= NO-FLOW / LOW-FLOW VASCULAR MALFORMATION
= LYMPHATICOVENOUS MALFORMATION
Prevalence: 3.5÷100,000; 1–2% of orbital childhood masses; 4–8% of expanding pediatric orbital lesions; 25% of vasculogenic orbital lesions
Origin: arises from a pluripotent venous anlage as a malformation (NOT neoplasm of proliferating cells!)
Path: unencapsulated diffuse multicompartmental lesion often with intra- and extraconal components insinuating between normal orbital structures
Histo: dilated lymphatics, dysplastic venous vessels, smooth muscle, areas of hemorrhage
(a) simple / capillary lymphangioma
= lymphatic channels of normal capillary size
(b) cavernous lymphangioma (most common)
= dilated microscopic channels
(c) cystic hygroma
= macroscopic multilocular cystic mass
May be associated with: intracranial vascular anomalies (70%): developmental venous anomalies (61%), AVM, cerebral cavernous malformation, sinus pericranii
Age: 1st decade or later (mean age of 6 years); M÷F = 1÷1; 43% before age of 6 years; 60% before age of 16 years
• proptosis:
• slowly progressive proptosis with restriction of eye movement, optic nerve compression, vertical displacement of globe
• sudden proptosis from intratumoral hemorrhage
= CARDINAL FEATURE; often occurring spontaneously / after minor trauma / during upper respiratory infection
• worsening proptosis from intralesional proliferation of lymphocytes during viral infection with subsequent resolution
• associated with lesions on lid, conjunctiva, cheek:
• eyelid fullness from birth
• purple discoloration of skin, usually in superomedial orbit
• vesicles in conjunctiva, facial skin, oral mucosa
• restricted ocular motility (50%)
• growth with patient’s growth ± accelerated growth in response to hormonal changes (during puberty / pregnancy)
Location: unilateral; usually medial to optic nerve with intra- and extraconal component, crossing anatomic boundaries (conal fascia / orbital septum)
Site: superficial (conjunctiva + eyelid) in anterior orbit (79%); deeper orbit (67%); pre- and postseptal orbit (73%)
√ poorly defined infiltrating multilobulated heterogeneous lesion
√ single / multiple cystlike areas with rim enhancement (after hemorrhage):
√ solid-appearing microcystic component
√ macrocystic component = cysts of 1–2 cm in size
√ blood cyst = “chocolate cyst” associated with multiple recurrences
√ variably mild patchy low-flow enhancement (= venous channels) / ring enhancement (after hemorrhage)
√ rarely contains phleboliths (DDx: hemangioma, orbital varix)
US:
√ heterogeneous echotexture with ill-defined borders:
√ area of predominantly cystic low-level internal echoes with infiltrative borders
√ hyperechoic intracystic clot
CT:
√ poorly marginated lesion insinuating itself between normal structures:
√ well visualized ← inherent contrast between malformation + orbital fat
√ venous / solid components slightly hyperattenuating relative to brain tissue
√ macrocystic lymphatic components similar in attenuation to vitreous of globe
√ mild to moderate expansion / remodeling / hyperostotic / lytic lesion of bony orbit
√ ± widening of superior / inferior orbital fissure
√ frequent thickening of upper eyelid
MR (modality of choice):
√ iso- to slightly hyperintense relative to brain on T1WI + very hyperintense relative to brain on T2WI:
√ T1WI for lymphatic / proteinaceous fluid
√ fat-suppressed T1WI for blood / blood products
√ fat-suppressed T2WI for nonhemorrhagic fluid
√ fluid-fluid levels of hemorrhages of various ages / T2 shading in multiple cysts (almost PATHOGNOMONIC)
√ NO enlarged feeding vessels / flow voids
Prognosis: no involution; aggressive behavior with continued enlargement (in 64%) + recurrence after treatment; eventually loss of vision (in 40%); progression slows with termination of body growth
Rx: observation; intralesional injection with sclerosing agents (tetradecyl sulfate or OK-432) / steroids; surgery in case of optic nerve compression + for relieve of pain and for cosmetic improvement
DDx: orbital varix (affected by postural changes, communication with systemic circulation)
LYMPHOMA OF ORBIT
Usually presents without evidence of systemic disease; subsequent development of systemic disease frequent
Frequency: in 8% of leukemia; in 3–4% of lymphoma; 67–90% of orbital lymphoproliferative tumors; 24% of all space-occupying orbital tumors in patients > 60 years of age
Age: 50 years on average
Type: usually non-Hodgkin B-cell lymphoma; Burkitt lymphoma with orbit as primary manifestation; Hodgkin disease rare
• palpable mass, mildly restricted ocular motility
• painless swelling of eyelid (pain is uncommon)
• proptosis (late in course of disease)
◊ 3rd most common cause of proptosis (after orbital pseudotumor + cavernous hemangioma)
Location: extraconal (especially lacrimal gland, anterior extraconal space, retrobulbar) > intraconal > optic nerve-sheath complex; unilateral (76%)
◊ The lacrimal gland is a common site for leukemic infiltrates + lymphoma (40%)!
Growth types:
(a) well-defined high-density mass (most commonly about lacrimal gland)
√ smooth circumscribed mass (50%)
(b) diffuse infiltration (tends to involve entire intraconal region)
√ diffuse ill-defined lesion (50%)
√ tendency to mold to orbital structures (globe, optic nerve, orbital wall → ± bone remodeling
√ slight to moderate uniform enhancement
√ isointense relative to muscle on T1WI
√ hyperintense relative to orbital fat on T2WI
US:
√ solitary / multiple hypoechoic homogeneous masses with infiltrative borders
DDx: pseudotumor (infiltration / thickening of ocular muscles, mass commonly T2-isointense relative to orbital fat, high ADC values, acute onset of pain)
MEDULLOEPITHELIOMA
= DIKTYOMA = TERATONEUROMA [diktyon, Greek = net]
= rare embryonal malignant (most) / benign intraocular neoplasm
Origin: primitive medullary epithelium in ciliary body
Histo: folded cords + sheets resembling a fisherman‘s net (diktyomatous pattern) surrounding fluid collections predominantly composed of hyaluronic acid; heteroplastic components of hyaline cartilage, rhabdomyoblasts, neuroglia, sarcomatous elements (a) teratoid (30–50%) (b) nonteratoid (50–70%)
Mean age: 5 years; M=F
• poor vision ← lens subluxation, lens notching, glaucoma, cataract formation, retinal detachment
• pain; leukokoria; mass of iris / ciliary body
• exophthalmos, buphthalmos. strabismus, ptosis
Location: ciliary body (common); optic nerve head / retina (rare); usually unilateral
√ dystrophic calcifications (in hyaline cartilage component) in 30%
US:
√ echogenic irregularly shaped /ovoid mass
CT:
√ dense irregular mass
√ moderate to marked enhancement
MR:
√ slightly to moderately hyperintense to vitreus on T1WI
√ hypointense on T2WI
√ marked homogeneous enhancement / heterogeneous (← cystic components)
Prognosis: local recurrence common; metastases rare
METASTASIS TO ORBIT
Prevalence: 1–13% of orbital tumors
Origin: source known in only in 50%
adults: carcinoma of breast + lung
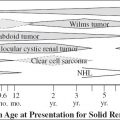
children: neuroblastoma > Ewing sarcoma, leukemia, Wilms tumor
Frequency of metastases to orbit:
breast cancer (48–53% of orbital metastases) > prostate carcinoma > cutaneous melanoma > lung cancer
• proptosis, motility disturbance, pain, diplopia, ↓ vision
• paradoxical enophthalmos (10% of orbital lesions)
= posterior globe retraction ← infiltrative + fibrotic contraction of orbital fat ← scirrhous breast cancer (most common) / scirrhous gastrointestinal carcinoma
Location: 12% intraorbital, 86% intraocular; bilateral in ⅓
Preferential site by type of metastasis:
› breast cancer → orbital fat + muscle
› prostate cancer → bone
› melanoma → muscle
√ diffuse enhancement of retrobulbar fat with abnormally heterogeneous hypointensity on T1WI + T2WI ← fibrotic infiltration
DDx: thyroid ophthalmopathy (bilateral, sparing tendinous insertions); orbital pseudotumor (typically painful involving tendinous insertion); sarcoidosis
Choroidal Metastasis
[choroid = posterior portion of uvea]
◊ Most common ocular malignancy in adults!
Origin: lung > breast, hypervascular + hematologic malignancy
Location: posterior half of globe near macula (access via short posterior ciliary arteries); extension along plane of choroid (in ⅓ bilateral + in ⅓ multiple)
• often asymptomatic (unless fovea involved)
• visual loss ← retinal detachment
√ small areas of broad-based flat thickening + increased density
√ subretinal fluid = retinal detachment
√ mild posterior choroidal thickening
US:
√ often multiple hyperechoic posterior wall masses: usually flat / discoid + with an irregular surface
√ higher flow than melanoma at Doppler
MR:
√ iso- to hyperintense on T1WI, hyperintense on T2WI
√ heterogeneous enhancement
√ may be T1 hyperintense + T2 hypointense ← high level of protein / hemoglobin degradation products ← metastasis from mucin-producing adenocarcinoma / hemorrhagic metastasis
NORRIE DISEASE
= RETINAL DYSPLASIA
= X-linked recessive disease: ? inherited form of persistent hyperplastic primary vitreus
• seizures, mental retardation (50%)
• hearing loss, deafness by age 4 (30%)
• bilateral leukokoria + microphthalmia
• cataract, blindness ← absence of retinal ganglion cells
√ microphthalmia
√ dense vitreus with blood-fluid level
√ cone-shaped central retinal detachment
√ calcifications
OCULAR TRAUMA
Frequency: 3% of all visits to Emergency Department in USA
Cause: blunt trauma (97%)
Mechanism: motor vehicle accident, sport-related accident, industrial accident, fall, violent trauma
Associated with: facial fractures (up to 11%), head injury (84%)
• clinical evaluation: testing of visual acuity, slit-lamp evaluation of cornea + anterior segment, intraocular pressure measurement, funduscopy
US (used if ocular media opaque due to vitreous hemorrhage / hyphema / traumatic cataract):
◊ Dynamic imaging improves visualization of the entire eye and depicts movement of vitreous echoes / lines.
√ may depict hyphema, lens dislocations, globe rupture, intraocular foreign body, vitreous + retinal hemorrhage
Contraindications for ocular US:
suspected traumatic globe rupture / recent surgery to prevent extrusion of ocular contents
CT (modality of choice):
√ especially useful for foreign body
MR:
√ CONTRAINDICATED with metallic foreign bodies
√ usually reserved for subtle open-globe injury / organic foreign body
Anterior Chamber Injury
1. Corneal laceration
Cause: usually penetrating trauma
√ decreased anterior-posterior dimension of anterior chamber compared to a normal globe on CT
Cave: anterior subluxation of lens may mimick a decreased anterior chamber volume
Cx: globe rupture with complete penetration of cornea
2. Traumatic hyphema
Cause: disruption of blood vessels in iris / ciliary body
• blood-fluid level in anterior chamber
√ increased attenuation in anterior chamber on CT
Cave: US NOT RECOMMENDED → excessive pressure
Lens Dislocation
Cause:
(1) Blunt trauma to eye (> 50% of all lens dislocations)
(2) Spontaneous (and often bilateral)
associated with connective tissue: Marfan syndrome, Ehlers-Danlos syndrome, homocystinuria
Pathomechanism: deformation of globe in anteroposterior direction → compensatory expansion equatorially → stretching + tearing of zonular attachments → dislocation of lens
Location of lens: posterior (common) / anterior (unusual)
Types:
(a) partial luxation = one margin of lens maintains its normal position behind iris
√ posteriorly angled position of lens
(b) complete luxation
√ lens in dependent portion of vitreous humor
In trauma associated with: echogenic lens (= traumatic cataract) + vitreous hemorrhage
Traumatic Cataract
Pathophysiology: disruption of lens capsule → edema within lens → cataract
√ hypoattenuating lens compared with nonaffected lens (in acute phase)
√ hyperattenuating / calcified lens (= mature cataract)
Open-Globe Injury = Ruptured Globe
= disruption of scleral integrity by blunt trauma / penetrating injury
Site: behind insertion of intraocular muscles (= thinnest portion of sclera)
• enlarged anterior chamber
US: CONTRAINDICATED in suspected globe rupture
CT (56–75% sensitive):
√ direct signs of globe injury:
√ change in globe contour (DDx: coloboma, staphyloma, posttraumatic orbital hematoma)
√ “flat tire” sign = loss of volume
√ scleral discontinuity with prolapse of vitreus
√ indirect signs of globe injury:
√ deep anterior chamber = mild posterior movement of lens (in spite of intact zonular fibers)
Mechanism: rupture in posterior segment → decrease in pressure + volume → allows lens to sink posteriorly
√ decreased anterior chamber depth = decreased volume in anterior segment ← severe corneal laceration
One indirect imaging finding of open-globe injuries is alteration of the anterior chamber depth.
√ intraocular air (DDx: injected perfluoropropane gas for treatment of retinal detachment)
√ intraocular foreign body (DDx: metal buckle of scleral band for treatment of retinal detachment)
◊ Consider MRI when a clinically suspected open-globe injury is not identified at CT!
Cx: blindness
Nontraumatic mimics:
coloboma, staphyloma, congenital glaucoma, elongated globe from myopia, phthisis bulbi
Altered globe contour:
mass effect from orbital mass / hematoma
Ocular Detachments / Posterior Segment Injury
1. Traumatic retinal detachment
= separation of retina from choroid
Mechanism: traumatic retinal tear → accumulation of vitreous fluid + blood between retina and choroid → detachment of retina
(a) Total retinal detachment
√ characteristic V-shaped appearance with apex at optic disc
√ retina remains bound down at ora serrata
(b) Focal retinal detachment
√ elevated immobile line close to sclera at periphery of globe
Retinal detachments may have a characteristic V-shaped appearance with the apex at the optic disc !
2. Vitreous detachment
= separation of vitreous from retina
√ thin undulated mobile line moving away from posterior aspect of globe during eye motion
3. Traumatic choroidal detachment
= separation of choroid from sclera by fluid accumulation in potential suprachoroidal space
Mechanism: traumatic injury → decreased pressure in posterior segment + suprachoroidal space → accumulation of fluid / blood → detachment of choroidal layer
Site: from vortex vein to ora serrata
√ biconvex / lentiform fluid accumulation
√ lentiform / biconvex shape with sparing of posterior portion of globe
DDx: high-attenuation silicone oil injected between vitreus and retina for treatment of retinal detachment
Choroidal detachments have a lentiform / biconvex shape and spare the posterior portion of the globe !
Intraocular Hemorrhage
1. Vitreous hemorrhage (53%)
Mechanism: disruption of retinal blood vessels → hemorrhage into vitreous humor of posterior segment
• “black rain” / decreased visual acuity (frequent)
US:
√ normal / slightly increased vitreous echogenicity (= mild acute bleeding)
√ poorly defined low-level echoes / hypoechoic clots within vitreous (= abundant hemorrhage)
√ echogenic material moving freely within vitreous chamber during eye movement
CAVE: Severe vitreous hemorrhage may obscure other ocular findings!
CT:
√ hyperattenuating fluid in posterior segment
Cx: retinal detachment ← vitreous traction ← fibrovascular ingrowth following hemorrhage
Prognosis: resolution may occur within 2–8 weeks
Rx: vitrectomy
2. Retrohyaloid hemorrhage (2%)
√ echogenic material remaining behind detached vitreous capsule during eye movement
3. Hematoma in retroocular space
Intraocular Foreign Body
Incidence: penetrating eye injury in 3.1÷100,000 per year
◊ Intraorbital foreign bodies are present in 10–17% of all ocular injuries + in 41% of open-globe injuries!
Cause: violent trauma, motor vehicle accident, recreational accident, work-related industrial accident
Location: anywhere (commonly in posterior segment)
Type: (a) inorganic: metal, glass, plastic
(b) organic: wood → may cause a severe infection
Radiography (40–90% sensitive, depending on type of material)
US (95% sensitive for intraocular + 50% for intraorbital foreign body):
√ echogenic spot
DDx: intraocular air may mimic a foreign body
CT (up to 100% sensitive):
√ metallic fragments < 1 mm can be demonstrated
√ glass foreign body: (detection depends on location, size + type of glass)
√ 96% of > 1.5-mm glass foreign bodies
√ 48% of 0.5-mm glass foreign bodies
√ wood splinter:
√ Wood is initially of low attenuation similar to air
√ geometric margins
√ increase in density after 1–5 days
MR:
N.B.: Failure to detect a metallic foreign body before performing MR may result in blindness!
√ more sensitive than CT in depicting organic material
Cx: siderosis (if metallic), endophthalmitis, retinal toxicity, vision loss
DDx: optic drusen; scleral plaques (calcifications along insertions of medial + lateral rectus mm. in elderly); calcified cataract; material for treatment of retinal detachment (scleral bands, silicon oil, gas)
OPTIC DRUSEN
= accretions of hyaline material on / near surface of optic disc; often familial
Age: patient with macular degeneration; also in young patient
• usually asymptomatic
• headache, visual field defects
• pseudopapilledema
Location: at junction of retina + optic nerve; bilateral in 75%
US:
√ hyperechoic lesions at papilla + acoustic shadowing
CT:
√ hyperattenuating small flat / round calcification
Cx: atrophy of optic nerve
OPTIC PATHWAY GLIOMA
= JUVENILE PILOCYTIC ASTROCYTOMA = OPTIC NERVE GLIOMA
= isolated to single prechiasmatic optic nerve anywhere along optic tract ± extension to other optic nerve, chiasm, optic tract
| ◊ Most common | › | cause of optic nerve enlargement |
| › | primary tumor of optic nerve | |
| › | intraconal tumor of childhood | |
| › | CNS neoplasm in NF1 |
Frequency: 1% of all intracranial tumors; 4% of orbital masses; 80% of primary tumors of optic nerve
Path: optic nerve is embryologically part of hypothalamus and develops gliomas instead of schwannomas
(a) perineural spread = fusiform enlargement of optic nerve: boundary between tumor and nerve often indistinguishable, overlying dura stretched but intact
(b) subarachnoid spread = tumor predominantly involves subarachnoid space surrounding a relatively spared nerve: infiltration through pia mater but contained by dura
Histo: proliferation of well-differentiated astrocytes
= low-grade glial neoplasm with cystic components
(a) in children (most common): juvenile pilocytic astrocytoma = grade 1 WHO with spindle-shaped astrocytes having hairlike (pilocytic) processes ± eosinophilic degenerative cell processes (Rosenthal fibers)
(b) in adults: glioblastoma
Mean age: 4–5 years; 1st decade (75%); rare in adults without NF1 (GBM); M÷F = 1÷2 to 2÷3
Associated with: neurofibromatosis type 1 (NF1) in 10–33–50% (± bilateral optic gliomas)
◊ 15–21% of children with NF1 have (often bilateral) optic nerve gliomas
◊ 10% of all optic nerve gliomas are associated with neurofibromatosis
• decreased visual acuity / visual-field deficit
• optic disc edema, pallor, atrophy (axonal damage)
• abnormal pupillary reflex; relative afferent pupillary defect
• axial proptosis with larger masses (less common)
• vision loss, strabismus
• spasmus nutans (= high-frequency nystagmus of low amplitude associated with head nodding movement)
• precocious puberty with accelerated growth (in 39% of only NF1 patients) ← involvement of optic chiasm + hypothalamus
Location: any part of optic pathway (intraorbital optic nerve in 25–48%); unilateral (most common); bilateral / multifocal (PATHOGNOMONIC for NF1); involvement of chiasma (more common in sporadic cases without NF1)
Extension to: intracanalicular + retrocanalicular optic nerve; lateral geniculate body and optic radiation (rare)
√ tubular / fusiform / excrescentic well-circumscribed homogeneous enlargement of optic nerve-sheath complex:
√ CHARACTERISTIC kinking / buckling of nerve
√ posterior extension to involve chiasm + hypothalamus in 25–60% (indicates nonresectability)
√ ipsilateral optic canal enlargement (90%) > 3 mm / 1 mm difference compared with contralateral side
CT:
√ iso- to slightly hypodense compared to normal optic nerve
√ variable contrast enhancement (less intense than meningioma)
√ calcifications (rare)
US:
√ well-defined homogeneous mass of medium echogenicity inseparable from optic nerve
MR: more sensitive than CT in detecting intracanalicular + intracranial extent
√ fusiform enlargement of nerve (without NF1):
√ effacement of surrounding subarachnoid space
√ tortuous / kinked / buckled diffusely enlarged optic nerve (NF1 patient):
√ tumor in subarachnoid space surrounds normal-sized optic nerve
√ lesion isointense to muscle on T1WI
√ lesion heterogeneously hyperintense on T2WI
√ rim of T2-hyperintensity at tumor periphery (mimicking expanded subarachnoid space) = arachnoidal gliomatosis ← leptomeningeal infiltration + proliferation
√ ± cystic spaces
√ calcifications (rare)
√ nerve indistinguishable from tumor (DDx to meningioma)
√ variable enhancement (in 50%):
√ additional intracranial findings:
√ other gliomas
√ macrocephaly
√ hydrocephalus ← aqueductal stenosis (almost exclusive to patients without NF1)
√ neurofibromatosis spots (= foci of T2 prolongation due to myelin vacuolization)
Cx: precocious puberty ← hypothalamic impingement
Prognosis: slow growth / stability over time; 87–97% 5-year survival
Rx: conservative management; chemotherapy (for young patients), radiation therapy (for patients > 5 years of age)
DDx: optic nerve sheath meningioma (middle age, hyperattenuating mass, plaquelike calcifications, hypointense on T2WI, intense enhancement, no intracranial extension along optic pathway)
Malignant Optic Glioma of Adulthood
Prevalence: extremely rare; 30 cases in this century
Mean age: 6th decade; M÷F = 1.3÷1.0
Histo: anaplastic astrocytoma / glioblastoma multiforme
• rapidly progressive monocular visual loss culminating in monocular blindness within a few weeks
• with retrograde tumor extension: contralateral temporal hemianopia, polyuria, polydipsia
√ focal / diffuse enlargement of optic nerve
√ hypo- to isointense on T1WI + hyperintense on T2WI
√ obliteration of subarachnoid space around affected portion of nerve
√ diffuse intense enhancement of optic nerve
√ thickening + abnormal enhancement of optic nerve sheath
Tumor extension: optic chiasm, hypothalamus, basal ganglia, brain stem, medial temporal lobes, leptomeninges, ependyma
Prognosis: < 1-year survival despite aggressive therapy
DDx: (1) Optic neuritis (demyelinating plaques elsewhere)
(2) Perioptic meningioma (hypointense on T2WI, stippled calcifications, hyperostosis)
(3) Sarcoidosis, lymphoma, orbital pseudotumor (moderately / markedly hypointense on T2WI)
OPTIC NERVE SHEATH MENINGIOMA
= PERIOPTIC MENINGIOMA
Frequency: 2% of space-occupying orbital masses; < 2% of intracranial meningiomas
◊ 2nd most common optic nerve tumor!
Mean age: 49 years; M÷F = 1÷4; slightly more aggressive in children
Occasionally associated with:
neurofibromatosis type 2 (usually in teenagers)
Origin: meningothelial cells in arachnoid sheath of optic nerve in orbit / middle cranial fossa
Histo: syncytial growth pattern composed of meningioma cells with indistinct cytoplasmic margins ± multiple ringlike psammoma bodies (= round calcifications)
• classic clinical triad of retinal examination:
(1) Painless slowly progressive loss of visual acuity over months
(2) Optic nerve atrophy → progressive loss of vision
(3) Optociliary shunt vessels = dilated connections between ciliary circulation + central retinal vessels ← long-term compression of central retinal vein
• proptosis
Location:
(a) orbit = intraoptic nerve sheath meningioma
(b) in optic canal = intracanalicular meningioma
(c) intracranial opening of optic canal = foraminal meningioma
(d) middle cranial fossa
√ tubular (most common) / fusiform / eccentric (excrescentic) thickening of optic nerve
√ calcifications in 20–50% (HIGHLY SUGGESTIVE)
√ sphenoid bone hyperostosis
US:
√ hypoechoic tumor with irregular border
CECT: enhancement is the rule
√ tumor enhancement around nonenhancing optic n.:
√ “tram-track” configuration on axial CECT = enhancing tumor on either side of spared optic nerve
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree