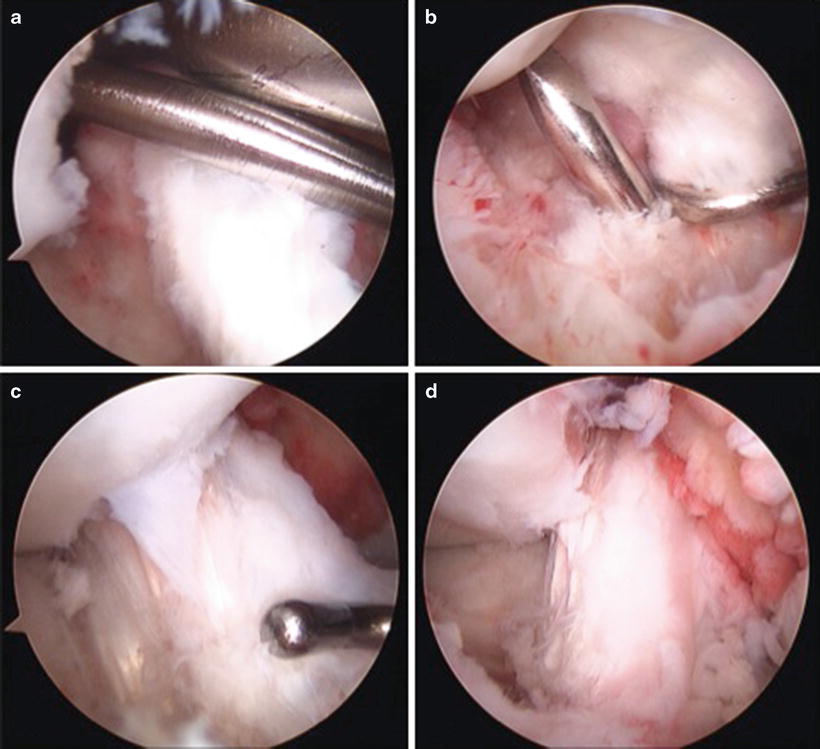
Fig. 5.1
(a, b) T2 sagittal image is shown demonstrating absence of the ACL as well as the typical bone bruise pattern. Coronal T2-weighted image demonstrates the “empty notch sign”
A complete midsubstance ACL tear was present as shown in Fig. 5.2a, b. Acute hemarthrosis was present with a typical bone contusion pattern present as shown in Fig. 5.3. The ACL is seen as an edematous mass without the typically taught fibers. The lateral meniscus visualized best on the sagittal T2-weighted image (Fig. 5.3) showed no meniscal tear. The medial meniscus was intact as was the MCL. No posterior cruciate ligament or articular cartilage pathology was present. The patella tendon was partially disrupted with a wavy appearance to a portion of its fibers (Fig. 5.2b).
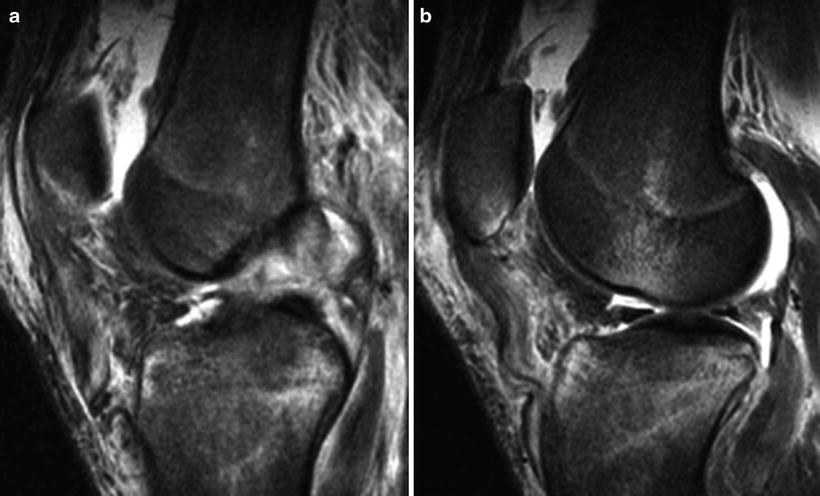
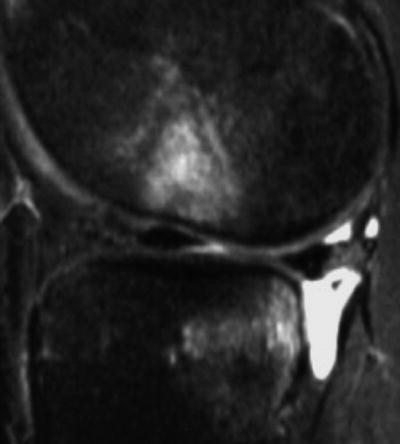
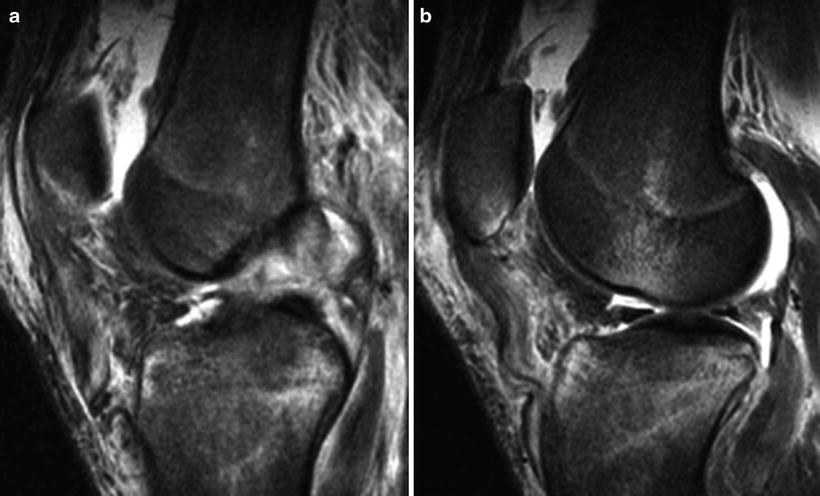
Fig. 5.2
T2 sagittal imaging demonstrates edema within the substance of the ACL with complete disruption (a). Partial tearing of the patella tendon is seen at this level (b)
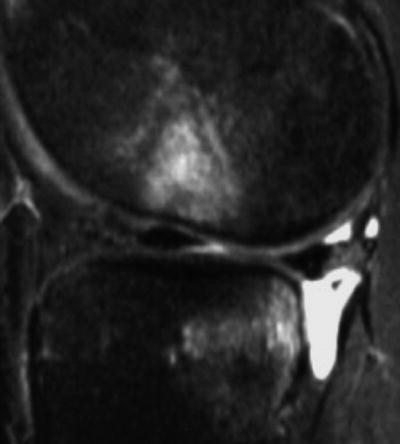
Fig. 5.3
The typical bone bruise pattern is shown on T2-weighted imaging about the lateral femoral condyle and posterolateral tibial plateau. Additionally, the tibia is noted to be translated forward relative to the posterior aspect of the distal femur producing an “anterior drawer” on imaging
MRI allowed for confirmation of ACL tear as well as diagnosis of a patella tendon disruption of uncertain severity. This was consistent with the patient’s clinical examination; therefore, risks and benefits of operative intervention were discussed with the patient. He elected to proceed with possible patella tendon repair and planned reconstruction of the ACL given his age and hopes to continue to compete at a collegiate level.
Arthroscopy
The patient was taken to the operating room and placed supine with a post placed in the appropriate position. Given recent evidence suggesting graft size is an important factor in ACL reconstruction failure, we typically prep in the other lower extremity when utilizing hamstring graft to reserve the ability to take contralateral graft if needed. The hamstring tendon graft was harvested in the usual fashion. The graft was prepared on the back table, and a standard diagnostic arthroscopy of the knee was completed. The ACL was completely absent with a remaining stump seen demonstrated in Fig. 5.4 with no intact fibers remaining. The articular cartilage and medial meniscus were found to be intact. This correlated well with the findings on MRI.


Fig. 5.4
Arthroscopic visualization of the intercondylar notch reveals a complete tear of the ACL with fibrous proliferation and remaining stump on the tibial side
Following diagnostic arthroscopy, the tibial footprint and ACL over the top position in the back of the notch were debrided using arthroscopic baskets and shaver. Next, the appropriate position off the back of the posterolateral notch was chosen for guide pin placement (Fig. 5.5a). An offset guide can be used here to retain 1–2 mm of posterior wall following drilling. We like to use an accessory medial (AM) portal for separate femoral tunnel drilling to allow more horizontal, anatomic femoral tunnel drilling with the knee in hyperflexion (Fig. 5.5b) [8].
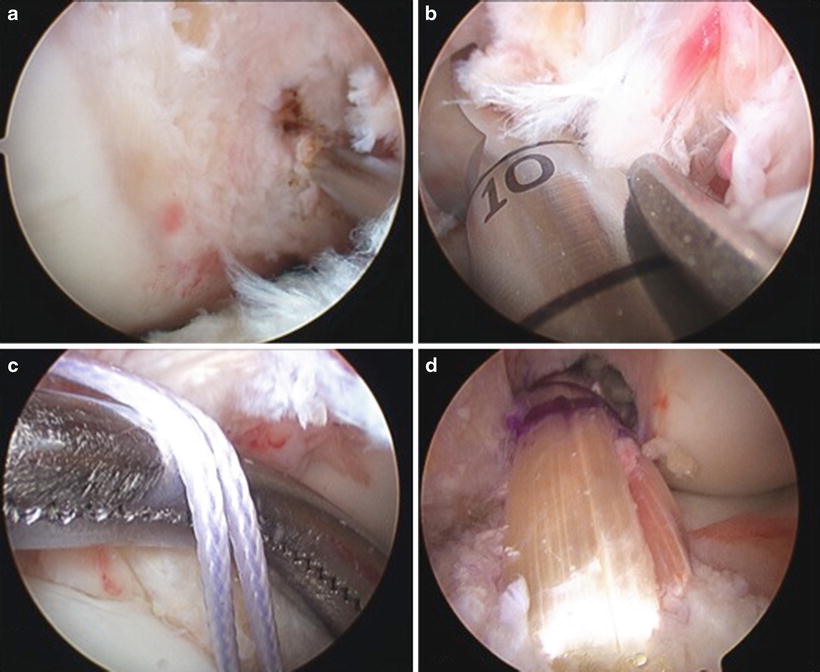
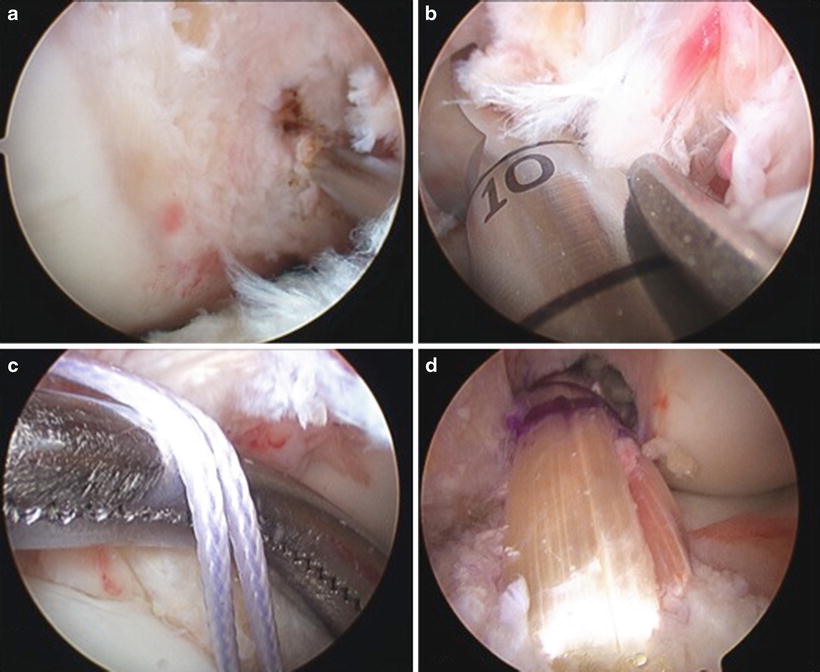
Fig. 5.5
ACL reconstruction steps are shown with placement of a guide pin in the anatomic position utilizing an accessory inferomedial portal (AM portal) (a). Femoral tunnel drilling is performed with a skid in place in hyperflexion to protect the femoral condyle (b). Both needle and suture are passed through the tunnel to allow for graft shuttling (c). The autograft is fixed with interference screw fixation (d)
Once the femoral tunnel is drilled to the appropriate depth, a commercially available tibial guide is used to place a guide wire for the tibial tunnel using intra-articular landmarks. Once the tibial tunnel is prepared, a Beath needle is used to pass the graft utilizing suture (Fig. 5.5c), and it is fixed on the femoral side with an interference screw. Once the femoral side is fixed, the knee is cycled through the complete ROM, and the graft is tensioned and the tibial side fixed. The final graft was inspected and noted to have excellent tension in Fig. 5.5d. Finally, the patella tendon was repaired using a Krackow suture technique as shown in Fig. 5.6a, b.
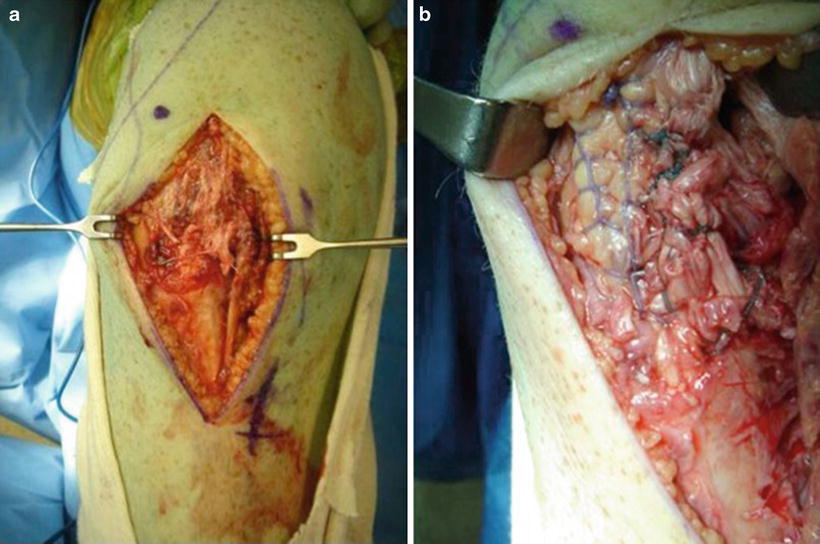
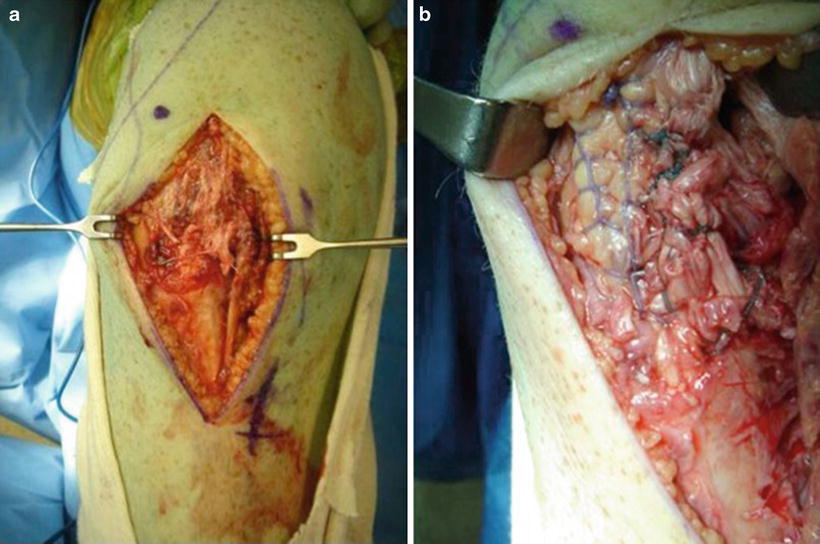
Fig. 5.6
Intraoperative photo demonstrates a partial patella tendon rupture (a). This is repaired primarily utilizing Krackow suture technique (b)
Discussion
MRI demonstrated a complete ACL tear. Several direct MRI signs suggest complete disruption of the ACL in this case. The ACL is discontinuous and does not have the turgor of a normal ACL (Fig. 5.1a). This is best examined on MRI in the sagittal plane where the fibers seen on the T2-weighted image as no longer taught. In the acute setting, the ACL appears as an edematous mass, producing the so-called empty notch sign where fluid rather than ACL fills the intercondylar notch (Fig. 5.1b).
The indirect signs of an ACL injury on MRI are also seen here including the typical hemarthrosis, though this is a largely nonspecific finding. Additionally, the characteristic bone bruise pattern is noted about the lateral femoral condyle and posterolateral tibial plateau due to the prior pivoting event (Fig. 5.3). Often an anterior drawer can be seen where the tibia sits slightly more anterior to a line drawn parallel to the posterior aspect of the distal femur (Fig. 5.3). A Segond fracture which is noticeable on X-ray can also be seen on MRI as shown in the T1 image in Fig. 5.7. The PCL may also appear buckled in some cases.


Fig. 5.7
T1-weighted coronal image demonstrates a Segond fracture
Case 2: Partial ACL Rupture
History/Exam
A 20-year-old female collegiate soccer player sustained a noncontact injury to her left knee during play. She was seen on the sidelines and noted to have a sizeable effusion and pain with knee range of motion and was unable to return to play. She was subsequently seen in our sports medicine clinic several days later and exhibited an ongoing effusion.
Physical examination of the knee demonstrated no opening with varus or valgus stress. A pivot shift was not possible in the office due to her pain and swelling. She did however have a 2+ Lachman’s on her symptomatic side as compared to her asymptomatic side. Patellar apprehension testing was negative as was McMurray’s provocative maneuvers. Given the patient’s desire to continue to play collegiate soccer and her examination, advanced imaging was obtained to confirm suspected ACL injury and evaluate for additional pathology.
Imaging
Initial plain radiography was unremarkable for any bony abnormality. Given the persistent symptoms, concerning examination and effusion, MRI without contrast was obtained. A complete sequence of images was obtained, including sagittal gradient, STIR, proton density, coronal gradient and fat-saturated T2, and axial fat-saturated T2 without contrast. Coronal T2-weighted images and sagittal images are demonstrated in Fig. 5.8a, b.
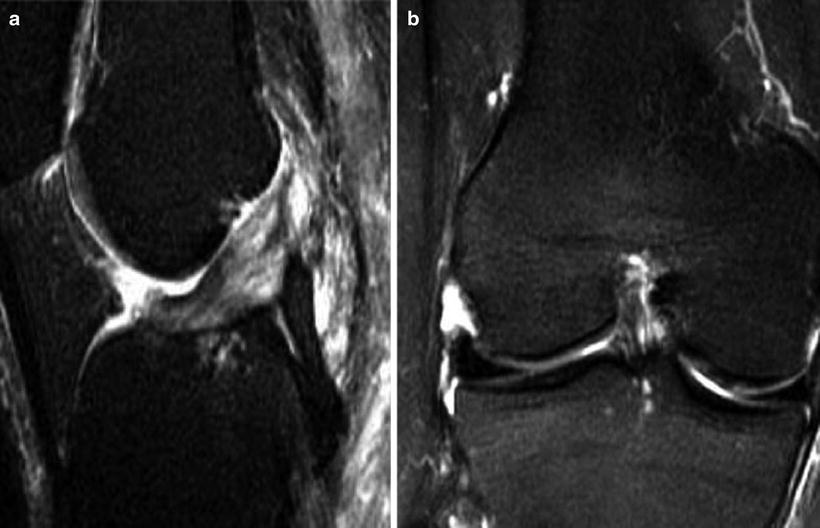
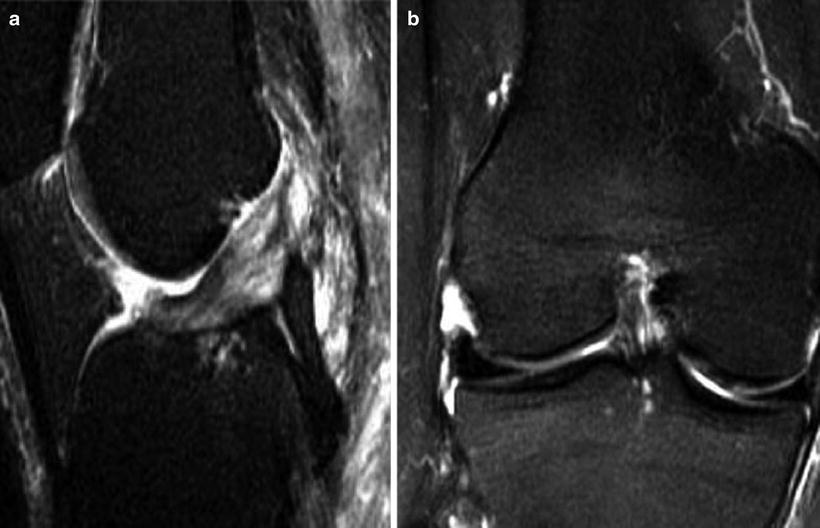
Fig. 5.8
Sagittal MRI demonstrates edema within the ACL with remaining intact fibers (a). The coronal plane imaging is shown which reveals increased fluid and potential disruption in the anteromedial aspect of the tibial footprint (b)
The sagittal images showed no abnormality in the medial and lateral meniscus with a normal cartilage layer throughout. The ACL visualized in the sagittal plane T2 weighted revealed increased signal evident within the substance of the ACL with some remaining continuity (Fig. 5.8a). The PCL, LCL, and MCL were all intact with no focal abnormalities. In the coronal plane, the more medial portion of the ACL attachment to the tibial spine was noted to have increased edema and possible midsubstance tearing (Fig. 5.9a, b). No significant bony edema was seen in the STIR sequences.
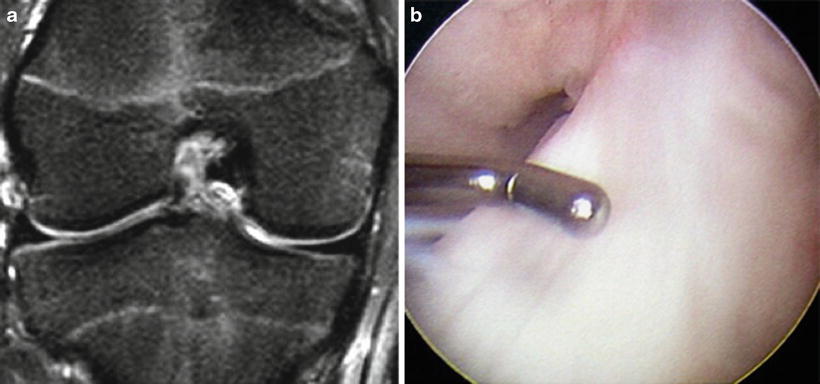
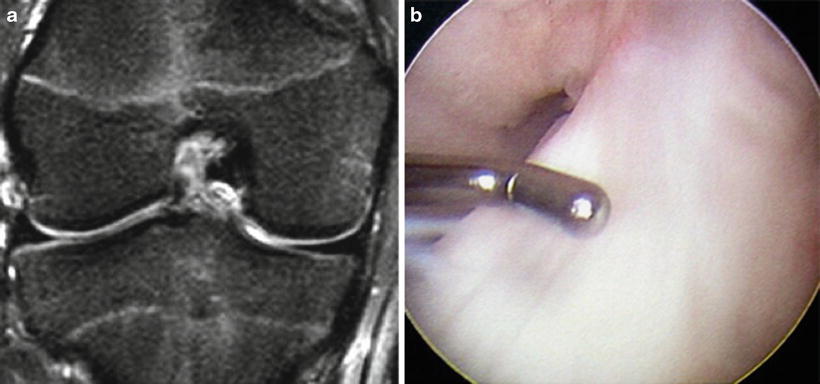
Fig. 5.9
A partial empty intercondylar notch is shown on coronal T2-weighted MRI (a). A partially intact ACL is shown on arthroscopy (b)
The patient’s history, physical exam, and MRI were consistent with an ACL tear though MRI imaging was not convincing of a complete ACL injury. A lengthy discussion was had with the patient and her family, trainer, and coach regarding the risks and benefits of watchful waiting versus early arthroscopic exploration and possible reconstruction. They elected to undergo arthroscopy as opposed to attempted early rehabilitation, with a plan to address her ACL with reconstruction if found to be compromised.
Arthroscopy
On the day of surgery following a preoperative nerve block, the patient was taken to the operating room and placed supine upon the operating room table and positioned for ACL reconstruction given our suspicion of ACL injury. Examination under anesthesia was performed as previously described. If the examination is unclear, a diagnostic arthroscopy is always performed before harvesting graft. Again under anesthesia, a Lachman was performed which showed side-to-side difference with a soft end point. A nonsterile tourniquet was placed around the operative extremity. Standard inferolateral and inferomedial portals were made and a diagnostic arthroscopy completed to establish whether her ACL was in fact torn. We evaluated the patellofemoral joint, medial and lateral gutters, and compartments to assess for any meniscal disease, loose bodies, or cartilage injury of which none were found.
Visualization of the notch of the ACL demonstrated a partial ACL injury as shown in Figs. 5.9a, b and 5.10a, b. The posterolateral bundle of the ACL appeared intact and taught. The anteromedial bundle however was not intact, and a residual stump was present on the tibial side from the prior attachment. The rest of the diagnostic scope was unremarkable for chondral damage or meniscal injury. Given the patient’s expectations preoperatively and her current activity as a collegiate soccer player, decision was made to perform arthroscopic-assisted ACL reconstruction.
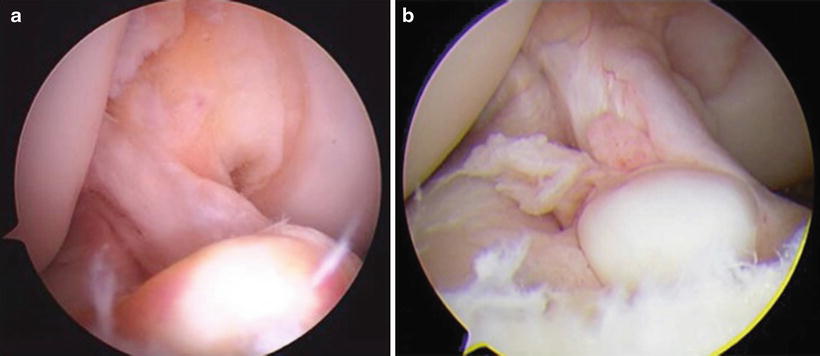
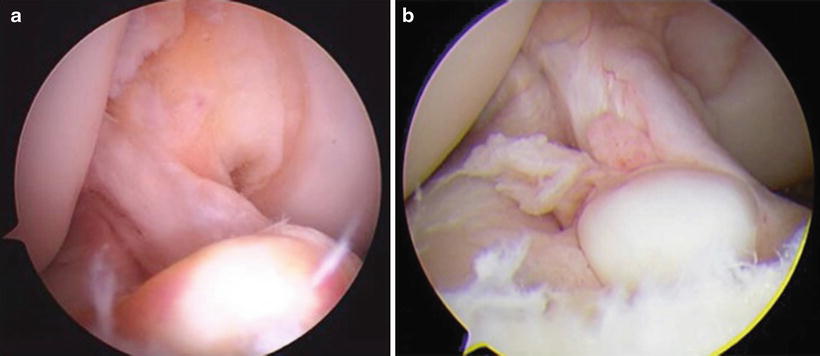
Fig. 5.10
Arthroscopic visualization of the notch demonstrates intact posterolateral bundle (a) with obviously less caliber than a typical ACL. The remaining stump of likely the anteromedial bundle of the ACL is seen as a cyclops lesion on the tibial side (b) with some remaining intact fibers shown
Although several graft options are available, autograft is a common graft option and has been demonstrated to lead to lower failure rates than allograft options in young patients [10]. In this case bone patella bone and hamstring autograft are reasonable options for this young athlete. With a combination of arthroscopic punch, motorized shaver, and electrocautery as needed, the ACL footprint was debrided. After debriding the ruptured ACL fibers, tunnels are drilled in the tibia and femur for the prepared grafts after sizing (Fig. 5.11a–d). In our hands, grafts are subsequently fixed utilizing interference screw fixation. We prefer to place the tibial tunnel in the posteromedial aspect of the ACL footprint and the femoral tunnel in the 10–10:30 position for the right knee leaving 2 mm of posterior wall in a more horizontal graft orientation. We performed a single-bundle technique utilizing an accessory inferomedial portal for guide wire placement and independent femoral drilling to allow for more anatomic graft placement [7, 8] (Fig. 5.11d). This portal is approximately 3–4 cm medial to the patellar tendon though should be localized under arthroscopy. Double-bundle techniques and individual-bundle techniques are described though they have not been widely adopted by most surgeons [11, 12].