ blind-ending pouch / ventilation of an accessory lobe
Bridging bronchus
= aberrant bronchus that partially / totally supplies the right lung but originates from LMB
√ carina at T4–T5
√ pseudocarina in the shape of an inverted T at T6-T7
Paracardiac Bronchus
= normal bronchus arising from medial aspect of lower lobe
Prevalence: 5% of patients
Airway
= conducting branches for the transport of air; ~ 300,000 branching airways from trachea to bronchiole with an average of 23 airway generations
Definition:
bronchus = cartilage in wall
bronchiole = absence of cartilage (after 6–2 divisions of segmental bronchus)
› membranous bronchiole = purely air conducting
› respiratory bronchiole = contains alveoli in its wall
› lobular bronchiole = supplies secondary pulmonary lobule; may branch into 3 or more terminal bronchioles
› terminal bronchiole = last generation of purely conducting bronchioles without alveoli; each supplying one acinus
| small airways | = | internal diameter < 2 mm = small noncartilaginous membranous and respiratory bronchioles; account for 25% of airway resistance |
| large airways | = | diameter > 2 mm; account for 75% of airway resistance |
HRCT of normal lung (window level –700 HU, window width 1,000–1,500):
√ –875 ± 18 HU at inspiration
√ –620 ± 43 HU at expiration
√ 8th order bronchi visible = bronchi > 2 mm in diameter
◊ Normal lobular bronchioles NOT visible!
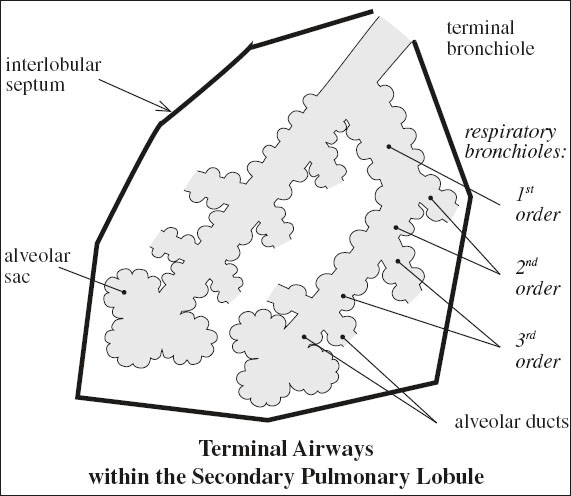
Acinus
◊ Functionally most important subunit of lung!
= all parenchymal tissue distal to one terminal bronchiole comprising 2–5 generations of respiratory bronchioles + alveolar ducts + alveolar sacs + alveoli
• gas exchange
√ radiologically NOT visible
Cells of Lung Parenchyma 75% of all lung cells
1. Air-blood barrier
› epithelial cells (25%) = lining of air space
› endothelial cells (25%) = lining of vessels
› interstitial cells (35%), collagen fibres (15%)
2. Alveolar epithelium
› lining cells (type I pneumocyte) → tight junctions, no mitosis
› secretory cells (type II pneumocyte) → synthesis + storage + secretion of surfactant
› brush cells
[Primary Pulmonary Lobule]
= alveolar duct + its connected air spaces
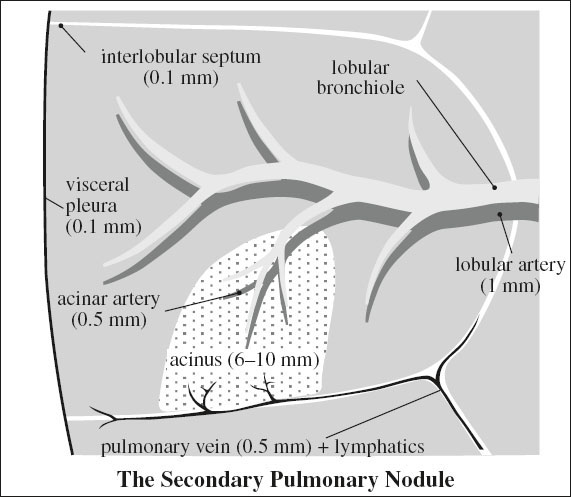
Secondary Pulmonary Lobule
= REID LOBULE
[Lynne McArthur Reid (1923–?), experimental pathologist and dean of Cardiothoracic Institute, London University, Harvard Medical School, pathologist-in-chief emeritus at Children’s Hospital in Boston]
= smallest portion of lung surrounded by connective tissue septa; supplied by 3–5 terminal bronchioles
√ basic anatomic + functional pulmonary unit appearing as an irregular polyhedron containing 3–24 acini
√ separated from each other by thin fibrous interlobular septa (100 µm)
Size: 10–25 mm in diameter
• visible on surface of lung
Contents:
› centrally = lobular core:
» branches of terminal bronchioles with a 0.1 mm wall thickness = below the resolution of HRCT
√pulmonary arterioles (1 mm)
› peripherally (within interlobular septa):
√pulmonary vein + lymph vessels
HRCT:
√ barely visible fine lines of increased attenuation in contact with pleura (= interlobular septa); best developed in subpleural areas of
| › | UL + ML: | anterior + lateral + juxtamediastinal |
| › | LL: | anterior + diaphragmatic regions |
√ dotlike / linear / branching structures (= pulmonary arterioles)
Site: near center of secondary pulmonary lobule; 3–5 mm from pleura
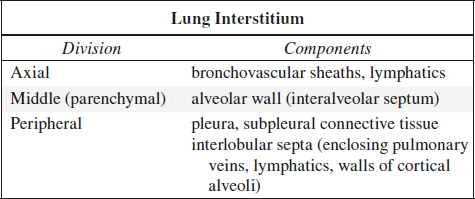
Interstitial Anatomy
1. Bronchovascular interstitium
surrounding bronchovascular bundle
2. Centrilobular interstitium
surrounds distal bronchiolovascular bundle
√ line extending to the center of a lobule
3. Interlobular septal interstitium
√ lines perpendicular to pleura surrounding a lobule
4. Pleural interstitium
Lung Development
› embryonic phase
respiratory diverticulum (= laryngotracheal bud) originates from ventral wall of primitive foregut
→ elongation of lung bud → lateral invagination of mesoderm → tracheoesophageal septum
→ bifurcation of laryngotracheal bud at 5–7 weeks EGA → R + L mainstem bronchi
→ mainstem bronchi branch further into lobar bronchi
→ pulmonary arteries arise from 6th aortic arch
Time: 26 days to 7 weeks EGA
› pseudoglandular phase development of segmental + subsegmental bronchi, respiratory bronchioles + terminal bronchioles, alveolar ducts + alveoli
Time: 7–16 weeks EGA
› canalicular / acinar phase development of distal acinar units + canalization of further airspaces; airspaces are approximated by network of capillaries; type II alveolar cells capable of surfactant synthesis
Time: 16–24 weeks EGA
› saccular phase increase in number of terminal sacs + thinning of intervening interstitium + beginning of alveolar septation
Time: 24–36 weeks EGA
› alveolar phase development of true fully mature alveoli with progressive formation throughout first 2 years of life
Time: 36 weeks EGA – 18th postnatal month
mnemonic: Every Premature Child Takes Air
Embryonic phase
Pseudoglandular phase
Canalicular phase
Terminal sac phase
Alveolar phase
Surfactant
= surface-active material essential for normal pulmonary function
Substrate: phospholipids (dipalmitoylphosphatidylcholine, phosphatidylglycerol), other lipids, cholesterol, lung-specific proteins
Production: type II pulmonary alveoli synthesize + transport + secrete lung surfactant; earliest production around 18th week of gestation (in amniotic fluid by 22nd week of gestation)
Action: increases lung compliance, stabilizes alveoli, enhances alveolar fluid clearance, reverses surface tension, protects against alveolar collapse during respiration, protects epithelial cell surface, reduces opening pressure + precapillary tone
PULMONARY CIRCULATION
Primary Pulmonary Circulation
⇒ supplies 99% of blood flow to lungs pulmonary arteries travel along lobar + segmental bronchi down to subsegmental level matching caliber of airways
(a) large elastic pulmonary arteries (500 to > 1,000 µm) accompany lobar + segmental bronchi matching caliber of airways
› main pulmonary artery / trunk: ≤ 28 mm
› right / left pulmonary artery
› lobar pulmonary artery
› segmental pulmonary artery
(b) muscular arteries (50–1,000 µm) accompany subsegmental airways + terminal bronchioles
√ provide active vasodilatation + constriction
(c) arterioles (15–150 µm) accompany respiratory bronchioles + alveolar ducts
(d) capillary network in alveolar walls
(e) venules
(f) pulmonary veins course through interlobular fibrous septa
Function: gas exchange
Bronchial Circulation
⇒ supplies 1% of blood flow to lungs = 1% of cardiac output
Pressure: systemic high-pressure system (6 x that of normal pulmonary circulation); bronchial arteries are resistant to arteriosclerosis
Origin:
(a) orthotopic bronchial artery (64%): anteriorly from proximal to mid-descending thoracic aorta at level of left main bronchus between superior endplate of T5 and inferior endplate of T6
Angio landmark: 1 cm above / below level of left main bronchus as it crosses descending thoracic aorta
(b) at least one ectopic bronchial artery (36%):
› from undersurface of aortic arch (15%)
› distal descending thoracic aorta, subclavian artery, thyrocervical trunk, costocervical trunk, brachiocephalic trunk, internal mammary artery, pericardiophrenic a., inferior phrenic a., coronary a.
(c) left bronchial artery: most commonly directly from aorta toward left side of esophagus
(d) right bronchial artery: most commonly originating from another artery, typically intercostal artery toward right side of esophagus
Variants of vascular anatomy (9 types):
(1) 1 right bronchial a. arising posteromedially from a common InterCostal Bronchial Artery Trunk (ICBAT) + 2 left bronchial a. anteriorly (41%)
(2) 1 bronchial artery on each side, the right bronchial artery originating from an ICBAT (21%)
(3) 2 bronchial aa. on each side, 1 right bronchial artery originating from an ICBAT (21%)
(4) 1 right bronchial a. + 1 right ICBAT + 2 left bronchial arteries (10%)
Course: behind trachea and main-stem bronchi; enter lung via hila; tortuous path along peribronchial sheath of mainstem airway to terminal bronchioles
Function:
⇒ nourishment for supporting structures
› extra- and intrapulmonary airways
› vasa vasorum of pulmonary arteries
› nerves, pulmonary veins, lymph nodes within thorax
⇒ systemic blood supply to
› trachea, bronchi, bronchial branches, visceral pleura
› esophagus
The bronchial circulation + other collateral vessels (eg, intercostal, internal mammary, inferior phrenic aa.) respond to chronic pulmonary ischemia and ↓ pulmonary blood flow → vessel hypertrophy / enlargement → maintenance of blood flow to affected lung + participation in gas exchange through systemic-pulmonary arterial anastomoses beyond the pulmonary artery obstruction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree