Artifacts and Normal Variants in FDG PET
Paul Shreve
Chuong Dac Huy Bui
Advances in positron emission tomography (PET) capability and widespread recognition of the value of fluorodeoxyglucose (FDG) PET in oncology and has led to the routine whole-body (CF torso) imaging in most oncologic indications of FDG PET. The high FDG uptake by most malignancies relative to the level of FDG distributed throughout much of the body facilitates identification of malignant neoplasm. Compared to conventional anatomic approaches alone, whole-body FDG PET permits much more rapid and accurate identification of the presence and extent of malignant disease. Focal FDG tracer accumulation due to cancer, however, must be distinguished from normal, normal variant, and benign pathological sources of FDG uptake. This is a principal task in the interpretation of whole-body FDG PET scans applied to oncologic diagnosis.
FDG tracer uptake depicts tissue glucose metabolism. Hence, in addition to the abnormal glucose metabolism associated with malignant neoplasm, both normal variations in glucose metabolism and increased glucose metabolism due to a variety of pathologies are revealed on FDG PET. Interpretation of whole-body FDG PET thus requires knowledge of normal and normal-variant patterns of FDG uptake as well as familiarity with the many benign pathologic causes of increased FDG uptake. Frequently both anatomic and physiologic knowledge is needed to reliably identify sites of FDG uptake as normal, variant, or benign pathological etiologies.
Normal Whole-body Fluorodeoxyglucose Distribution
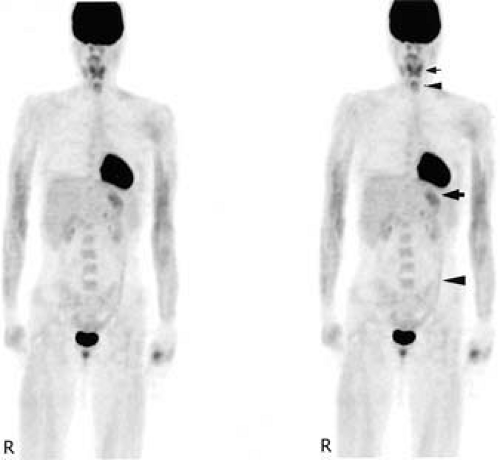
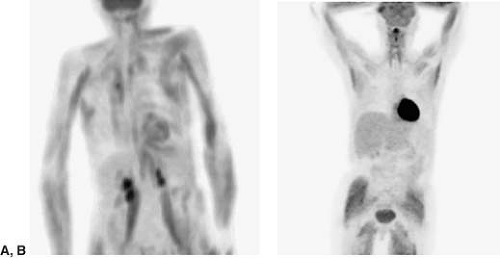
On whole-body PET performed between 1 and 2 hours following intravenous administration of FDG, the brain, heart, and urinary tract are the most prominent sites of tracer accumulation (Fig. 8.3.1). The brain, an obligate user of glucose, is always prominent relative to the rest of the body. Both supratentorial and infratentorial gray matter are FDG avid, and the level of FDG uptake is in the range typical of FDG-avid malignancies. The myocardium is of similar FDG avidity in the fed state, but with sufficiently long fast (typically greater than 12 hours), the myocardium metabolism shifts to fatty acids as a source of energy, and the myocardial uptake becomes largely indistinguishable from blood pool tracer activity. FDG follows a urinary excretory route, hence in the absence of aggressive hydration, diuretics, and urinary bladder catheterization, FDG is present in the bladder and to varying degrees the upper urinary tract.
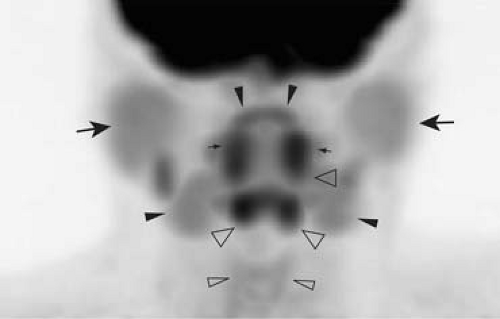
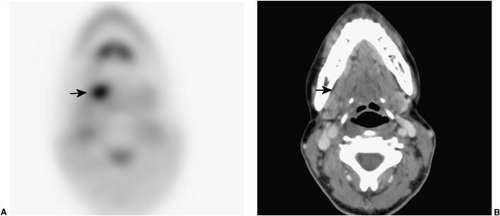
Elsewhere, tracer activity is distributed at low levels in recognizable anatomic structures on attenuation-corrected images (Fig. 8.3.1). Cardiac and mediastinal great vessel blood pool is discernable against the very low tracer activity of the lungs (Fig. 8.3.2). Glandular tissue of the breast is associated with low-level uptake, slightly greater than blood pool, in younger women. The liver and spleen are associated with slightly higher FDG activity than blood pool levels and are reliably identified in the abdomen, as are the kidneys. The pancreas is normally not discretely identified. Bowel is seen to varying degrees, as is the stomach due to widely variable levels of FDG uptake in the alimentary tract. Bone marrow normally is associated with FDG accumulation at levels higher than blood pool activity, hence vertebral bodies are reliably identified, as well as in major marrow containing skeletal structures such as the pelvis, hips, and sternum. In the neck lymphoid tissue associated with the palatine tonsils is consistently FDG avid and typically clearly identified (Fig. 8.3.3). The parotid and submandibular salivary glands are discernable by uniform low-level FDG activity. Muscles of vocalization within the larynx, specifically the posterior cricoarytenoid and vocalis muscles, are commonly seen on routine whole-body scans. Musculature at the base of the tongue, just within the lower anterior mandible, is almost always seen. Cervical spinal cord is identifiable with uniform low-level FDG uptake (Fig. 8.3.3).
Normal Variant Fluorodeoxyglucose Distribution
Myocardium
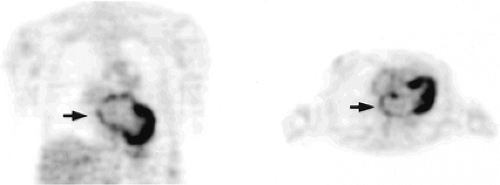
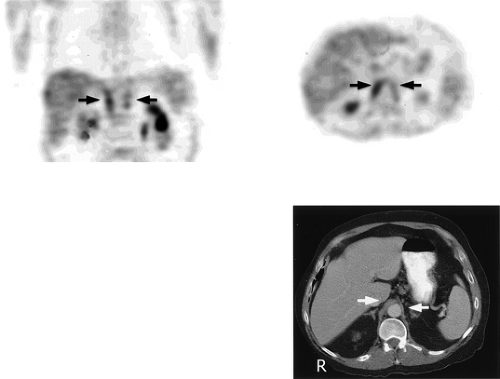
Uptake of FDG in myocardium in patients who have fasted 4 to 18 hours is variable, ranging from uniform and intense, to nearly absent. In the fed state, FDG uptake in intact myocardium is intense, on the order of brain gray matter. With a sufficient fast, myocardium will shift energy metabolism from glucose to fatty acids (1), and demonstrate little FDG uptake; however, in practice, even with overnight fasting, FDG uptake in myocardium is not reliably absent. There is some evidence that an all-protein diet the day before an FDG study enhances the shift of myocardial metabolism to fatty acids. With contemporary dual modality of PET with computed tomography (CT) and image reconstruction algorithms, the presence of intense FDG uptake in the myocardium does not generally present limitations in interpretation of the lungs and mediastinum, except for abnormalities associated with the pericardium or directly adjacent lung. The transition from the intense FDG uptake of dominant glycolytic myocardial metabolism to absent FDG uptake of dominant fatty acid metabolism is frequently nonuniform (Fig. 8.3.4). The base of the left ventricular myocardium tends to be the last portion to lose glucose avidity. Such irregular FDG left ventricular myocardial distribution can be observed in patients who have fasted 4 to 18 hours, yielding apparent discrete foci at the base of the heart that could be misinterpreted as FDG-avid mediastinal lymph nodes if anatomic relationships are not appreciated. In addition, atrial myocardium is sometimes discernable, and again irregular FDG distribution can occur, yielding apparent small focal abnormalities in the mediastinum (Fig. 8.3.5). In the fed state, right ventricular myocardium is typically seen at low levels, but can become as prominent as the left ventricular myocardium in the setting of right ventricular hypertrophy, such as seen with pulmonary hypertension.
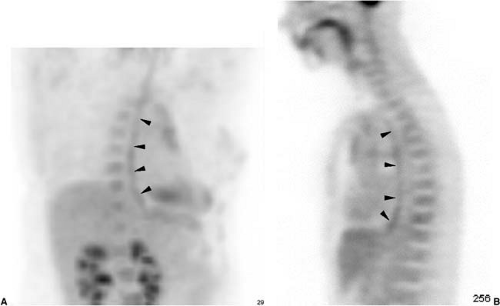
Skeletal Muscle
At rest, skeletal muscle relies on fatty acid oxidative metabolism for energy. With increased energy demand, glycolysis becomes the major source of energy for skeletal muscle depending on relative oxygen delivery and tissue oxidative capacity. Fast twitch muscle fibers, with sparse mitochondria and limited oxidative capacity, are associated with consistent high glucose demand; extraocular muscles routinely demonstrate elevated FDG accumulation (2). Skeletal muscle composed of slow twitch fibers will demonstrate glucose uptake when under active contraction or following glycogen depletion. Hence, skeletal muscle under active contraction during the FDG uptake phase (largely the first 30 minutes after tracer administration) will demonstrate elevated FDG accumulation. Further, skeletal muscle under heavy use prior to injection of FDG may also exhibit FDG uptake, likely related to replenishment of glycogen stores (3). For this reason, patients are typically advised to refrain from heavy exercise the day prior to their FDG PET examination, and following FDG administration, to sit semirecumbent or lie quietly. Since insulin increases muscle uptake of glucose, insulin given prior to, or immediately after, FDG administration will result in diffusely increased muscle uptake (Fig. 8.3.6) (4).
Low-level uptake in the forearm muscles is relatively common (Fig. 8.3.1). Major truncal muscles can be prominent with patients who have been physically active even hours before FDG injection (Fig. 8.3.6). Heavy ventilatory efforts associated with physical exertion or pulmonary disease commonly result in identifiable intercostal muscles and diaphragmatic crura (Fig. 8.3.7) (5). The symmetry and configuration of muscle FDG uptake generally permits correct identification on the FDG PET images alone; however, the FDG uptake does not always involve the entire muscle. Imbalance in muscle groups due to disease or associated treatment such as surgery can result in focal asymmetric FDG uptake, which in certain locations such as the neck, can lead to potential misdiagnosis (6). Asymmetric or isolated major muscle FDG uptake can be confounding in the shoulder girdle musculature. The teres minor is commonly seen when patients are scanned in an arms-by-the-side positioning and should not be confused with metastasis or other pathology in the shoulder region. Identification of the muscle origin of FDG activity is greatly facilitated by review of the registered and aligned images provided on PET/CT acquisitions.
Speech during the uptake phase of FDG increases FDG activity in the laryngeal muscles and the tongue (7). Laryngeal musculature uptake is, in the absence of prior related surgery or unilateral recurrent nerve palsy, nearly always symmetrical and hence readily appreciated as normal. The principal muscles seen are the posterior cricoarytenoid muscles and the vocalis muscles (Fig. 8.3.8). The unilateral absence of FDG activity in the vocalis and cricoarytenoid muscles is a sign of unilateral recurrent laryngeal nerve palsy (Fig. 8.3.9), such as due to tumor mass in the mediastinum or neck.
Tongue uptake varies from mild to intense, typically involves the entire tongue or top of the tongue, and is easily recognizable on maximum intensity projection and sagittal images. Isolated focal uptake can be seen, however. Prior surgery involving the tongue can yield focal asymmetrical muscle uptake, which may be indistinguishable from residual or recurrent malignancy (Fig. 8.3.10). Muscle flaps in the tongue will result in focal tracer uptake indistinguishable from recurrent neoplasm on the FDG PET images. Careful and experienced review of the corresponding CT images (preferably registered and
aligned from a PET/CT scan) and surgical and treatment history is often essential in distinguishing benign from malignant sources of focal FDG tracer activity in the posttreatment neck.
aligned from a PET/CT scan) and surgical and treatment history is often essential in distinguishing benign from malignant sources of focal FDG tracer activity in the posttreatment neck.
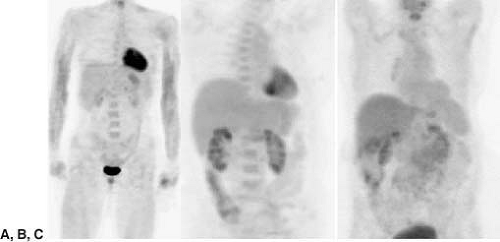
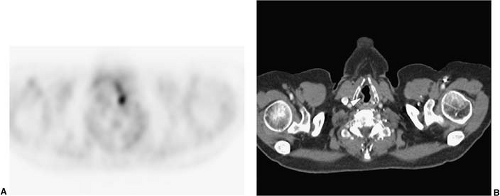
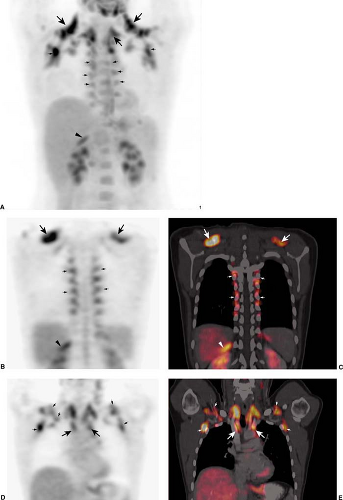
Brown Adipose Tissue
Brown adipose tissue (BAT) is abundantly present in infancy and diminishes with age. BAT expresses a unique mitochondrial uncoupling protein that permits direct heat generation rather than adenosine triphosphate (ATP) production from fatty acid oxidation in response to cold exposure, ingestion of food, or increased sympathetic activity. This process requires an increased supply of ATP, which in turn is provided by an increase in glycolytic metabolism. With routine use of PET/CT, it is now recognized that surprisingly intense increased FDG activity can localize to adipose tissue (most likely BAT) in the neck, supraclavicular regions, axillae, paravertebral locations at the thoracic spine, mediastinum, and occasionally subdiaphragmatic and perinephric fat (Fig. 8.3.11). This phenomenon is seen more often in young patients, females, and slender patients, appears to occur more frequently in the months with colder outdoor temperatures, and is correlated with patient anxiety (8). Activated BAT may also explain increased FDG uptake in lipomatous hypertrophy of interatrial septum. This rare normal variant can mimic malignancy in the mediastinum, but can usually be
correctly identified with PET/CT–generated registered and aligned images. Close attention to controlling the patient’s level of anxiety and the environmental temperature (at least 25°C) for 15 minutes to 2 hours before FDG injection as well as during the FDG uptake phase can significantly reduce FDG uptake in brown fat in the neck and paravertebral area (9,10,11). Drugs such as propranolol and reserpine reduce brown fat uptake by blocking adrenergic receptor–mediated stimulation of BAT (12).
correctly identified with PET/CT–generated registered and aligned images. Close attention to controlling the patient’s level of anxiety and the environmental temperature (at least 25°C) for 15 minutes to 2 hours before FDG injection as well as during the FDG uptake phase can significantly reduce FDG uptake in brown fat in the neck and paravertebral area (9,10,11). Drugs such as propranolol and reserpine reduce brown fat uptake by blocking adrenergic receptor–mediated stimulation of BAT (12).
Alimentry Tract
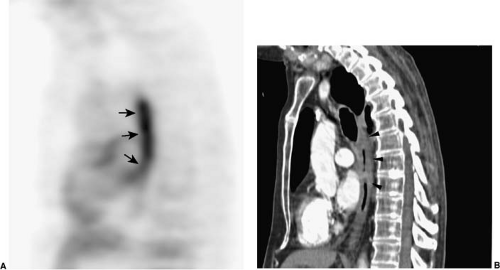
FDG uptake in the alimentary tract, from the esophagus to rectosigmoid colon, is widely variable both in terms of distribution and intensity. The etiology of FDG uptake in the alimentary tract is presently not understood and may reflect different normal and benign pathologic phenomenon in different portions of the alimentary tract. The esophagus occasionally is associated with
low-level activity throughout its extent (Fig. 8.3.12). Relatively intense fusiform and extended FDG uptake occurs in the presence of esophagitis (Fig. 8.3.13), which is indistinguishable from the configurations of esophageal cancer when the cancer has extended along the lymphatic plexus of the esophagus. It should be noted that esophagitis is common and often asymptomatic; hence, FDG uptake in the esophagus, when segmental and even intense, is not specific for esophageal malignancy. A focal area of FDG tracer uptake, especially when seen with focal thickening or asymmetric mass on CT, should be considered suspicious for neoplasm. A small focus of FDG activity is frequently seen at the gastroesophageal junction, probably related to the lower esophageal sphincter, and when no corresponding abnormal thickening or mass on CT is present, generally should not be presumed to be related to malignancy.
low-level activity throughout its extent (Fig. 8.3.12). Relatively intense fusiform and extended FDG uptake occurs in the presence of esophagitis (Fig. 8.3.13), which is indistinguishable from the configurations of esophageal cancer when the cancer has extended along the lymphatic plexus of the esophagus. It should be noted that esophagitis is common and often asymptomatic; hence, FDG uptake in the esophagus, when segmental and even intense, is not specific for esophageal malignancy. A focal area of FDG tracer uptake, especially when seen with focal thickening or asymmetric mass on CT, should be considered suspicious for neoplasm. A small focus of FDG activity is frequently seen at the gastroesophageal junction, probably related to the lower esophageal sphincter, and when no corresponding abnormal thickening or mass on CT is present, generally should not be presumed to be related to malignancy.
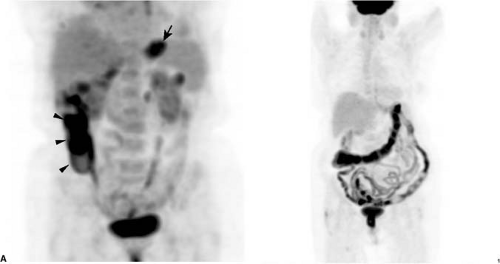
The normal stomach commonly shows FDG uptake, usually somewhat greater than FDG activity in the liver, and readily identifiable based on location and configuration (Fig. 8.3.14A). Gastric FDG uptake can be intense and, if the stomach is contracted, appear as an isolated FDG-avid mass. Location and configuration of the stomach, as well as distribution of FDG uptake in the gastric wall, can be variable, in some instances requiring careful reference to registered and aligned CT images to confirm the gastric origin of the FDG uptake. Gastric lymphoma and gastric carcinoma are thus not reliably diagnosed on FDG PET alone. The propensity for gastric FDG uptake is maintained in hiatal hernias, and hence FDG tracer activity in the lower mediastinum must be correlated with CT images.
Bowel, particularly the right colon (Fig. 8.3.14B), commonly demonstrates FDG uptake. The bowel uptake appears to be in the wall, and may reflect to varying degrees active smooth muscle, metabolically active mucosa, bowel wall lymphoid tissue, swallowed secretions, or colonic microbial activity. Tracer uptake is typically segmental or contiguous in the colon, and the appearance on maximum intensity projection images can be reminiscent of radiographic contrast studies of the colon (Fig. 8.3.14B). Small bowel
FDG activity is usually lower in intensity than FDG activity observed in the colon and is typically seen in the lower pelvis (Fig. 8.3.14B), with continuous or segmental components to its appearance assisting in proper identification.
FDG activity is usually lower in intensity than FDG activity observed in the colon and is typically seen in the lower pelvis (Fig. 8.3.14B), with continuous or segmental components to its appearance assisting in proper identification.
Focality of FDG uptake in either large or small bowel can be confounding, as peritoneal metastatic implants or mesenteric lymph node pathology may be entirely indistinguishable. Careful review of registered and aligned CT images can be essential for assigning isolated focal FDG uptake in the abdomen or pelvis to physiologic bowel tracer activity versus adjacent lymph nodes or serosal implants (Fig. 8.3.15). Focal FDG tracer activity, particularly when more intense than background liver activity within the bowel lumen
adjacent to colon wall, frequently corresponds to pathology, either villous adenomatous polyp or primary colon cancer, requiring further evaluation such as endoscopic examination (13,14). Sometimes a corresponding nodule can be identified on CT, but often no convincing CT abnormality is identified on routine CT, even with contrast enhancement. Inflammatory bowel disease is known to cause diffuse or segmental FDG uptake (15), and the FDG PET appearance tends to be of a featureless tubular structure, analogous to radiographic depictions (Fig. 8.3.16). Characteristic CT signs of inflammatory bowel disease, when present, allow for reliable distinction between benign physiologic FDG tracer uptake and inflammatory bowel disease (Fig. 8.3.16). Non-distended colon can also appear thickened and demonstrate physiologic FDG uptake. Some centers have reported reduction of bowel FDG uptake using smooth muscle relaxants immediately prior to FDG administration (16) or isosmotic bowel preparations the evening prior to the examination (17), although this is not routinely practiced at most centers.
adjacent to colon wall, frequently corresponds to pathology, either villous adenomatous polyp or primary colon cancer, requiring further evaluation such as endoscopic examination (13,14). Sometimes a corresponding nodule can be identified on CT, but often no convincing CT abnormality is identified on routine CT, even with contrast enhancement. Inflammatory bowel disease is known to cause diffuse or segmental FDG uptake (15), and the FDG PET appearance tends to be of a featureless tubular structure, analogous to radiographic depictions (Fig. 8.3.16). Characteristic CT signs of inflammatory bowel disease, when present, allow for reliable distinction between benign physiologic FDG tracer uptake and inflammatory bowel disease (Fig. 8.3.16). Non-distended colon can also appear thickened and demonstrate physiologic FDG uptake. Some centers have reported reduction of bowel FDG uptake using smooth muscle relaxants immediately prior to FDG administration (16) or isosmotic bowel preparations the evening prior to the examination (17), although this is not routinely practiced at most centers.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree