CHAPTER 16
Anomalous Pulmonary Venous Connection
Definition
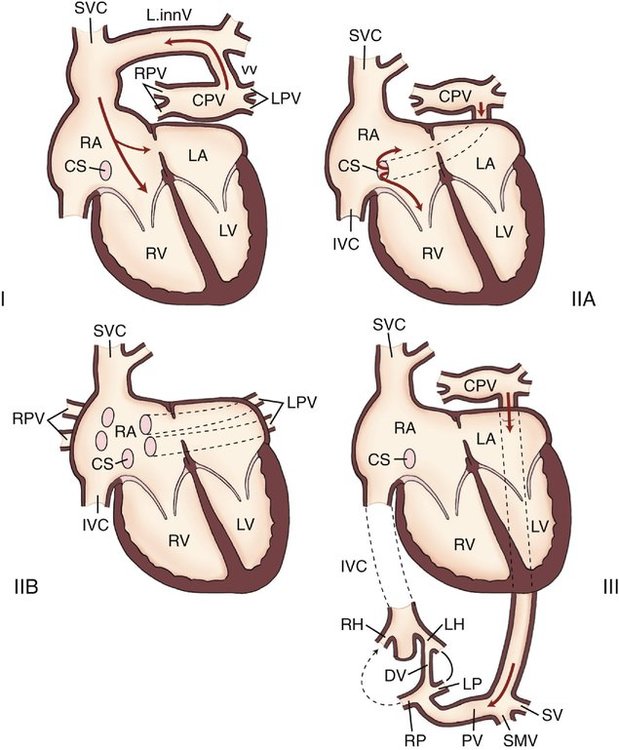
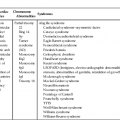
Although several different classification systems have been proposed for TAPVC, the most widely used is that of Craig et al,1 which is based on the anatomical location of the anomalous connection.1 With this system, TAPVC is divided into four categories (Fig. 16–1), listed here in order of frequency:
There is some variation in the reported frequencies for these four types of TAPVC; however, in most large series, the order of frequency is as listed, with supracardiac anomalous connection comprising the majority of cases.2 A large retrospective study reviewed the medical records of 377 children with TAPVC between 1946 and 2005. In this study the anomalous venous connection was supracardiac in 44%, infracardiac in 26%, cardiac in 21%, and mixed in 9%.3
Obstruction to pulmonary venous return can occur at any level between the pulmonary veins (or the common pulmonary venous confluence characteristic of TAPVC) and the right atrium. Obstruction may occur at a discrete level because of intrinsic narrowing of a vessel or compression from external structures, or it may be more generalized as when a large volume of pulmonary venous blood is forced through the liver in the setting of TAPVC of the infracardiac type. Karamlou et al3 found that at the time of presentation 48% of children with TAPVC had some degree of obstruction.
Type I (Supracardiac)
Obstruction is rare with both types of supracardiac connection; however, it may occur when the left vertical vein is compressed between the left main stem bronchus and pulmonary artery or when there is a restrictive connection to the SVC. Complex cardiac malformations are common with anomalous connection to the right SVC.4
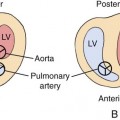
Type II (Cardiac)
In the cardiac type of TAPVC, the anomalous veins empty into the coronary sinus (more common) or into the posterior right atrium directly (less common) or through a short common trunk. Although several studies have suggested that obstruction is rare with direct cardiac connection,5,6 a subsequent series found obstruction in 22% of patients with TAPVC to the coronary sinus.7
Type III (Infracardiac)
In infracardiac TAPVC, the four pulmonary veins generally join to form a confluence posterior to the left atrium. An anomalous descending vein extends from the confluence downward just anterior to the esophagus and accompanies the esophagus through the diaphragm by way of esophageal hiatus. In approximately 80% of cases, the anomalous vein drains into the portal venous system (usually at the portal confluence or splenic vein).1,8 Rarely, this anomalous descending vein empties into one of the hepatic veins, the ductus venosus, or the inferior vena cava (IVC).8
Type IV (Mixed Anomalous Connections)
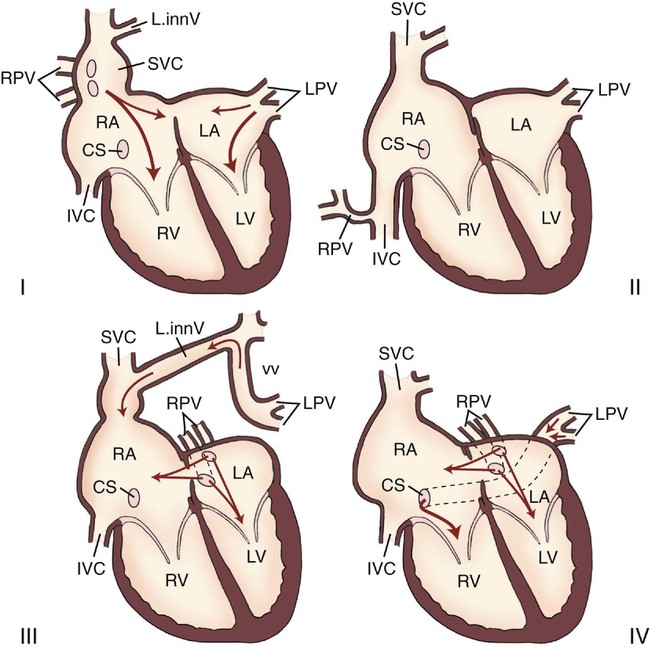
Similar to TAPVC, four common forms of PAPVC are usually described (Fig. 16–2)9,10:
• The right pulmonary veins enter the right atrium via the SVC. The left pulmonary veins enter the left atrium. A sinus venosus ASD is usually present.
• The right pulmonary veins enter the right atrium via the IVC. The left pulmonary veins enter the left atrium. In this form, the atrial septum is usually intact (excluding the normal foramen ovale). This type of PAPVC has been associated with hypoplasia of the right lung, hypoplasia of the right pulmonary artery, dextroposition, and other cardiac anomalies.10
• The left pulmonary veins enter the left innominate vein, which then connects with the SVC and drains into the right atrium. The right pulmonary veins may enter the left atrium, the coronary sinus, the IVC, the SVC, or the left subclavian vein. An ostium secundum ASD is often present. This form of PAPVC has been associated with a variety of cardiac anomalies and syndromes, including polysplenia, asplenia, Turner syndrome, and Noonan syndrome.
• The least common form of PAPVC involves the left pulmonary veins draining into the coronary sinus, the IVC, the SVC, the right atrium, or the left subclavian vein. The right pulmonary veins usually maintain their normal connection to the left atrium.
Embryology
The embryonic lungs, larynx, and tracheobronchial tree are derived from the foregut. The primitive lungs are in close contact with the vascular plexus of the foregut (the splanchnic plexus), a portion of which later forms the pulmonary vascular bed. Initially, there is no direct venous connection between the heart and the lungs, and the pulmonary vascular bed drains with the splanchnic system into the cardinal and umbilicovitelline venous systems. Between 27 and 29 days’ gestation, the common pulmonary vein begins to form from an outpouching located to the left of the septum primum on the roof of the common atrium (Fig. 16–3, A). By gestational day 30, the atrial outpouching (common pulmonary vein) and the pulmonary venous portion of the splanchnic system have joined, forming a direct connection between the heart and the pulmonary veins (Fig. 16–3, B
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree