- •
Magnetic resonance angiography (MRA) is an excellent imaging modality for defining pulmonary venous anatomy before pulmonary vein isolation for treatment of atrial fibrillation.
- •
Pulmonary vein stenosis, a possible side effect of atrial fibrillation ablation, is associated with dyspnea, cough, or hemoptysis and can be diagnosed with MRA.
- •
Esophageal perforation, another feared complication of catheter ablation for atrial fibrillation, typically presents with dysphagia. Early recognition and treatment is of paramount importance and can be facilitated by cardiac magnetic resonance (CMR) imaging.
- •
Transesophageal echocardiography (TEE) is the current standard of care for ruling out the presence of thrombus in the left atrial appendage before cardioversion or catheter ablation. The noninvasive nature of CMR compared with TEE suggests promise for its future use in thrombus evaluation.
- •
Because of its superior soft tissue resolution, CMR is an ideal tool for diagnosis, staging, and preprocedural planning for treatment of cardiac mass lesions.
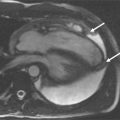
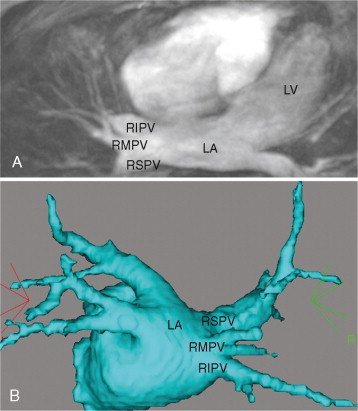
A 65-year-old man with history of highly symptomatic persistent atrial fibrillation refractory to antiarrhythmic therapy presented for pulmonary vein isolation. Preprocedural TEE ruled out the presence of left atrial thrombus. CMR was performed prior to the procedure to plan lesion sets and obtain baseline pulmonary vein diameters ( Figure 6-1 ). The MRA revealed a right middle pulmonary vein.
Comments
Atrial fibrillation is the most common sustained cardiac arrhythmia and is associated with increased morbidity and mortality. The identification of focal pulmonary vein triggers for atrial fibrillation has led to surgical and catheter-based ablation techniques to treat atrial fibrillation through electrical isolation of pulmonary veins from the atria. To guide the intricate lesion sets required for isolation, MRA images of the left atrium and pulmonary veins are often acquired before catheter-based pulmonary vein isolation procedures for atrial fibrillation. Three-dimensional reconstructions of such images can be merged with an electroanatomic mapping system to provide catheter positioning information during the procedure and help guide the targeting of lesions sets. Information about variant anatomic features such as a right middle lobe pulmonary vein can change procedural plans. For example, ablation between the superior and inferior pulmonary veins is commonly performed, may cause occlusion of the right middle branch, and is best avoided in patients with such variant anatomy. Lack of information about such anatomic detail may result in pulmonary vein stenosis or occlusion, often presenting with dyspnea, cough, and/or hemoptysis.
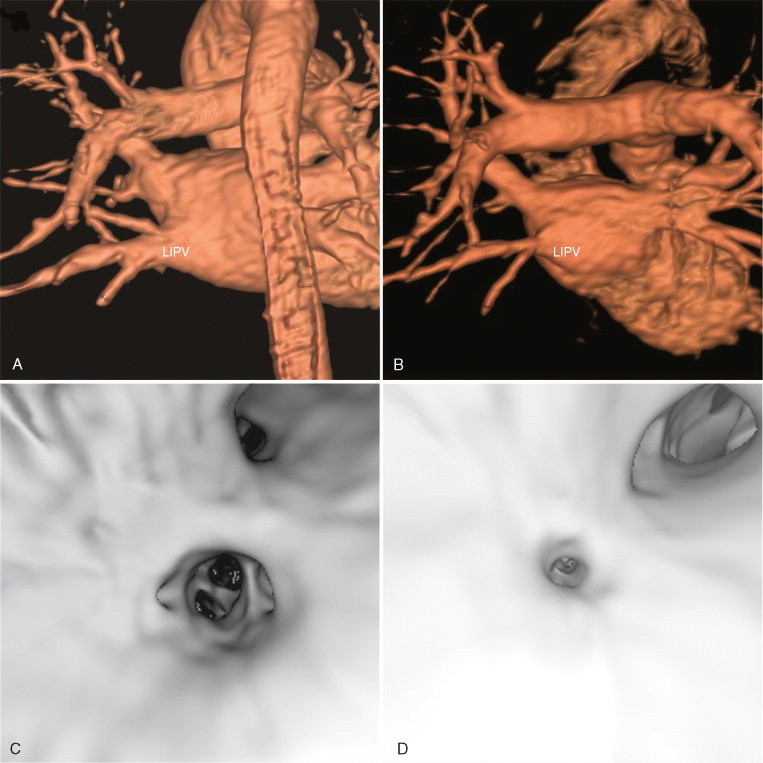
A 39-year-old man with a 3-year history of highly symptomatic paroxysmal atrial fibrillation underwent catheter-directed pulmonary vein isolation using radiofrequency energy. Follow-up CMR images revealed mild narrowing of all pulmonary vein ostia, and occlusion of the superior branch of the left inferior pulmonary vein ( Figure 6-2 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree