The lifetime prevalence of epilepsy ranges from 2.7 to 12.4 per 1000 in Western countries. Around 30% of patients with epilepsy remain refractory to antiepileptic drugs and continue to have seizures. Noninvasive imaging techniques such as functional magnetic resonance imaging (fMRI) and diffusion tensor imaging (DTI) have helped to better understand mechanisms of seizure generation and propagation, and to localize epileptic, eloquent, and cognitive networks. In this review, the clinical applications of fMRI and DTI are discussed, for mapping cognitive and epileptic networks and organization of white matter tracts in individuals with epilepsy.
Key points
- •
Language-related networks can be mapped noninvasively using functional magnetic resonance imaging (fMRI). Verbal fluency paradigms can provide lateralization of the Broca area; however, further paradigm development is needed to predict naming difficulties after temporal lobe resection.
- •
Functional imaging can map memory-related networks noninvasively, and word encoding shows promise for detecting verbal memory decline after temporal lobe resection.
- •
Simultaneous electroencephalography (EEG)-fMRI can localize interictal and seizure-related blood-oxygen-level-dependent networks noninvasively, in concordance with intracranial EEG-based localization, which may be helpful in surgical planning.
- •
Tractography can be used to minimize visual field defects in patients undergoing temporal lobe resection.
- •
Multimodal image integration can combine fMRI and diffusion tensor imaging maps for visual display, which can be helpful in reducing the risk of surgical damage to the eloquent cortex.
Applications of functional magnetic resonance imaging in epilepsy
The life time prevalence of epilepsy ranges from 2.7 to 12.4 per 1000 in western countries. Around 30% of patients with epilepsy remain refractory to antiepileptic drugs and continue to have seizures. Over the last decade, non-invasive imaging techniques such as functional magnetic resonance imaging (fMRI) and diffusion tensor imaging (DTI) have helped to better understand mechanisms of seizure generation and propagation, and to localize epileptic, eloquent and cognitive networks. This review considers the clinical applications of fMRI and DTI, for mapping cognitive and epileptic networks and organization of white matter tracts in individuals with epilepsy.
Increased neuronal activity secondary to a task performance causes variations in the cerebral blood flow, blood volume, and blood oxygenation. This situation results in changes in the ratio of oxyhemoglobin and deoxyhemoglobin concentrations in brain, which is detected as blood-oxygen-level-dependent (BOLD) effect by functional magnetic resonance imaging (fMRI) in specific brain areas that are recruited during the task. Therefore, fMRI provides an indirect measure of neuronal activity. Functional MR imaging has been used to map language and memory networks before and after surgery with high spatial resolution. Simultaneous recording of electroencephalography (EEG) and fMRI can map BOLD networks associated with interictal epileptiform discharges (IED) and seizures in focal and generalized epilepsy.
Language-Related Blood-Oxygen-Level-Dependent Networks in Epilepsy
fMRI can map language networks in patients with refractory epilepsy undergoing epilepsy surgery for research and clinical purposes. Various language paradigms to activate anterior (Broca area: expressive language) and posterior (Wernicke area: comprehension; anterior temporal lobe: semantic integration) language areas have been used to lateralize typical and atypical language representation. Verbal fluency, verb generation, and semantic decision tasks are commonly used tasks for language evaluation in a clinical context, providing complementary information. Verb generation causes more discrete activation, whereas verbal fluency activates language-related areas that are not found with the former. Language lateralization via fMRI has been compared with neuropsychological evaluation, cortical stimulation, or Wada test. Real-time fMRI analysis can improve the processing speed of fMRI data analysis and has good concordance of language localization with conventional general linear model–based analysis or cortical stimulation.
Statistical threshold
Lateralization index (LI) is calculated to detect hemispheric dominance for language networks on fMRI maps, comparing activations in the left and right hemispheres. Choice of details (eg, selecting whole brain or prespecified regions or excluding midline structures for calculating LI) may affect lateralization. Choosing appropriate statistical thresholds is an important issue when evaluating language dominance using fMRI, because the extent and thus localization of fMRI activation depends on the former. Conventional threshold, adaptive threshold, and bootstrap techniques have been used to assess the laterality of language-related fMRI maps. The bootstrap technique is particularly advantageous in that it is more specific and accurately identifies outliers. To avoid dependence of language lateralization on arbitrarily selected statistical thresholds and LI, threshold-independent scores have been used and compared with the Wada test, providing language lateralization at individual level. Data-driven approaches have been used to localize language networks in patients with focal epilepsy and have shown significant differences in language organization, as an effect of epilepsy, which were not seen previously with conventional fMRI analysis. Pattern classifying algorithms have also been used to classify language-related fMRI maps automatically, corroborating with existing LI and visual rating classification methods. For most purposes, comparing left and right activations using the bootstrap method is most satisfactory.
Localization of language networks
Patients with left hemisphere or left temporal lobe epilepsy (TLE) have a higher likelihood of atypical language lateralization than patients with an epileptic focus in the right hemisphere or right temporal lobe. Patients with left TLE with hippocampal sclerosis (HS) and left language dominance have increased recruitment of homologous right hemisphere in addition to left hemisphere language areas for language processing, suggesting widespread language representation and greater cognitive effort performed compared with controls. There is an increase and posterior shift of language-related activation in the right inferior frontal gyrus (IFG) after left hemisphere injury. However, activations in left IFG remain in the same location. Compared with patients with frontal lobe epilepsy (FLE), patients with TLE have more atypical language in the Wernicke area, whereas a frontal focus affects anterior language areas more. In comparison, patients with nonlesional TLE and right TLE show left lateralized language. There is coupling between functional and structural measures for left language lateralization in the patients with right TLE, and decoupling between the functional and structural indices of the patients with left TLE, suggesting complex language networks in left TLE. Language areas activated for abstract and concrete words are also different for patients with TLE, with or without HS, suggesting that HS is associated with altered functional organization of cortical networks involved in lexical and semantic processing. Atypical language representation may also occur in patients with normal structural MR imaging, mesial temporal sclerosis, focal cortical lesions, and stroke.
Language lateralization deduced from fMRI concurs with the Wada test in 80% to 90% of patients when using conjunction analysis of 3 language paradigms or semantic decision paradigm, suggesting the clinical usefulness of the test. Concordance between fMRI and Wada test is the highest for patients with right TLE with left language dominance and for frontal language areas; and the lowest for patients with left TLE with left language dominance. Atypical language dominance on fMRI and interhemispheric language dissociation are correlated with Wada/fMRI discordance. This finding suggests that fMRI may be more sensitive than Wada or cortical stimulation to map the whole network involved in language processing but is less specific at individual level compared with cortical stimulation. fMRI language localization can replace Wada test in most patients. However, Wada test may still be required when a patient cannot perform the fMRI task, for example, because of having a pacemaker or suffering claustrophobia, for validation of atypical language representation on fMRI or for the evaluation of selective language areas near structural abnormalities.
Also, functional connectivity is reduced and reorganized in patients with TLE or intractable epilepsy within the language network. More specifically, functional connectivity is decreased in the left hemisphere irrespective of the epileptogenic focus and frontotemporal network, which is associated with impaired performance on language assessment. Performance on language tasks is also correlated to networks in posterior temporal regions showing increased functional connectivity for both patients with left and right medial TLE.
Language lateralization decreases, and reorganization in frontal, temporal and parietal language networks increases, with earlier age of seizure onset but is not associated with type and location of lesion (acquired or developmental), symptoms, and gender. However, others have not found any association between language lateralization and age of seizure onset but have found an association between language lateralization and handedness, location and nature of pathologic substrate, and duration of epilepsy. Verbal memory performance on neuropsychological evaluation is also found to be associated with language lateralization, suggesting a link between inferior frontal cortex and hippocampus. Gray matter in language networks increases in the hemisphere contralateral to the epileptic focus, and recruitment of the contralateral hemisphere in language processing in patients with atypical language representation may suggest compensatory reorganization mechanisms.
A relative decrease in cerebral blood flow in the left Wernicke area is correlated with decreased activation in the left IFG and LI, suggesting distributed but interconnected language networks. γ Activity in higher frequency range increases and is positively correlated with BOLD responses in the inferior frontal and middle temporal gyri. This γ activity lasts longer in the frontal lobe and declines quickly in the temporal lobe, which may explain difficulties in detecting BOLD in the temporal lobe.
Language fMRI activations of polymicrogyric cortex over Broca area suggest that it retains functionality, and surgical resection should be considered with caution. In patients with generalized epilepsy, fMRI has shown that language function is impaired, as represented by reduced suppression of the default mode network, an inadequate suppression of activation in the left anterior temporal lobe and the posterior cingulate cortex, and an aberrant activation in the right hippocampal formation. Children with benign epilepsy with centrotemporal spikes (BECTS) and other epilepsy types also show bihemispheric language networks, which may represent a compensatory response for ongoing epileptic activity in brain. Also, anterior language networks are affected more in BECTS, resulting in language difficulties for functions dependent on the integrity of anterior language regions (eg, sentence production).
Prognostic value
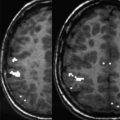
Language mapping using fMRI is more accurate than Wada test in predicting naming postoperatively. Activation in the left hippocampus during verbal fluency task, in patients with right TLE, is associated with preserved naming function. In contrast, patients with left TLE, who are more proficient in naming, involve left frontal lobe, suggesting compensatory responses caused by ongoing epileptic activity in the left hippocampus. Preoperative language fMRI activation with verbal fluency in the left middle frontal gyrus (MFG) can be used to predict significant naming decline in patients with left TLE, with good sensitivity but suboptimal specificity ( Fig. 1 ). Auditory and visual naming paradigms may give more specific prediction of naming difficulties after anterior temporal lobe resection (ATLR).
Postoperative findings
In postoperative patients with left TLE with left hemispheric language dominance, language representation is more bihemispheric than in controls and patients with right TLE, suggesting that redistribution of language to temporofrontal and interhemispheric areas represent reorganization of language function. Postoperative activation in the right MFG and remaining left posterior hippocampus was correlated with better naming for patients with and without significant naming decline, respectively, again suggesting reorganization in language networks after surgery (see Fig. 1 ). Proficient reading skills after left ATLR depend on integration between normal systems involving the left middle temporal, right hippocampus, and anterior superior temporal sulcus, and recruitment of the right IFG, which is not activated in controls.
Effect of epileptic activity and antiepileptic drugs
Antiepileptic drugs can affect cognitive processing. Topiramate has an effect on activation in the basal ganglia, anterior cingulated, and posterior visual cortex and can cause reduced deactivation of the default mode network-related areas during a language task, suggesting interference in cognitive processing. There has also been some evidence suggesting that atypical language reorganization/dominance may be affected by the presence and absence of ongoing epileptic activity. Chronic frequent interictal epileptic activity in left temporal lobes may be associated with a left-right shift of language representation. Also, atypical language lateralization in the right hemisphere may shift back to the left hemisphere in seizure-free patients after left selective amygdalohippocampectomy.
Memory-Related Blood-Oxygen-Level-Dependent Networks in Epilepsy
Memory impairment is common in patients with epilepsy. Working and long-term memory (autobiographical memory [AM], verbal, visual memory) may become affected, in a material-specific way, based on the site of lesion in TLE and FLE. Functional imaging can show memory networks noninvasively and reliably and also the effect of surgery on these networks. Anatomic localization of memory-related networks as well as LIs has been applied to study the effects of epilepsy and epilepsy surgery on memory, as discussed later.
Autobiographical memory-related networks
This network, including the hippocampus, medial prefrontal cortex, temporal poles, retrosplenial and lateral parietal cortex, shows reduced activation in patients with left HS and transient epileptic amnesia. The connectivity of a sclerosed left hippocampus is reduced, whereas connections between extrahippocampal nodes are increased. In patients with transient epileptic amnesia, there is reduced activation of the right hemisphere, more specifically of the posterior parahippocampal gyrus, temporoparietal junction, and the cerebellum, for midlife and recent memories. In addition, there is reduced effective connectivity between the right posterior parahippocampal gyrus and the right middle temporal gyrus. These findings suggest that there is functional reorganization and connectivity of the neural network supporting AM retrieval in patients with TLE and transient epileptic amnesia.
Episodic memory-related networks
Verbal memory encoding recruits a bilateral network, including parietal, temporal, and frontal cortices, lateralized to the hemisphere contralateral to the epileptic focus, in patients with TLE. Greater left hippocampal activation for word encoding is correlated with better verbal memory in patients with left TLE. Frontal lobe involvement is more bilateral in left TLE and lateralized in right TLE. Also, greater fMRI activation in the contralateral hippocampus is correlated with worse memory performance, suggesting that reorganization of memory to the healthy medial temporal lobe is an inefficient process.
Visual memory encoding recruits a more widespread bilateral cortical network, also lateralized to the hemisphere contralateral to the epileptic focus in patients with right HS. Lateralization of visual memory encoding to the contralateral hemisphere is associated with decreased and increased verbal memory performance in patients with left and right TLE, respectively. Greater right hippocampal activation for face encoding is correlated with better visual memory in patients with right TLE. Functional connectivity is reduced between the posterior cingulate and the epileptogenic hippocampus and increased between the posterior cingulate and the contralateral hippocampus. Functional reorganization of networks involving extratemporal (orbitofrontal cortex, anterior cingulum [left TLE] and insula [right TLE]), and temporal structures (parahippocampus and fusiform gyrus) for verbal, visual and nonmaterial specific memory encoding suggests compensatory mechanisms to mitigate the failure of the sclerosed hippocampus.
Verbal and visual memory immediate recall shows less activation in patients with HS compared with controls. Patients tend to use the opposite hippocampus and parahippocampal gyrus on the same side, suggesting adaptation or functional reorganization.
Working memory-related networks
Working memory is also affected in patients with TLE with HS, showing variable connectivity between brain regions. Stronger functional connectivity between superior parietal lobe (BOLD activation) and sclerosed hippocampus (BOLD deactivation) is associated with worse performance, suggesting that the segregation of the task-positive and task-negative functional networks is disrupted, resulting in working memory dysfunction in TLE. There is reduced right superior parietal lobe activity; and hippocampal activity from the healthy hippocampus is progressively suppressed as the working memory load increases with maintenance of good performance in patients with TLE. Patients with FLE recruit more widely distributed networks for memory encoding compared with controls, particularly the frontal lobe contralateral to the seizure focus, which is associated with performance, suggesting a compensatory response of brain. Moreover, pediatric patients with FLE show decreased frontal lobe connectivity, which is associated with cognitive impairment, despite intact fMRI activation pattern for working memory. This decreased frontal lobe connectivity may explain the cognitive problems encountered in children with FLE. A higher number of secondary generalized seizures may induce functional reorganization of working memory–related network (eg, increased activation and reduced functional connectivity of prefrontal cortex), explaining working memory dysfunction in patients with focal epilepsy. In contrast to focal epilepsy, patients with juvenile myoclonic epilepsy (JME) do not show a difference in working memory–related BOLD network compared with controls.
Prognostic value
Verbal memory or visual memory may decline in up to one-third of patients undergoing left or right ATLR, respectively. Preoperative memory performance, age at onset of epilepsy, language lateralization, and asymmetry of activation on fMRI for verbal and visual memory can predict verbal memory decline in left ATLR but are less able to predict visual memory decline in right ATLR. The variability of fMRI BOLD signal in the left hippocampus can predict verbal retention, suggesting that variability in brain signals may reflect functional integrity of the area and can be used as a possible clinical tool to predict memory. Preoperatively, verbal and visual memory depend on the damaged left and right hippocampus respectively, as well as contralateral hippocampus. Greater BOLD activation of the diseased left hippocampus and its connectivity to ipsilateral posterior cingulate leads to stronger verbal memory decline after left ATLR. On the other hand, greater BOLD activation of the diseased right hippocampus is associated with more visual memory decline after right ATLR. Conversely, reduced activation of the medial temporal region ipsilateral to the epileptogenic region is correlated with a favorable memory outcome after surgery.
Postoperative findings
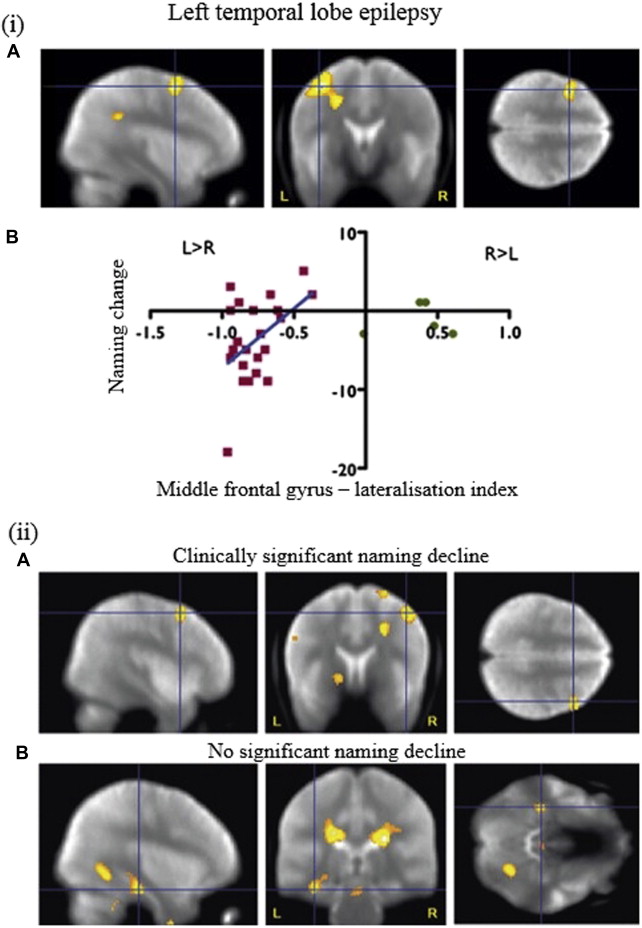
After surgery, patients with left TLE show different pattern of recruitment of frontal lobes for verbal memory encoding. It is suggested that there is effective preoperative reorganization of verbal memory function to the ipsilateral posterior medial temporal lobe as greater preoperative than postoperative activation of this area for word encoding is correlated with better verbal memory outcome after left ATLR, and postoperative reorganization is ineffective ( Fig. 2 ). Others have suggested that postoperative visual and verbal memory performance is positively associated with the activation of contralateral medial temporal lobe and its connectivity to posterior cingulate cortex ipsilateral to the sclerosed hippocampus after temporal lobe resection.
Simultaneous Electroencephalography-Functional Magnetic Resonance Imaging in Epilepsy
Scalp electroencephalography-functional magnetic resonance imaging
Interictal scalp EEG-fMRI can map IED-related BOLD changes but has low sensitivity (30%–40%) because of the dependence on scalp EEG to identify IED and suboptimal modeling of the fMRI signal. The sensitivity can be improved by explaining more variance in the fMRI signal or using topographic map correlation between EEGs recorded outside and inside the scanner. It shows reproducible IED-related BOLD maps, providing more specific localization of the epileptic focus, which may help plan the implantation of intracranial electrodes. The potential clinical value lies in its ability to corroborate negative evidence regarding surgical candidacy, suggesting poor postsurgical outcome, or to suggest reconsideration of surgery after previous rejection as surgical candidates.
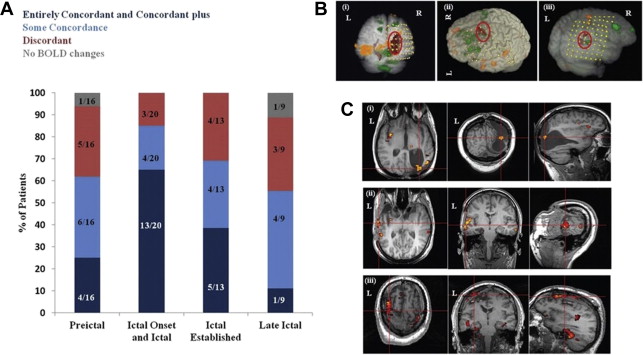
Scalp EEG-fMRI can also map seizure-related BOLD networks during and before seizures. Seizures were captured either by chance during interictal studies or intentionally. The technique can localize the epileptic focus at sublobar level (better than scalp EEG) in ∼85% of cases ( Fig. 3 ), and can separate seizure onset–related BOLD changes from propagation-related BOLD changes. Scalp EEG-fMRI studies are constrained because seizures are unpredictable in nature and seizure-related motion can affect data quality adversely. Focal or widespread BOLD changes have also been shown before the onset of IED or seizure on scalp EEG, highlighting the low sensitivity of scalp EEG and suggesting that hemodynamic changes start before the seizure onset on scalp EEG. The localization of the seizure focus and IED-related BOLD network provided by scalp EEG-fMRI can be used during presurgical assessment. However, larger studies are required comparing the localization provided by scalp EEG-fMRI with postsurgical outcome.
EEG-fMRI studies have played an important role in evolving the debate from zones to networks. It has strengthened the evidence for the existence of corticosubcortical networks associated with generalized spike wave discharges (GSWDs) in idiopathic generalized epilepsy (IGE), involving BOLD increases in the thalamus and widespread BOLD decreases in medial and lateral frontal, superior parietal, posterior cingulate, precuneus and caudate, and posterior brainstem. It has highlighted the role of the default mode network in maintaining awareness in generalized and focal epilepsy, because BOLD networks for attention and working memory are altered by the presence of GSWDs during the task performance. It is possible that precuneus (part of the default mode network) may facilitate the occurrence of GSWDs, consistent with the cortical focus theory of initiation of absences. BOLD changes in propagation-related networks in refractory focal seizures, visual attention network in children with photoparoxysmal response, musicogenic network in musicogenic seizures, reading epilepsy-related network, and motor network in epilepsia partialis continua of the hand have been shown using scalp EEG-fMRI. Scalp EEG-fMRI has shown different GSWD-related BOLD patterns for patients who are refractory or responsive to valproate treatment, and a common area (ie, frontal piriform cortex), ipsilateral to the epileptic focus, has been shown for different types of IED. These findings may be helpful in designing new strategies of treatment of focal epilepsy.
It is unclear as yet how the different nodes of interictal and ictal BOLD networks contribute to the epileptogenicity in a particular patient with focal epilepsy. It is possible that 1 node of the network acts as a principal node, removal of which results in seizure freedom. In contrast, in patients who continue to have seizures after surgery, a second node in the widespread epileptic BOLD network becomes epileptogenic.
Intracranial electroencephalography-functional magnetic resonance imaging
Simultaneous recording of intracranial EEG-fMRI has been made possible after extensive feasibility and safety studies. Significant IED-related BOLD changes have been seen both close to and remote from the most active intracranial electrode, and it has also been suggested that concordance of IED-related BOLD maps, shown by intracranial EEG-fMRI, with the epileptic focus may explain postsurgical outcome better in patients who become seizure free compared with patients who continue having seizures after surgery. Intracranial EEG-fMR imaging has higher electrophysiologic sensitivity and regional specificity and can help to understand the coupling between neurophysiologic and BOLD signal.
Applications of functional magnetic resonance imaging in epilepsy
The life time prevalence of epilepsy ranges from 2.7 to 12.4 per 1000 in western countries. Around 30% of patients with epilepsy remain refractory to antiepileptic drugs and continue to have seizures. Over the last decade, non-invasive imaging techniques such as functional magnetic resonance imaging (fMRI) and diffusion tensor imaging (DTI) have helped to better understand mechanisms of seizure generation and propagation, and to localize epileptic, eloquent and cognitive networks. This review considers the clinical applications of fMRI and DTI, for mapping cognitive and epileptic networks and organization of white matter tracts in individuals with epilepsy.
Increased neuronal activity secondary to a task performance causes variations in the cerebral blood flow, blood volume, and blood oxygenation. This situation results in changes in the ratio of oxyhemoglobin and deoxyhemoglobin concentrations in brain, which is detected as blood-oxygen-level-dependent (BOLD) effect by functional magnetic resonance imaging (fMRI) in specific brain areas that are recruited during the task. Therefore, fMRI provides an indirect measure of neuronal activity. Functional MR imaging has been used to map language and memory networks before and after surgery with high spatial resolution. Simultaneous recording of electroencephalography (EEG) and fMRI can map BOLD networks associated with interictal epileptiform discharges (IED) and seizures in focal and generalized epilepsy.
Language-Related Blood-Oxygen-Level-Dependent Networks in Epilepsy
fMRI can map language networks in patients with refractory epilepsy undergoing epilepsy surgery for research and clinical purposes. Various language paradigms to activate anterior (Broca area: expressive language) and posterior (Wernicke area: comprehension; anterior temporal lobe: semantic integration) language areas have been used to lateralize typical and atypical language representation. Verbal fluency, verb generation, and semantic decision tasks are commonly used tasks for language evaluation in a clinical context, providing complementary information. Verb generation causes more discrete activation, whereas verbal fluency activates language-related areas that are not found with the former. Language lateralization via fMRI has been compared with neuropsychological evaluation, cortical stimulation, or Wada test. Real-time fMRI analysis can improve the processing speed of fMRI data analysis and has good concordance of language localization with conventional general linear model–based analysis or cortical stimulation.
Statistical threshold
Lateralization index (LI) is calculated to detect hemispheric dominance for language networks on fMRI maps, comparing activations in the left and right hemispheres. Choice of details (eg, selecting whole brain or prespecified regions or excluding midline structures for calculating LI) may affect lateralization. Choosing appropriate statistical thresholds is an important issue when evaluating language dominance using fMRI, because the extent and thus localization of fMRI activation depends on the former. Conventional threshold, adaptive threshold, and bootstrap techniques have been used to assess the laterality of language-related fMRI maps. The bootstrap technique is particularly advantageous in that it is more specific and accurately identifies outliers. To avoid dependence of language lateralization on arbitrarily selected statistical thresholds and LI, threshold-independent scores have been used and compared with the Wada test, providing language lateralization at individual level. Data-driven approaches have been used to localize language networks in patients with focal epilepsy and have shown significant differences in language organization, as an effect of epilepsy, which were not seen previously with conventional fMRI analysis. Pattern classifying algorithms have also been used to classify language-related fMRI maps automatically, corroborating with existing LI and visual rating classification methods. For most purposes, comparing left and right activations using the bootstrap method is most satisfactory.
Localization of language networks
Patients with left hemisphere or left temporal lobe epilepsy (TLE) have a higher likelihood of atypical language lateralization than patients with an epileptic focus in the right hemisphere or right temporal lobe. Patients with left TLE with hippocampal sclerosis (HS) and left language dominance have increased recruitment of homologous right hemisphere in addition to left hemisphere language areas for language processing, suggesting widespread language representation and greater cognitive effort performed compared with controls. There is an increase and posterior shift of language-related activation in the right inferior frontal gyrus (IFG) after left hemisphere injury. However, activations in left IFG remain in the same location. Compared with patients with frontal lobe epilepsy (FLE), patients with TLE have more atypical language in the Wernicke area, whereas a frontal focus affects anterior language areas more. In comparison, patients with nonlesional TLE and right TLE show left lateralized language. There is coupling between functional and structural measures for left language lateralization in the patients with right TLE, and decoupling between the functional and structural indices of the patients with left TLE, suggesting complex language networks in left TLE. Language areas activated for abstract and concrete words are also different for patients with TLE, with or without HS, suggesting that HS is associated with altered functional organization of cortical networks involved in lexical and semantic processing. Atypical language representation may also occur in patients with normal structural MR imaging, mesial temporal sclerosis, focal cortical lesions, and stroke.
Language lateralization deduced from fMRI concurs with the Wada test in 80% to 90% of patients when using conjunction analysis of 3 language paradigms or semantic decision paradigm, suggesting the clinical usefulness of the test. Concordance between fMRI and Wada test is the highest for patients with right TLE with left language dominance and for frontal language areas; and the lowest for patients with left TLE with left language dominance. Atypical language dominance on fMRI and interhemispheric language dissociation are correlated with Wada/fMRI discordance. This finding suggests that fMRI may be more sensitive than Wada or cortical stimulation to map the whole network involved in language processing but is less specific at individual level compared with cortical stimulation. fMRI language localization can replace Wada test in most patients. However, Wada test may still be required when a patient cannot perform the fMRI task, for example, because of having a pacemaker or suffering claustrophobia, for validation of atypical language representation on fMRI or for the evaluation of selective language areas near structural abnormalities.
Also, functional connectivity is reduced and reorganized in patients with TLE or intractable epilepsy within the language network. More specifically, functional connectivity is decreased in the left hemisphere irrespective of the epileptogenic focus and frontotemporal network, which is associated with impaired performance on language assessment. Performance on language tasks is also correlated to networks in posterior temporal regions showing increased functional connectivity for both patients with left and right medial TLE.
Language lateralization decreases, and reorganization in frontal, temporal and parietal language networks increases, with earlier age of seizure onset but is not associated with type and location of lesion (acquired or developmental), symptoms, and gender. However, others have not found any association between language lateralization and age of seizure onset but have found an association between language lateralization and handedness, location and nature of pathologic substrate, and duration of epilepsy. Verbal memory performance on neuropsychological evaluation is also found to be associated with language lateralization, suggesting a link between inferior frontal cortex and hippocampus. Gray matter in language networks increases in the hemisphere contralateral to the epileptic focus, and recruitment of the contralateral hemisphere in language processing in patients with atypical language representation may suggest compensatory reorganization mechanisms.
A relative decrease in cerebral blood flow in the left Wernicke area is correlated with decreased activation in the left IFG and LI, suggesting distributed but interconnected language networks. γ Activity in higher frequency range increases and is positively correlated with BOLD responses in the inferior frontal and middle temporal gyri. This γ activity lasts longer in the frontal lobe and declines quickly in the temporal lobe, which may explain difficulties in detecting BOLD in the temporal lobe.
Language fMRI activations of polymicrogyric cortex over Broca area suggest that it retains functionality, and surgical resection should be considered with caution. In patients with generalized epilepsy, fMRI has shown that language function is impaired, as represented by reduced suppression of the default mode network, an inadequate suppression of activation in the left anterior temporal lobe and the posterior cingulate cortex, and an aberrant activation in the right hippocampal formation. Children with benign epilepsy with centrotemporal spikes (BECTS) and other epilepsy types also show bihemispheric language networks, which may represent a compensatory response for ongoing epileptic activity in brain. Also, anterior language networks are affected more in BECTS, resulting in language difficulties for functions dependent on the integrity of anterior language regions (eg, sentence production).
Prognostic value
Language mapping using fMRI is more accurate than Wada test in predicting naming postoperatively. Activation in the left hippocampus during verbal fluency task, in patients with right TLE, is associated with preserved naming function. In contrast, patients with left TLE, who are more proficient in naming, involve left frontal lobe, suggesting compensatory responses caused by ongoing epileptic activity in the left hippocampus. Preoperative language fMRI activation with verbal fluency in the left middle frontal gyrus (MFG) can be used to predict significant naming decline in patients with left TLE, with good sensitivity but suboptimal specificity ( Fig. 1 ). Auditory and visual naming paradigms may give more specific prediction of naming difficulties after anterior temporal lobe resection (ATLR).
Postoperative findings
In postoperative patients with left TLE with left hemispheric language dominance, language representation is more bihemispheric than in controls and patients with right TLE, suggesting that redistribution of language to temporofrontal and interhemispheric areas represent reorganization of language function. Postoperative activation in the right MFG and remaining left posterior hippocampus was correlated with better naming for patients with and without significant naming decline, respectively, again suggesting reorganization in language networks after surgery (see Fig. 1 ). Proficient reading skills after left ATLR depend on integration between normal systems involving the left middle temporal, right hippocampus, and anterior superior temporal sulcus, and recruitment of the right IFG, which is not activated in controls.
Effect of epileptic activity and antiepileptic drugs
Antiepileptic drugs can affect cognitive processing. Topiramate has an effect on activation in the basal ganglia, anterior cingulated, and posterior visual cortex and can cause reduced deactivation of the default mode network-related areas during a language task, suggesting interference in cognitive processing. There has also been some evidence suggesting that atypical language reorganization/dominance may be affected by the presence and absence of ongoing epileptic activity. Chronic frequent interictal epileptic activity in left temporal lobes may be associated with a left-right shift of language representation. Also, atypical language lateralization in the right hemisphere may shift back to the left hemisphere in seizure-free patients after left selective amygdalohippocampectomy.
Memory-Related Blood-Oxygen-Level-Dependent Networks in Epilepsy
Memory impairment is common in patients with epilepsy. Working and long-term memory (autobiographical memory [AM], verbal, visual memory) may become affected, in a material-specific way, based on the site of lesion in TLE and FLE. Functional imaging can show memory networks noninvasively and reliably and also the effect of surgery on these networks. Anatomic localization of memory-related networks as well as LIs has been applied to study the effects of epilepsy and epilepsy surgery on memory, as discussed later.
Autobiographical memory-related networks
This network, including the hippocampus, medial prefrontal cortex, temporal poles, retrosplenial and lateral parietal cortex, shows reduced activation in patients with left HS and transient epileptic amnesia. The connectivity of a sclerosed left hippocampus is reduced, whereas connections between extrahippocampal nodes are increased. In patients with transient epileptic amnesia, there is reduced activation of the right hemisphere, more specifically of the posterior parahippocampal gyrus, temporoparietal junction, and the cerebellum, for midlife and recent memories. In addition, there is reduced effective connectivity between the right posterior parahippocampal gyrus and the right middle temporal gyrus. These findings suggest that there is functional reorganization and connectivity of the neural network supporting AM retrieval in patients with TLE and transient epileptic amnesia.
Episodic memory-related networks
Verbal memory encoding recruits a bilateral network, including parietal, temporal, and frontal cortices, lateralized to the hemisphere contralateral to the epileptic focus, in patients with TLE. Greater left hippocampal activation for word encoding is correlated with better verbal memory in patients with left TLE. Frontal lobe involvement is more bilateral in left TLE and lateralized in right TLE. Also, greater fMRI activation in the contralateral hippocampus is correlated with worse memory performance, suggesting that reorganization of memory to the healthy medial temporal lobe is an inefficient process.
Visual memory encoding recruits a more widespread bilateral cortical network, also lateralized to the hemisphere contralateral to the epileptic focus in patients with right HS. Lateralization of visual memory encoding to the contralateral hemisphere is associated with decreased and increased verbal memory performance in patients with left and right TLE, respectively. Greater right hippocampal activation for face encoding is correlated with better visual memory in patients with right TLE. Functional connectivity is reduced between the posterior cingulate and the epileptogenic hippocampus and increased between the posterior cingulate and the contralateral hippocampus. Functional reorganization of networks involving extratemporal (orbitofrontal cortex, anterior cingulum [left TLE] and insula [right TLE]), and temporal structures (parahippocampus and fusiform gyrus) for verbal, visual and nonmaterial specific memory encoding suggests compensatory mechanisms to mitigate the failure of the sclerosed hippocampus.
Verbal and visual memory immediate recall shows less activation in patients with HS compared with controls. Patients tend to use the opposite hippocampus and parahippocampal gyrus on the same side, suggesting adaptation or functional reorganization.
Working memory-related networks
Working memory is also affected in patients with TLE with HS, showing variable connectivity between brain regions. Stronger functional connectivity between superior parietal lobe (BOLD activation) and sclerosed hippocampus (BOLD deactivation) is associated with worse performance, suggesting that the segregation of the task-positive and task-negative functional networks is disrupted, resulting in working memory dysfunction in TLE. There is reduced right superior parietal lobe activity; and hippocampal activity from the healthy hippocampus is progressively suppressed as the working memory load increases with maintenance of good performance in patients with TLE. Patients with FLE recruit more widely distributed networks for memory encoding compared with controls, particularly the frontal lobe contralateral to the seizure focus, which is associated with performance, suggesting a compensatory response of brain. Moreover, pediatric patients with FLE show decreased frontal lobe connectivity, which is associated with cognitive impairment, despite intact fMRI activation pattern for working memory. This decreased frontal lobe connectivity may explain the cognitive problems encountered in children with FLE. A higher number of secondary generalized seizures may induce functional reorganization of working memory–related network (eg, increased activation and reduced functional connectivity of prefrontal cortex), explaining working memory dysfunction in patients with focal epilepsy. In contrast to focal epilepsy, patients with juvenile myoclonic epilepsy (JME) do not show a difference in working memory–related BOLD network compared with controls.
Prognostic value
Verbal memory or visual memory may decline in up to one-third of patients undergoing left or right ATLR, respectively. Preoperative memory performance, age at onset of epilepsy, language lateralization, and asymmetry of activation on fMRI for verbal and visual memory can predict verbal memory decline in left ATLR but are less able to predict visual memory decline in right ATLR. The variability of fMRI BOLD signal in the left hippocampus can predict verbal retention, suggesting that variability in brain signals may reflect functional integrity of the area and can be used as a possible clinical tool to predict memory. Preoperatively, verbal and visual memory depend on the damaged left and right hippocampus respectively, as well as contralateral hippocampus. Greater BOLD activation of the diseased left hippocampus and its connectivity to ipsilateral posterior cingulate leads to stronger verbal memory decline after left ATLR. On the other hand, greater BOLD activation of the diseased right hippocampus is associated with more visual memory decline after right ATLR. Conversely, reduced activation of the medial temporal region ipsilateral to the epileptogenic region is correlated with a favorable memory outcome after surgery.
Postoperative findings
After surgery, patients with left TLE show different pattern of recruitment of frontal lobes for verbal memory encoding. It is suggested that there is effective preoperative reorganization of verbal memory function to the ipsilateral posterior medial temporal lobe as greater preoperative than postoperative activation of this area for word encoding is correlated with better verbal memory outcome after left ATLR, and postoperative reorganization is ineffective ( Fig. 2 ). Others have suggested that postoperative visual and verbal memory performance is positively associated with the activation of contralateral medial temporal lobe and its connectivity to posterior cingulate cortex ipsilateral to the sclerosed hippocampus after temporal lobe resection.
Simultaneous Electroencephalography-Functional Magnetic Resonance Imaging in Epilepsy
Scalp electroencephalography-functional magnetic resonance imaging
Interictal scalp EEG-fMRI can map IED-related BOLD changes but has low sensitivity (30%–40%) because of the dependence on scalp EEG to identify IED and suboptimal modeling of the fMRI signal. The sensitivity can be improved by explaining more variance in the fMRI signal or using topographic map correlation between EEGs recorded outside and inside the scanner. It shows reproducible IED-related BOLD maps, providing more specific localization of the epileptic focus, which may help plan the implantation of intracranial electrodes. The potential clinical value lies in its ability to corroborate negative evidence regarding surgical candidacy, suggesting poor postsurgical outcome, or to suggest reconsideration of surgery after previous rejection as surgical candidates.
Scalp EEG-fMRI can also map seizure-related BOLD networks during and before seizures. Seizures were captured either by chance during interictal studies or intentionally. The technique can localize the epileptic focus at sublobar level (better than scalp EEG) in ∼85% of cases ( Fig. 3 ), and can separate seizure onset–related BOLD changes from propagation-related BOLD changes. Scalp EEG-fMRI studies are constrained because seizures are unpredictable in nature and seizure-related motion can affect data quality adversely. Focal or widespread BOLD changes have also been shown before the onset of IED or seizure on scalp EEG, highlighting the low sensitivity of scalp EEG and suggesting that hemodynamic changes start before the seizure onset on scalp EEG. The localization of the seizure focus and IED-related BOLD network provided by scalp EEG-fMRI can be used during presurgical assessment. However, larger studies are required comparing the localization provided by scalp EEG-fMRI with postsurgical outcome.