Astrocytic Tumors
Many primary tumors of the central nervous system (CNS) arise from glial cells. The glial cells, in turn, are comprised of astrocytes, oligodendrocytes, and ependymal cells. Astrocytes give rise to a number of tumors which the World Health Organization (WHO) has classified into the following entities:
Pilocytic astrocytoma.
Subependymal giant cell astrocytoma.
Pleomorphic xanthoastrocytoma.
Diffuse astrocytoma (fibrillary, protoplasmic, and gemistocytic).
Anaplastic astrocytoma.
Glioblastoma (giant cell glioblastoma, gliosarcoma).
Gliomatosis cerebri.
Diffuse astrocytoma, anaplastic astrocytoma, and glioblastoma have the same or similar molecular genetics and the basic property of diffusely infiltrating the surrounding CNS tissue. This explains why 50–75% of diffuse astrocytomas progress to anaplastic astrocytoma or even directly to glioblastoma. The timing of this anaplastic transformation is highly variable, however, and the process may take up to 10 years. Molecular genetic studies have identified two different types of glioblastoma: one group that develops secondarily from astrocytomas and another group that forms primarily as glioblastoma. Significant genetic differences have been found between these primary and secondary glioblastomas. Traditionally the subclassification of astrocytic tumors has been based on various grading systems, and the WHO system has become widely established in everyday practice. Although the WHO classification (astrocytoma, anaplastic astrocytoma, and glioblastoma) is actually preferable from a neuropathologic standpoint, the WHO grading system is still universally employed. This is not a problem, however, as there is a direct correlation between the WHO classification and the WHO grades ( ▶ Table 3.3).
WHO classification | WHO grade |
Pilocytic astrocytoma | I |
Diffuse astrocytoma | II |
Anaplastic astrocytoma | III |
Glioblastoma | IV |
3.2.1 Pilocytic Astrocytoma
Pilocytic astrocytomas should be differentiated from diffusely growing astrocytic tumors because they have a different genetic basis, do not infiltrate surrounding brain tissue, and generally do not undergo anaplastic transformation. Additionally, pilocytic astrocytomas have certain sites of predilection that are not shared by other astrocytic neoplasms.
Epidemiology Pilocytic astrocytomas are the most common gliomas in children. Most of these tumors are diagnosed in the first two decades of life, and both sexes are affected equally. Sites of predilection for pilocytic astrocytoma are the optic nerve (optic nerve glioma), optic chiasm, hypothalamus, and cerebellum. The cerebellar hemispheres and brainstem are less commonly affected, and spinal cord involvement is rare.
Clinical manifestations and treatment Because the tumors grow relatively slowly, they cause either direct focal neurologic deficits or secondary signs of increased intracranial pressure, i.e., compression of cerebrospinal fluid (CSF) pathways leading to obstructive hydrocephalus. Seizures are rare because the lesions usually do not involve the cortex. Given their relatively slow growth rate, there is often time for compensatory mechanisms to develop (e.g., little visual disturbance from an optic chiasm tumor). The most common clinical symptoms result from the raised intracranial pressure or functional disturbances in the posterior cranial fossa. The standard treatment is surgery, and recurrence following a complete resection is extremely rare. Tumor remnants are most likely to cause local cyst formation, but rarely the solid tumor component may enlarge. As a general rule, these tumors are relatively stable and slow-growing. A very small percentage may undergo spontaneous regression.
Pathology Macroscopically the tumor tissue is relatively soft and gray in color, with an associated cyst. Rarely, small calcifications or hemosiderin deposits may be found. The solid tumor component is often highly vascularized, and even the cyst wall may show areas of marked neovascularization. Invasion of the subarachnoid space is rarely observed.
MRI findings Most pilocytic astrocytomas are located close to the third and fourth ventricles. Cerebellar pilocytic astrocytomas are generally cystic. The solid nodules show intense, inhomogeneous enhancement after contrast administration ( ▶ Fig. 3.1). Given their frequent infratentorial location, the tumors often compress the fourth ventricle or aqueduct leading to obstructive hydrocephalus ( ▶ p. 374) and, in advanced cases, to the development of periventricular hydrocephalic edema. While most pilocytic astrocytomas are located on the midline, lateral tumor sites may also occur. Pilocytic astrocytomas of the optic chiasm and hypothalamus show intense, homogeneous enhancement but are less likely to have a cystic component. The enhancement itself is more homogeneous than in cerebellar pilocytic astrocytomas ( ▶ Fig. 3.2).

Fig. 3.1 Pilocytic astrocytoma of the cerebellum. (a) Axial contrast-enhanced T1w image demonstrates the solid, laterally situated tumor nodule, which shows intense peripheral enhancement (arrow) around a central necrotic zone. (b) The tumor cyst medial to the nodule is isointense to CSF in T1w and T2w images.

Fig. 3.2 Pilocytic astrocytoma of the optic chiasm. (a) The optic chiasm tumor appears isointense hyperintense (arrow) in the unenhanced coronal T1w image. (b) After contrast administration the tumor shows intense homogeneous enhancement. (c) T2w image demonstrates the hyperintense, somewhat inhomogeneous, tumor matrix.
Differential diagnosis Pilocytic astrocytomas at an infratentorial site and in children mainly require differentiation from medulloblastoma. This is important because the prognosis and postoperative treatment regimen are different for these two entities, but it may be very difficult to distinguish between them in any given case. Generally speaking, medulloblastomas do not have a cystic component and are more likely to show signs of bleeding into the tumor matrix. Also, they often enhance less intensely than pilocytic astrocytomas. The differential diagnosis of large infratentorial lesions should include ependymoma or a primary choroid plexus tumor. Hemangioblastoma is a possible diagnosis for tumors with a large cystic component, but generally this entity shows conspicuous flow voids on MRI due to its angiomalike structure.
3.2.2 Pleomorphic Xanthoastrocytoma
This is a circumscribed, desmoplastic astrocytic neoplasm that most commonly occurs in superficial portions of the cerebral hemispheres in children and young adults. Most of these tumors have a large cystic component.
Note
Pleomorphic xanthoastrocytoma is more sharply circumscribed than other astrocytomas and is less likely to show diffuse spread.
Epidemiology The tumor occurs predominantly in children and young adults. The peak age incidence is between the second and third decades.
Clinical manifestations and treatment Because of their temporal location, these tumors frequently cause temporal lobe seizures. Treatment consists of radical surgical excision. The tumor has a considerably better prognosis than other astrocytic tumors (10-year survival rate >70%).
Pathology The tumor often grows superficially in the cortex. Most pleomorphic xanthoastrocytomas form a relatively large cyst that includes a solid nodule in the cyst wall.
MRI findings The tumor is relatively well delineated on MRI. Its appearance closely resembles that of pilocytic astrocytoma (cyst with an intensely enhancing tumor nodule; ▶ Fig. 3.3).

Fig. 3.3 Pleomorphic xanthoastrocytoma. This tumor exhibits a lobulated cyst in its occipital portion with corresponding fluid signal intensity in T2w and T1w images. Just rostral to the cyst is the solid tumor nodule, which shows intermediate signal intensity in the T2w image (a). Both the septa of the cystic component and the solid nodule show intense enhancement (b,c). The mass effect has caused herniation of the temporal lobe with displacement of the midbrain and congestion of the right temporal horn (a,b).
(a) Axial T2w image. (b) Axial T1w image. (c) Coronal T1w image.
3.2.3 Diffuse Astrocytoma
Astrocytomas are also known as “low-grade astrocytomas” and are classified as grade II gliomas in the WHO classification. Three different histologic types are distinguished:
Fibrillary astrocytomas.
Protoplasmic astrocytomas.
Gemistocytic astrocytomas.
Fibrillary astrocytomas constitute the largest of these groups. Cerebral astrocytomas have the property of growing diffusely in the white matter. The affected anatomic structures are enlarged or displaced but are not destroyed by this type of tumor. These tumors generally grow very slowly but may undergo malignant transformation at any time. Low-grade astrocytomas occur predominantly in the frontal and temporal lobes, less commonly in other brain regions, and only rarely in the basal ganglia. Some of these tumors have a gelatinous consistency, and cysts may form that contain a relatively clear fluid. Brainstem astrocytomas are most commonly located at the center of the pons but may also have exophytic components that encase the basilar artery. Focal calcifications are also seen in rare cases. Neovascularization is usually absent, and tumoral hemorrhage is very rare.
Epidemiology Low-grade astrocytomas are somewhat rare. At most they represent 10 to 15% of all gliomas and, accordingly, are much less common than glioblastomas. Low-grade fibrillary astrocytomas occur predominantly in children and in adults 20 to 40 years of age. These tumors are very rarely found in older adults.
Clinical manifestations and treatment Given their frequent subcortical and cortical location, these tumors usually present with epileptic seizures. Because low-grade astrocytomas have the genetic potential for malignant transformation (50–75%), the treatment of choice for low-grade astrocytomas is surgical removal. This is particularly recommended when a complete tumor resection appears feasible. Malignant transformation to higher-grade gliomas is the most frequent cause of death in patients with low-grade astrocytomas. Mean survival time is approximately 10 years after initial diagnosis.
Pathology Diffuse astrocytomas show only slight cellular atypia on cytologic examination. The ability of glioma cells to invade healthy brain tissue incites various local reactions in the form of astrocytosis and the activation of microglia. Malignant transformation is marked by the occurrence of neovascularization. Although the subcortical U-fibers create a certain natural barrier to the migration of glial cells, diffuse cortical infiltration may still occur.
MRI findings Low-grade astrocytomas typically are slightly hypointense to gray matter on T1w images. These tumors are uniformly hyperintense on T2w images and especially on FLAIR images ( ▶ Fig. 3.4). Perifocal edema is generally absent, so all signal changes conform to actual tumor size. Tumor classification by MRI is relatively simple, as grade II astrocytomas do not enhance after contrast administration. This correlates very well with the histopathologic absence of neovascularity. In the event of malignant transformation (to a grade III or IV glioma), enhancement will be noted on MRI. In rare cases these low-grade astrocytomas may have a cystic or even polycystic appearance. Tumor extent is defined most accurately on FLAIR images (or PDw images). DWI does not show restricted diffusion, which is consistent with the low-grade classification of these tumors. The choline peak is not elevated on MR spectroscopy, and SWI generally does not show susceptibility changes.

Fig. 3.4 WHO grade II astrocytoma. (a) The tumor has infiltrated the brain, causing essentially no mass effect. The entire tumor has high signal intensity in the T2w image, with no evidence of perifocal edema. (b) The tumor is nonenhancing and hypointense in the T1w image.
Differential diagnosis Circumscribed subcortical signal changes basically have a broad differential diagnosis. With very small changes, for example, postinflammatory or posttraumatic gliosis would not be distinguishable from a low-grade astrocytoma. The very rare primary cystic presentation of a low-grade astrocytoma requires differentiation from a neuroepithelial cyst. Larger astrocytomas also require differentiation from subacute infarcts. Differentiation in this case is aided by DWI, because infarcts show restricted diffusion with a decreased apparent diffusion coefficient (ADC) for up to 5 days after the infarction event. A territorial infarct is usually distinguishable from low-grade astrocytoma on T1w images as well, owing to the relatively low T1w signal intensity of low-grade astrocytomas. Doubts can be resolved by spectroscopy (which detects lactate in an infarction) or by repeating the MRI examination in 2 to 4 weeks. By that time an infarct would significantly change its signal characteristics while a low-grade glioma would appear unchanged. Postsurgical changes after a tumor resection may be a source of confusion, as gliosis at the surgical margins may have the same signal characteristics as low-grade astrocytoma.
Tips and Tricks
In patients who have had a tumor resection, only a direct comparison of identical pre- and postoperative images can distinguish between residual tumor and initial scar formation at the surgical margins. In other cases this differentiation must rely on follow-ups. Given the possibility of malignant transformation, contrast should be used for all follow-up scans.
3.2.4 Anaplastic Astrocytoma and Glioblastoma
Anaplastic astrocytoma is classified as a grade III glioma in the WHO classification, and glioblastoma multiforme as a grade IV glioma. Glioblastomas may arise de novo or may result from the malignant transformation of an initially low-grade astrocytoma ( ▶ Fig. 3.5). These two pathways of tumor development can be distinguished only by molecular genetic analysis; they are indistinguishable by gross or histopathologic examination. Glioblastoma multiforme is the most common primary intracranial brain tumor. As the name implies, it is highly variable in its microscopic and macroscopic features.

Fig. 3.5 Anaplastic brainstem astrocytoma. (a) Sagittal T1w image after contrast administration. This large, hypointense pontine tumor in a 7-year-old boy was investigated by stereotactic biopsy: grade III astrocytoma. (b) Despite radiotherapy the tumor progressed within 10 months to glioblastoma, manifested by intense, irregular enhancement.
Epidemiology Glioblastoma multiforme and anaplastic astrocytoma together comprise 65 to 75% of all gliomas. As the grades indicate, anaplastic astrocytoma is a transitional or intermediate form between astrocytoma and glioblastoma multiforme. Glioblastomas have a bimodal age distribution with a main peak occurring after age 50 and a smaller peak before age 30.
Clinical manifestations and treatment The history of these fast-growing tumors is relatively short and usually lasts only a few weeks or months. Initial symptoms consist of focal neurologic deficits, strokelike symptoms, or seizures. More advanced tumors produce a mass effect that may cause secondary obstruction of CSF flow. The standard primary treatment at diagnosis is maximal surgical resection, which is limited by the relationship of the tumor to eloquent brain areas (e.g., speech center, motor cortex). Resection is therefore focused on the neovascularized portion of the tumor, which corresponds to the enhancing components on MRI. Partial tumor resection is followed by radiation and subsequent adjuvant chemotherapy with temozolomide. For circumscribed recurrence, a second operation or, rarely, a third can be performed to reduce the gross tumor mass. Even so, glioblastoma patients have a limited mean survival time that rarely exceeds 12 months after diagnosis. Several studies in recent years have shown that survival time can be significantly lengthened by removing the tumor component that enhanced on MRI. Newer therapies are aimed at limiting glial proliferation or stimulating the immune system by local drug infusions or applications.
Pathology Glioma cells have an active migratory capacity, i.e., they can grow autonomously through the brain tissue along anatomic pathways such as myelin sheaths or basement membranes. Like many other malignant tumors, gliomas synthesize factors that stimulate neovascularization (e.g., vascular endothelial growth factor). Thus, once the tumor has reached a certain size, new pathologic blood vessels are formed. Unlike healthy vessels, however, these tumor vessels have a much weaker barrier with surrounding brain tissue, resulting in edema formation as well as contrast enhancement.
Note
These fundamental properties—migratory capacity and neovascularization—are the histopathologic basis for the imaging appearance of glioblastomas. Nevertheless, glioblastomas can have a variety of appearances as their alternate name (glioblastoma multiforme) suggests.
Three main patterns of tumor growth can be distinguished by their descriptive morphologies:
Primary solid tumor.
Infiltrating pattern.
Central necrosis.
Glioblastoma most commonly occurs in the deep cerebral white matter, predominantly in the frontal or temporal lobes. Its growth is often directed along major fiber tracts. Peritumoral edema is often considered a facilitator of solid tumor growth. The edema disrupts coherent cell groups in the brain tissue, creating new pathways for the migration of glioma cells. Multilobular and bihemispheric tumor spread is found in advanced stages, including spread across the corpus callosum. Glioblastomas rarely occur in the posterior cranial fossa.
MRI findings Glioblastomas have a range of appearances on MRI, consistent with their diverse histopathology, but all glioblastomas enhance after intravenous contrast administration, corresponding to their histologic grades and neovascularity. Contrast-enhanced T1w images typically show a gross tumor mass with scalloped margins and central necrosis surrounded by a distinct fingerlike pattern of white-matter edema ( ▶ Fig. 3.6). Punctate hemorrhages may be found in the tumor matrix. The three main growth patterns of glioblastoma—described above as solid, infiltrating, or with central necrosis ( ▶ Fig. 3.7)—can also be distinguished on MRI. The degree of perifocal edema is highly variable, but histology consistently detects malignant cells within the edema and even beyond its boundaries in some cases. When tumor growth is advanced, nests of new tumor cells can be found at some distance from the core lesion, even within the fingers of peritumoral edema. These cell nests show neovascularity and enhancement on MRI. Glioblastomas may be multifocal or multicentric. Multifocal lesions are interconnected at least by edema, whereas multicentric tumors are separated from one another by normal white matter but arise in synchronous fashion. This may be considered a model for the genetic triggering of tumorigenesis ( ▶ Fig. 3.8). Initially, the subcortical U-fibers create a certain barrier to the migration of glioma cells. This barrier is breached in the advanced stage, however, and tumor cells can invade the subarachnoid space and become disseminated via the CSF. Sheetlike tumor growth may even develop on the brain surface. Pachymeningeal (dural) infiltration is unusual.

Fig. 3.6 Glioblastoma multiforme. (a) T1w image shows a glioblastoma with scalloped rim enhancement and central necrosis. (b) On a T2w image, the tumor core shows a partially distinct and partially ill-defined transition to nonenhancing hyperintense peripheral tumor components and peritumoral edema. The edema is difficult to distinguish from peripheral tumor. (c) Several medial and posterior tumor components have undergone malignant transformation, with associated restriction of diffusion. (d) SWI sequence shows numerous signal voids caused by pathologic tumor vessels and microhemorrhages.

Fig. 3.7 Principal growth patterns of glioblastoma. Diagrammatic representation. (a) Round, solid tumor. (b) Central necrosis. (c) Diffuse infiltration.

Fig. 3.8 Multicentric anaplastic astrocytoma, WHO grade III. MRI shows a characteristic mixed pattern of diffuse tumor infiltration, predominantly affecting the white matter, and individual tumor nodules with associated blood–brain barrier disruption in both frontal lobes. (a) T2w image shows the extent of diffuse low-grade tumor spread, which is confined chiefly to the white matter. (b) Contrast-enhanced T1w image shows a dedifferentiated tumor component with ring enhancement in the left periventricular region. A smaller malignant nodule appears as a focal enhancing lesion in the right frontal lobe.
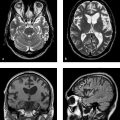
Early postoperative follow-up Today the primary goal of surgical treatment is the radical removal of all gross tumor (i.e., tumor that enhances on MRI). Early postoperative imaging can document this therapeutic goal. Imaging should be performed within the first 3 to 4 postoperative days, however, because the period from 4 days to approximately 3 months is marked by surgically induced enhancement of the resection margins. Blood breakdown products (especially if the resection cavity was irrigated with hydrogen peroxide) can mimic residual tumor on postoperative scans ( ▶ Fig. 3.9). The surgical resection of glioblastoma is usually followed by radiotherapy. Thus, it is important in follow-up to distinguish between recurrent tumor and radiation necrosis (also known as “pseudoprogression”). The latter usually occurs between 4 and 6 months after radiotherapy. Radiation necrosis is characterized by a marked disruption of the blood–brain barrier with significant edema formation and rapid extravasation of contrast medium into the surrounding tissue. Perfusion imaging, spectroscopy, and SWI can help distinguish between recurrent tumor and radiation necrosis. The dominant feature of radiation necrosis is not neovascularization but increased permeability with corresponding perfusion curves (leakage). Spectroscopy shows high lactate and lipid peaks and low choline peaks. Ultimately, however, there are no definite MRI criteria that can reliably differentiate recurrent glioma from radiation necrosis; this can be accomplished only by follow-up imaging. The Response Assessment in Neuro-Oncology (RANO) criteria have become well established for the follow-up of glioblastoma ( ▶ Fig. 3.10). The RANO criteria take into account the phenomena of pseudoprogression and pseudoregression:
Pseudoprogression: appearance of neovascularization in response to radiotherapy and adjuvant chemotherapy, which can mimic true progression.
Pseudoregression: tumor growth with a decreased enhancing component but a tumor-related increase in T2w lesions; occurs after treatment with antiangiogenic agents.
Pitfall
Given the above uncertainties following anticancer therapies, tumor progression should be diagnosed only on the basis of continued follow-ups, aided if necessary by magnetic resonance spectroscopy (MRS) and perfusion MRI.

Fig. 3.9 Early postoperative follow-up of glioblastoma. (a) Axial T1w image after contrast administration. Preoperative view of a tumor with central necrosis and peripheral rim enhancement in the left temporal region. (b) Unenhanced T1w image after surgery. Hyperintensities on the medial rim of the surgical cavity are caused by blood breakdown products. (c) Image after contrast administration demonstrates residual malignant tissue on the rostral rim of the cavity (arrow).

Fig. 3.10 Brain tumor staging based on RANO criteria. Follow-up images in a 37-year-old woman who presented with acute onset of word-finding difficulty, then underwent surgery and postoperative chemoradiation. (a) Preoperative T2w image shows a left frontal cortical tumor measuring approximately 13 mm × 15 mm. (b) Contrast-enhanced T1w image corresponding to (a). Most of the tumor shows contrast enhancement. Slight perifocal edema is also present. (c) Postoperative T2w image 8 days after surgery documents tumor removal (complete response by RANO criteria). Histology identified the lesion as anaplastic astrocytoma. (d) Contrast-enhanced T1w image corresponding to (c). (e) T2w image 14 months after surgery shows (pseudo)progression after chemoradiation with significant new edema in the left hemisphere plus streaky enhancement along the original surgical margins and deep in the white matter. As these changes regressed over time, they were interpreted as postirradiation changes. (f) Contrast-enhanced T1w image corresponding to (e). (g) T2w image 18 months after surgery shows a recurrent tumor measuring approximately 16 mm × 29 mm (progressive disease by RANO criteria). The tumor was identified histologically as glioblastoma multiforme. (h) Contrast-enhanced T1w image corresponding to (g).
The RANO criteria for evaluating tumor response are summarized in ▶ Table 3.4.
Criteria | Complete response | Partial response | Stable disease | Progression |
Enhancing lesions on T1w MRI | None | ≥50% decrease | <50% decrease but <25% increase | ≥25% increase(1) |
FLAIR/T2w lesions | Stable or decreasing | Stable or decreasing | Stable or decreasing | Increase(1) |
New lesions | None | None | None | Any new lesions(1) |
Corticosteroids | None | Stable or reduced | Stable or reduced | NA(2) |
Clinical status | Stable or improved | Stable or improved | Stable or improved | Deterioration(1) |
Necessary criteria | All | All | All | At least one criterion(1) |
NA = not applicable. Source: Radbruch A, Bendszus M. RANO-criteria for high grade glioma. Radiology up2date 2012; 3: 267–269. (1) Progression is present if this criterion is met. (2) Increased steroid dosing alone does not justify classification as “progressive disease” if clinical deterioration is not present. | ||||
Differential diagnosis Higher-grade gliomas require primary differentiation from metastases and lymphomas. Lymphomas in immunocompromised patients generally show intense homogeneous enhancement without necrosis. As a result, SWI sequences demonstrate microhemorrhages in glioblastomas but not in lymphomas. On perfusion imaging, glioblastomas show hypervascularity while lymphomas show increased permeability. Gliomas often show infiltrative features at the periphery of gross tumor growth, which is a helpful differentiating criterion from metastases. Difficulties may arise in identifying gliomas that have undergone primary intratumoral hemorrhage. Differentiation in these cases is aided only by very early MRI, before a methemoglobin signal has appeared. Peripheral enhancement of an apparent primary hemorrhage at this early stage is suspicious for an underlying tumor. The differential diagnosis of glioblastoma also includes atypical infarcts, tumorlike demyelination, and circumscribed infections (bacterial abscess, tuberculoma, or aspergilloma). A well-encapsulated abscess with central viscous pus shows a marked DWI abnormality with high signal intensity. The abscess capsule is hypointense on T2w and PDw images, and perifocal edema is generally very pronounced ( ▶ Fig. 3.11). These aids for distinguishing between glioma and abscess are not 100% reliable but are still helpful in narrowing the differential diagnosis.

Fig. 3.11 Brain abscess. (a) T2w image of an abscess in the right frontal lobe demonstrates a hypointense granulating rim and marked perifocal edema. (b) As expected, the lesion shows intense peripheral enhancement on the postcontrast T1w image. (c) Pus shows characteristic high signal intensity on DWI.
3.2.5 Gliosarcoma
Gliosarcoma is a rare primary brain tumor that arises from a glioma with a mesenchymal component. The latter originates from endothelial, fibroplastic, and myoplastic elements. The tumor consists of a very firm lobulated mass with central necrosis. The highest incidence is in the fifth to seventh decades. Survival rates are similar to those of glioblastoma multiforme. Unlike that tumor, however, gliosarcoma can metastasize to extracranial sites, and 15 to 30% of all gliosarcoma patients have visceral metastases. Gliosarcomas usually have a peripheral location with a tendency to invade the dura. Their MRI appearance is variable. The tumors are inhomogeneous, contain hemorrhagic and necrotic zones, and generally show marked heterogeneous enhancement ( ▶ Fig. 3.12).

Fig. 3.12 Gliosarcoma. (a) T2w image shows a very inhomogeneous mass in the left frontal lobe with a solid nodule and multiple cystic and necrotic components of high signal intensity. Mass effect from the tumor and perifocal white-matter edema have caused transfalcine herniation of the frontal lobe to the right side. (b) Coronal T1w image after contrast administration shows a mixed nodular and peripheral pattern of tumor enhancement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree