Summary of Key Points
- •
The goal of antepartum testing is to prevent fetal death.
- •
Antepartum testing is most commonly performed in pregnancies identified as high risk due to maternal conditions or following the identification of fetuses at risk for intrauterine compromise so that intervention and timely delivery can prevent progression to stillbirth.
- •
Antepartum surveillance may also be used to confirm the well-being of the normal fetus so as to prevent unnecessary intervention and iatrogenic prematurity.
- •
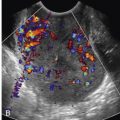
Real-time ultrasonography, including assessment of fetal heart rate patterns and umbilical artery Doppler velocimetry, is a component of antepartum surveillance.
- •
Surveillance techniques include fetal kick counts, nonstress test (NST), contraction stress test (CST), biophysical profile (BPP), modified biophysical profile, and umbilical artery Doppler velocimetry.
Antepartum fetal assessment is used to assess the risk of fetal death in pregnancies complicated by maternal medical problems or fetal compromise. Multiple techniques can be utilized to assess fetal status, including fetal kick counts, nonstress test (NST), contraction stress test (CST), biophysical profile (BPP), modified BPP, and umbilical artery Doppler velocimetry. All of these techniques are aimed at identifying hypoxemic or acidemic fetuses with the intention of providing an opportunity to intervene before permanent damage or death results. As such, antenatal surveillance can be used to screen for fetal compromise when it is suspected (i.e., maternal report of decreased fetal movement) or anticipated (cyanotic maternal heart disease). Ultrasound can be particularly valuable because it provides a real-time view of fetal activity and assessment of the intrauterine environment. Acute events, however, such as abruption or cord accident, cannot be predicted by such techniques.
Serial antepartum surveillance using one or multiple fetal assessment techniques is the standard of care for pregnancies complicated by maternal or fetal complications. There is little evidence from randomized controlled trials that antepartum testing actually decreases the risk of fetal death, and some evidence suggests that it may actually be harmful as a result of increases in the rate of iatrogenic prematurity. Nevertheless, antenatal testing remains a mainstay of prenatal care to assess fetal well-being for a wide range of maternal and fetal indications ( Table 21-1 ). The primary measure of antepartum testing efficacy is the false negative rate, which is defined as the incidence of fetal death within 1 week of a normal test result. Among the aforementioned antepartum testing techniques, false negative rates range from a low of 0.4/1000 for CSTs to a high of 3.2/1000 for NSTs. However, the high false positive rate of various testing protocols (up to 50% with the NST), defined as an abnormal test result in the setting of an uncompromised fetus, limits the utility of interpreting a test in isolation without considering the clinical situation or utilizing subsequent surveillance measures ( Table 21-2 ).
| Maternal Conditions |
|
| Pregnancy-Related Conditions |
|
| Antenatal Test | Risk of Stillbirth/1000 |
|---|---|
| NST (once a week) a | 3.2 |
| NST (twice a week) b | 1.9 |
| BPP c | 0.8 |
| Modified BPP d | 0.8 |
| CST a | 0.4 |
a Freeman RK, Anderson G, Dorchester W: A prospective multi-institutional study of antepartum fetal heart rate monitoring. II. Contraction stress test versus nonstress test for primary surveillance. Am J Obstet Gynecol 143(7):778-781, 1982.
b Boehm FH, Salyer S, Shah DM, Vaughn WK: Improved outcome of twice weekly nonstress testing. Obstet Gynecol 67(4):566-568, 1986.
c Manning FA, Morrison I, Harman CR, et al: Fetal assessment based on fetal biophysical profile scoring: experience in 19,221 referred high-risk pregnancies. II. An analysis of false-negative fetal deaths. Am J Obstet Gynecol 157(4 Pt 1):880-884, 1987.
d Miller DA, Rabello YA, Paul RH: The modified biophysical profile: antepartum testing in the 1990s. Am J Obstet Gynecol 174(3):812-817, 1996.
Assessment of Fetal Movement
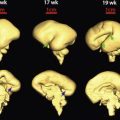
Quickening , or the time at which fetal movement is first perceptible to the mother, typically occurs at about 19 to 20 weeks. With advancing gestation, fetal movement becomes more pronounced and peaks at approximately 38 weeks. Periods of active movement generally last about 40 minutes whereas quiet periods last about 20 minutes. The fetus is most active between 9:00 pm and 1:00 am , which correlates with falling maternal glucose levels.
Fetal physiology studies performed in the setting of growth-restricted fetuses demonstrate that fetal movement decreases with increasing hypoxia. Thus, maternal assessment of fetal movement is a potentially simple and inexpensive method of monitoring fetal well-being. Physicians routinely inquire about fetal activity as part of the standard prenatal visit. In the low-risk pregnancy, this technique is often the only form of fetal surveillance that is performed.
Numerous protocols can be used for quantifying normal movement; however, there are no high-quality studies indicating a superior methodology or parameters for normal amounts of fetal movement. Most often, women are advised to do “kick counts” by lying on their side and counting the number of fetal movements. The perception of 10 distinct movements in 2 hours is commonly regarded as reassuring. Once 10 movements have been recognized by the mother, the count may be discontinued. Kick counts can be repeated as often as daily. It may, however, be just as useful to encourage the mother to report any change from what she perceives as “normal.”
Multiple factors other than deteriorating fetal status can affect maternal perceptions of movement, including gestational age, placental location, medications, maternal activity, position, and obesity. However, decreased fetal movement has been associated with an increased risk of stillbirth. Further evaluation, therefore, is always warranted once decreased maternal perception of fetal movement is reported both to exclude potentially reversible factors that may be responsible and to ensure fetal well-being.
There is only one randomized controlled trial evaluating formal fetal movement counting. During this study, over 68,000 low-risk women were enrolled and randomized to regular fetal movement evaluation (intervention group) or routine care (control group). The antepartum death rate was statistically equal in both groups, 2.9/1000 in the intervention group versus 2.7/1000 in the control group. Reporting compliance was a major limitation of this study and may have affected the results. Only 46% of women in the intervention group were compliant in reporting decreased fetal movement. In contrast, a prospective cohort study performed in Norway found that providing written information about fetal activity, including a definition of what constitutes decreased fetal movement, as well as an invitation to monitor fetal movements via kick charts, reduced the incidence of stillbirth by almost 50% in women who presented with a complaint of decreased fetal movement (odds ratio [OR] 0.51, 95% confidence interval [CI] 0.32-0.81). There have been no randomized controlled trials evaluating fetal movement counting in women with high-risk pregnancies. A systematic review published in the Cochrane Database concluded that there is insufficient evidence to recommend routine fetal movement counting to prevent stillbirth.
Nonstress Test
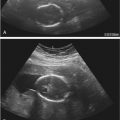
The NST is the most common screening test used in antepartum surveillance. A cardiotocograph, or external fetal monitor, is used to simultaneously record the fetal heart rate (FHR) and maternal uterine activity with Doppler ultrasound transducers that are placed on the maternal abdomen. NST interpretation is based on the premise that a healthy, well-oxygenated fetus will demonstrate accelerations of the heart rate with movement. During an NST, the uterus is quiescent (hence the term nonstress ) and the FHR is evaluated for a period of up to 20 minutes, although it may be extended for up to 40 minutes to allow for variations in the fetal sleep-wake cycle. The FHR pattern, including baseline heart rate, variability, and the presence or absence of accelerations and decelerations are evaluated in NST interpretation ( Figs. 21-1 and 21-2 ). These parameters reflect a fetus’s ability to adapt effectively to the intrauterine environment and can give the provider information about fetal well-being.


The FHR baseline is regulated by the autonomic nervous system. The parasympathetic innervation of the heart is mediated by the vagus nerve and is responsible for a chronotropic effect that slows down the FHR, as well as an oscillatory effect that alters R wave intervals, resulting in the heart rate variability. The sympathetic nervous system, on the other hand, releases norepinephrine when stimulated, which accelerates the FHR and improves inotropy, or contractility. The FHR baseline is the average number of beats per minute (rounded to 0 or 5) over a 10-minute period. Periods of marked variability (amplitude of the FHR greater than 25 beats per minute above the baseline) should not be used to determine the baseline. Additionally the baseline should be identifiable for at least 2 minutes during the NST, although the 2 minutes may not be contiguous. Most clinicians do not use a computerized model to determine baseline and instead “eyeball” the tracing, leading to subjectivity in interpretation. Additionally, the baseline may be indeterminate, meaning the NST cannot be interpreted. The normal baseline FHR ranges from 110 to 160 beats per minute; the baseline is usually in the higher end of the normal range early in gestation and decreases as gestation advances.
Variability refers to the expected fluctuations in the baseline FHR that are irregular in amplitude and frequency and are quantified as the amplitude of the peak-to-trough in beats per minute. Variability can be absent, minimal, moderate, or marked ( Fig. 21-3 ). Moderate variability, in which the amplitude ranges between 6 and 25 beats per minute, is considered reassuring. FHR variability is rare before 24 weeks but should be present after 28 weeks. Absence of variability in the third trimester should be considered abnormal until further evaluation. Tracings demonstrating minimal variability (amplitude less than 6 beats per minute) or absent variability (amplitude range is undetectable) warrant further investigation, especially when the gestational age is in the mid- to late third trimester.

Accelerations are defined as a visually abrupt increase in FHR with onset to peak less than 30 seconds. In a fetus that is 32 weeks’ gestation or greater, the acceleration should peak at least 15 beats per minute above the baseline and persist for at least 15 seconds from baseline to baseline. In a fetus younger than 32 weeks the peak of the acceleration should be at least 10 beats per minute above baseline and persist for at least 10 seconds.
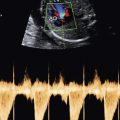
Decelerations are classified as late, early, or variable ( Fig. 21-4 ) and differ in their onset, nadir, and recovery in relation to uterine contractions. Each type of deceleration has a different cause (hypoxemia, head compression, and cord compression, respectively). Correct identification of the type of deceleration can therefore impact FHR interpretation and management.

A sinusoidal FHR is relatively rare and is defined as a smooth, sine wave–like undulating pattern in the FHR baseline with a cycle frequency of 3 to 5/minute that persists for over 20 minutes ( Fig. 21-5 ). This pattern is highly associated with fetal anemia. It is considered abnormal and requires prompt attention. Given the association with fetal anemia, assessment by measurement of the peak systolic velocity of the fetal middle cerebral artery (MCA) using Doppler velocimetry is warranted in the absence of a known cause (see Chapter 22 ).

Ultimately, the NST is interpreted as “reactive” or “nonreactive.” A reactive NST is defined as the presence of at least two accelerations of the FHR 15 beats per minute or greater above the baseline for a minimum of 15 seconds within a 20-minute period of monitoring. A nonreactive NST lacks the appropriate number of accelerations or doesn’t meet criteria for acceleration but does not demonstrate absence of variability or decelerations. In 2008, the Eunice Kennedy Shriver National Institute of Child Health and Human Development in conjunction with the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine published recommendations for the terminology and interpretation of FHR tracings and described a new three-tiered system. Although the emphasis in this report is on intrapartum FHR patterns, these definitions may also be extrapolated to the antepartum setting ( Figs. 21-6 through 21-8 and Table 21-3 ).



| Category I |
| Category I fetal heart rate (FHR) tracings that include all of the following: |
|
| Category II |
| Category II tracings include all FHR tracings not categorized as category I or category III. Category II tracings may represent an appreciable fraction of those encountered in clinical care. Examples of category II FHR tracings include any of the following: |
| Baseline Rate |
|
| Baseline FHR Variability |
|
| Accelerations |
|
| Periodic or Episodic Decelerations |
|
| Category III |
| Category III FHR tracings include either: |
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree