32 Axillary Block
Three terminal branches of the brachial plexus (the median, radial, and ulnar nerves) lie close to the axillary artery in the axilla (Table 32-1). This makes the axilla a convenient place to block the brachial plexus (Table 32-2). Axillary block is traditionally performed by transarterial injection of local anesthetic around the axillary artery or by use of nerve stimulation to evoke motor responses. Transarterial block necessitates puncturing the axillary artery. Another weakness is failure to anesthetize the musculocutaneous nerve, which leaves the neurovascular bundle proximally underneath the pectoralis minor muscle at the level of the coracoid process.
Table 32-1 Characteristics of Terminal Branches of the Brachial Plexus in the Axilla
| Nerve | Characteristics |
|---|---|
| Axillary | |
| Musculocutaneous | |
| Radial | |
| Median | |
| Ulnar | |
| Medial antebrachial cutaneous | Lies between median nerve and ulnar nerve |
| Intercostobrachial and medial brachial cutaneous |
Table 32-2 Clinical Considerations for Axillary Block with Ultrasound
| Advantages | Disadvantages |
|---|---|
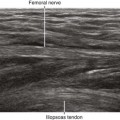
Ultrasound imaging improves axillary block of the brachial plexus. Almost all institutions have reported advantages to using ultrasound to guide this procedure.1,2 Ultrasound can be used to guide injections around the axillary artery. In addition, the musculocutaneous nerve can be directly imaged to complete the axillary block (see Chapter 33).