Asbestosis
Helen T. Winer-Muram, MD
Key Facts
Terminology
Interstitial lung disease due to inhalation of asbestos fibers
Imaging Findings
Morphology: Fibrosis centered on respiratory bronchioles
Lung cancer: Lower zone predominance in contrast to upper zone predominance in general population of smokers
Subpleural curvilinear lines early sign
Protocol advice: Prone scans help to differentiate true interstitial lung disease from gravity-related physiology
Top Differential Diagnoses
Idiopathic Pulmonary Fibrosis
Scleroderma
Rheumatoid Arthritis
Hypersensitivity Pneumonitis
Lymphangitic Tumor
Cytotoxic Drug Reaction
Pathology
Fibrosis + asbestos bodies = asbestosis
Retention: Long thin fibers > short thick fibers
Fibrosis associated with > 1 million fibers/g lung tissue
Clinical Issues
Latent period 20-30 years
Does not regress, slowly progresses
In those with asbestosis who smoke, high proportion die of lung cancer (1 in 4)
TERMINOLOGY
Definitions
Asbestosis: Interstitial lung disease due to inhalation of asbestos fibers
IMAGING FINDINGS
General Features
Best diagnostic clue: Basilar interstitial fibrosis and pleural plaques
Patient position/location: Posterobasilar subpleural lung
Morphology: Fibrosis centered on respiratory bronchioles
CT Findings
Morphology
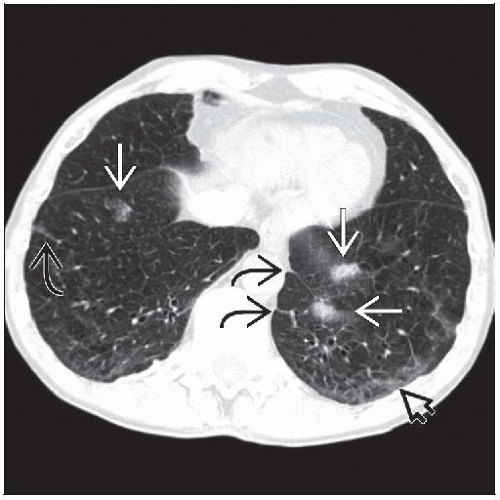
Reticular (linear opacities) most common manifestation
Short intralobular or interlobular septal thickening
Centrilobular nodules or branching opacities earliest manifestation
Reflects fibrosis around small airways where fibers located
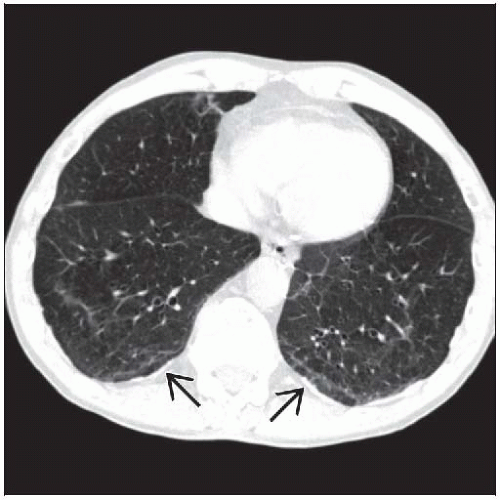
Subpleural curvilinear lines
Parallel chest wall within 1 cm of the pleura, length 5-10 cm
Represent peribronchial confluent fibrosis or atelectasis associated with obstructed respiratory bronchioles
Not specific for asbestosis
Parenchymal bands project perpendicular from pleura
2-5 cm long
Fibrosis along interlobular septa or bronchovascular bundles
Small airways obstruction (from fibrosis incited by asbestos fibers)
May result in mosaic perfusion pattern
Traction bronchiolectasis is uncommon (more common in idiopathic pulmonary fibrosis)
Fibrosis with traction bronchiectasis and honeycombing in advanced disease
Pleural plaques (80%), best finding to differentiate from idiopathic pulmonary fibrosis
Distribution
Peripheral basilar lung most common distribution
Reflects initial location of deposited fibers
Because fibers are too large to be removed by macrophages, fibers tend to reflect initial deposition
Radiographic Findings
Radiography
May be normal (10-20%); pleural plaques (25%)
International Labor Office (ILO) classification compared to standard radiographs “B” reading
Asbestosis generally s, t, or u opacities
Late: End-stage honeycombing; progressive massive fibrosis extremely rare
Lung cancer: Lower zone predominance in contrast to upper zone predominance in general population of smokers
Imaging Recommendations
Best imaging tool
CT useful to differentiate lung nodules from pleural plaques, round atelectasis, and lung fibrosis
10% of asbestos-exposed workers screened by CT for asbestosis will have lung mass
Screening asbestos-exposed workers
Of those with clinical asbestosis: Chest radiographs abnormal in 80%; HRCT abnormal in 96%
33% with neither clinical nor chest radiographic evidence of asbestosis abnormal at HRCT
However, false-negatives for early asbestosis (25%)
Protocol advice: Prone scans help to differentiate true interstitial lung disease from gravity-related physiology
DIFFERENTIAL DIAGNOSIS
Idiopathic Pulmonary Fibrosis
No pleural plaques
Ground-glass opacities and traction bronchiolectasis are more common
Band-like opacities and mosaic pattern of perfusion are less common
Scleroderma
No plaques; however, pleural thickening and pseudoplaques are common
Dilated esophagus
Rheumatoid Arthritis
No plaques; arthritis and joint erosions
Hypersensitivity Pneumonitis
No plaques
Less severe in costophrenic angles, more severe in mid and upper lungs
Mosaic perfusion from air-trapping, more common
Cytotoxic Drug Reaction
No plaques; interstitial thickening similar
Prototypical drug: Methotrexate
Lymphangitic Tumor
No plaques but pleural effusion and lymphadenopathy are common
Asymmetric distribution
Nodular thickening of septa and core bronchovascular structures
PATHOLOGY
General Features
General path comments
Asbestos mineral properties: Heat resistant, high tensile strength, flexible, durable
2 types of fibers: Serpentine and amphibole
Serpentine (chrysotile or white asbestos, 90% commercial asbestos)
Curly, wavy fiber, long (> 100 µm), diameter (20-40 µm)
Amphibole
Crocidolite (blue asbestos), amosite (brown asbestos), anthophyllite, tremolite, actinolite
Straight rigid fiber; length:width = 3:1 is aspect ratio
Retention: Long thin fibers > short thick fibers
Asbestos (ferruginous) bodies
Hemosiderin-coated fiber (mostly amphibole)
Incompletely phagocytized by macrophages
Not pathognomonic for asbestosis
Coated fibers fewer than uncoated fibers
Not correlated with fibrosis
Pathophysiology
Increased deposition of fibers in lower lung zones due to gravitational ventilatory gradient
Fibers deposit in respiratory bronchioles
No lymphatic removal, largest and most harmful asbestos fibers too large to be removed by macrophages
Epidemiology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree